Introduction
Choanal atresia is a congenital obstruction of the posterior nasal aperture associated with failure of nasal cavity canalisation. Occurring in 1:5000–1:8000 live births,Reference Ramsden, Campisi and Forte1 it is more frequent in females than males. Choanal atresia is bilateral in 40 per cent of cases and unilateral in 60 per cent. Bilateral choanal atresia can be life-threatening in the obligate nasal-breathing neonate unless an airway is secured after birth. Unilateral choanal atresia presents later with persistent unilateral nasal discharge or obstruction.Reference Stankiewicz2 The atretic plate is bony (in approximately 30 per cent) or mixed bony-membranous (in approximately 70 per cent),Reference Brown, Pownell and Manning3 and is bounded by the floor of the sphenoid superiorly, the hard palate inferiorly, a widened vomer medially, and the medialised lateral and medial pterygoid plates laterally.Reference Wormald, Zhao, Valdes, Pacheco, Ha and Tewfik4
Patients with choanal atresia require surgery to fashion a patent choana. Different approaches have been described, including transpalatal and transantral approaches.Reference Park, Brockenbrough and Stankiewicz5 The transnasal endoscopic technique provides better results and is associated with fewer complications.Reference Josephson, Vickery, Giles and Gross6 Post-operative restenosis of the choanae occurs in 11–35 per cent of casesReference Gosepath, Santamaria, Lippert and Mann7 and remains a challenge, with patients requiring an average of 2.7 procedures to achieve sustained patency.Reference Samadi, Shah and Handler8 Choanal stenting and mitomycin C have been proposed for the reduction of restenosis rates, and these methods remain contentious. The use of septal mucosal flaps to resurface the neo-choana at the end of atresia resection has been proposed as key to avoid post-operative stenosis.Reference Stamm and Pignatari9
The present paper describes our endoscopic transnasal cross-over septal flap technique, with discussion of the principles associated with the success rate. Stamm and PignatariReference Stamm and Pignatari9 described a similar technique; the differences are discussed.
Materials and methods
A retrospective observational analysis was adopted in the ENT departments at two teaching hospitals: the Circolo Hospital and Macchi Foundation, University of Insubria, Varese, Italy, and the Korle Bu Teaching Hospital, Accra, Ghana. Databases were evaluated to identify choanal atresia patients undergoing primary surgery in the respective institutions between 2013 and 2020. Neither institution required ethical approval or further patient consent for a retrospective analysis. A total of 12 patients fit the study's eligibility criteria, of which 8 were from Varese and 4 were from Accra.
Technical note
Surgery was performed under general anaesthesia with the patient in a supine reverse Trendelenburg position. The nasal cavities were instilled with 0.05–0.2 per cent oxymetazoline, or 0.5–1 per cent oxybuprocaine and adrenaline (1:100 000–1:200 000) solution, or with neurosurgical pledgets, depending on the patient's age, for 5–10 minutes. Zero-degree endoscopes (Karl Storz, Tuttlingen, Germany) with diameters of 2.7 mm or 4 mm were used. Endoscopic adult and paediatric nasal surgery instruments were used; middle-ear surgery instruments were at times required.
Cross-over septal flap technique
Two vertical septal mucosa incisions (one anterior and one posterior) are performed on both sides of the posterior third of the septum. The submucosal flaps are elevated; the posterior vomer and atretic plates are removed with a Kerrison punch or a 4 mm diamond burr drill. No drilling is performed on the lateral nasal wall, as this will result in more exposed bone, granulation tissue, and subsequent scarring with the risk of circular stenosis. Lateral widening is achieved using through-cutting instruments, to leave mucosal covering at the incised edges.
In unilateral choanal atresia, the first flap is harvested on the contralateral side to the choanal atresia and is pedicled superiorly; this flap is rotated to cover the drilled sphenoid rostrum bone. The second ipsilateral flap is pedicled inferiorly, allowing resection and drilling of the atretic plate, rostrum and basisphenoid. This flap is rotated inferiorly to cover the exposed vomer remnant and hard palate bone. In bilateral choanal atresia, the superior and inferior based flaps can be fashioned on either side. The lateral nasal wall mucosal integrity is maintained on both sides (Figure 1).
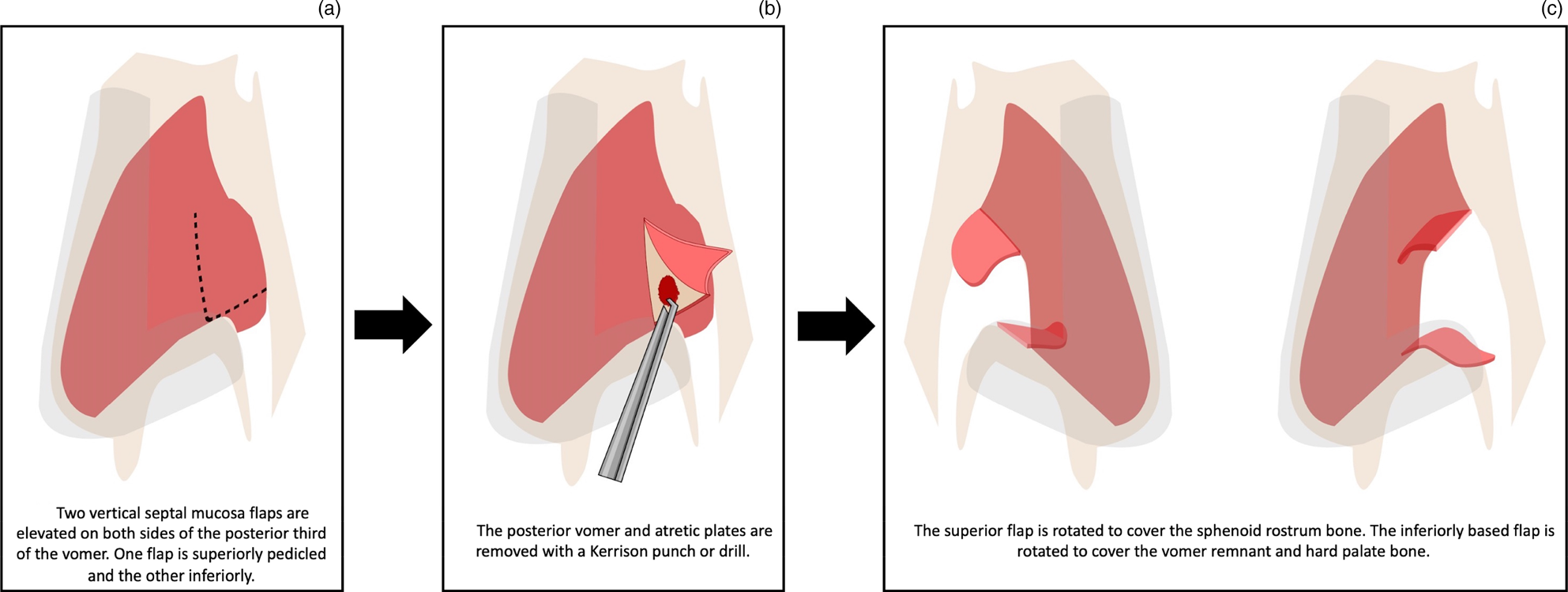
Fig. 1. Illustration of the surgical steps of left-sided choanal atresia repair (Vector Graphics Editor Software was used to create this figure).
Dressings
Fibrin glue was used on occasion to keep the flaps in position. A Silastic® was sutured to the nasal septum and kept in place for 15–20 days to avoid synechiae.
In the Italian cohort, five newborn and infant patients (mean age of 2.8 years) underwent second-look endoscopy under sedation, an average of 36 days following primary surgery, to address crusting or granulation, and to remove splints if still in situ (Figure 2). In the Ghana cohort, oxidised regenerated cellulose mesh (Surgicel; Ethicon, Somerville, New Jersey, USA) was used instead of fibrin glue and no Silastic splints were inserted. The patients were extubated following surgery and discharged the next day.

Fig. 2. Patent neo-choana at second-look endoscopy.
Results and analysis
A total of 18 patients with choanal atresia underwent surgery at both units from 2013 to 2020. Of those patients, 12 were operated using the cross-over septal technique and their data were subjected to further analysis in this study; 8 patients underwent the surgery in Varese and 4 in Accra. The six patients who underwent other surgical techniques had undergone primary surgery at other units and the fashioning of cross-over flaps was not feasible at the time of revision surgery.
Of the 12 patients who underwent the cross-over septal technique, 10 underwent primary unilateral procedures (3 left-sided and 7 right-sided) and 2 underwent bilateral revision procedures. The patients’ age range was 26 days to 50 years (median of 7 years). The male to female ratio was 1:5. Nine patients had bony choanal atresia; the rest had mixed (bony-membranous) choanal atresia. There were no associated malformations.
Silastic septal splints were inserted at the end of the procedure. Stents or mitomycin C were never used in any case. Five patients – the youngest patients in our cohort, with a mean age of 2.8 years – underwent second-look endoscopy under sedation to remove crusting, at 36 days on average, following primary surgery. Post-operatively, all repairs remained patent and no patient required revision surgery after a mean follow-up time of 10.6 months (range, 6–18 months; standard deviation = 3.3 months).
Discussion
Surgery is the only definitive treatment for choanal atresia. It aims to provide a patent choana to relieve obstruction. The transnasal endoscopic assisted approach, first described in the 1980s,Reference Morgan and Bailey10 is the least invasive and the current ‘gold standard’ treatment. The hypothetical disruption to midface growth using this approach is not supported by evidence.Reference Richardson and Osguthorpe11 The use of transnasal endoscopes increased the exposure to the atretic plate and led to better outcomes. Post-operative restenosis, even with this approach, remains common, at 11–35 per cent.Reference Gosepath, Santamaria, Lippert and Mann7 Patients can require an average of 2.7 procedures to achieve sustained choana patency.Reference Samadi, Shah and Handler8
Why does restenosis occur?
The rate of choanal restenosis is high. This has led to a debate on the best adjunct treatments to reduce stenosis rates, such as stenting and mitomycin. A recent metanalysis of choanal atresia repair with and without nasal stents found no difference in outcomes.Reference Strychowsky, Kawai, Moritz, Rahbar and Adil12 As such, a more pertinent research question might be ‘why does restenosis occur?’
Avoid exposed bone to reduce stenosis
Experience with other endoscopic nasal procedures has raised the principle of mucosal preservation. Where bone is left exposed, post-operative re-epithelialisation, scarring and/or granulation tissue will result in subsequent stenosis. This is the case in Draf III frontal sinusotomy and endoscopic dacryocystorhinostomy surgical procedures, where mucosal grafts and flaps are now used routinely to cover exposed bone at the end of the procedure in order to decrease stenosis rates and improve outcomes.Reference Hildenbrand, Wormald and Weber13 The same principle can be applied in choanal atresia surgery that involves resection of the vomer, and drilling of the basisphenoid and lateral nasal walls (pterygoid plates), leaving exposed bone circumferentially which will inevitably result in stenosis.
Minimise lateral nasal wall resection
Transnasal endoscopic techniques universally involve the resection of atretic bony plates, rather than puncturing and dilating them. In other techniques, the focus can, erroneously, be to widen the lateral choana by drilling the lateral nasal wall, specifically the medial pterygoid plates (with or without vomer removal).Reference Wormald, Zhao, Valdes, Pacheco, Ha and Tewfik4 This exposes more bone, and increases the bleeding risk associated with sphenopalatine injury, and may not be necessary when enough of the posterior vomer is removed. In cases where lateral mucosa and atretic bone require excision, through-cutting instruments are used, reducing bone exposure. In our series, lateral nasal wall drilling was not necessary in any case.
Resect posterior vomer bone
Mounting evidence suggests that removal of the posterior third of the septum (vomer bone) is crucial for improved outcomes.Reference Stankiewicz2 Resection of the posterior third of the vomer bone creates a singular elliptical anterior opening, the ‘common choana’ technique.Reference McLeod, Brooks and Mair14 This has the advantage of reducing the healing mucosal surface area, as the circumference of the large neo-choana is less than the sum of the circumference of two small choana. Additionally, the overall airflow through the singular elliptical common choana would be greater than the sum of the two circular choanae, as per Poiseuille's law.Reference McLeod, Brooks and Mair14 Thus, removal of the posterior portion of the bony septum alone may suffice to relieve choanal atresia.
Use mucosal flaps to cover exposed bone
Our cross-over septal technique meticulously repositions posterior septal mucosa flaps following resection of the atretic plate and vomer. The bilateral septal flaps cover all the exposed bone of the sphenoid and vomer, and as such we do not use stents at the end of the procedure. Thus far, none of our patients have undergone revision because of stenosis.
Flap design
Transnasal endoscopic choanal atresia surgery has led to the development of intranasal mucosal flaps. The flap location, mucosa source, attachment of the pedicle and number of flaps used vary according to technique.Reference El-Guindy, El-Sherief, Hagrass and Gamea15,Reference Kamel16 A common flap design is the lateral flap supplied by the posterior septal branch of the sphenopalatine artery and tethered to the lateral nasal wall.Reference Josephson, Vickery, Giles and Gross6,Reference Pasquini, Sciarretta, Saggese, Cantaroni, Macrì and Farneti17,Reference Saraniti, Santangelo and Salvago18 This was the previous technique used in our unit.Reference Karligkiotis, Farneti, Gallo, Pusateri, Zappoli-Thyrion and Sciarretta19 Two issues arose with this technique: firstly, the vomer bone remnant on the nasal floor remained uncovered and would lead to partial restenosis at this site;Reference Saraniti, Santangelo and Salvago18 and secondly, drilling the lateral nasal wall exposed more bone, with subsequent concentric re-epithelialisation, scarring and stenosis.
• Choanal atresia requires surgery to fashion a patent choana; post-operative re-stenosis occurs in 11–35 per cent of cases
• Our technique uses posterior septal mucosal flaps to resurface the neo-choana following atresia resection
• Two vertical septal mucosa incisions are made on each posterior septum side; submucosal flaps are elevated, and the posterior vomer and atretic plate(s) are removed
• One flap is pedicled superiorly and rotated over the bare skull base and sphenoid bone; the contralateral flap is pedicled inferiorly and rotated to cover the exposed vomer remnant and hard palate
• This paper describes choanal atresia surgery related principles to reduce stenosis
• Our endoscopic transnasal cross-over septal flap technique resulted in 100 per cent patency, without stent use
Modified Stamm technique
Our technique is a modification of the one described by Stamm and PignatariReference Stamm and Pignatari9 used in 33 patients in their series. The main differences are that Stamm et al. perform an ‘L’-shaped septal flap in continuity with atretic plate mucosa that remains pedicled on the upper and lateral nasal walls, whereas we only use septal mucosa and release the septal flaps with posterior vertical incisions, leaving superiorly and inferiorly pedicled flaps. In addition, Stamm et al. packed the nasal cavity with a Merocel (TM) sponge inside a finger glove, while we use septal Silastic splints but no packing or stents.
Analysis of cross-over septal technique
In a meta-analysis of 20 studies, comprising a total of 238 cases, the mean success rate with endonasal endoscopic repair was 85.3 per cent.Reference Durmaz, Tosun, Yildirım, Sahan, Kivrakdal and Gerek20 Stamm and Pignatari, in their seminal paper, reported a high success rate for unilateral cases (86 per cent, 19 out of 22);Reference Stamm and Pignatari9 similarly, in our smaller study of 12 cases, no recurrence has been observed. Stamm and Pignatari's paper was published in 2001 when the microscope technique was still in use, whereas the meta-analysis described endoscopic repair, which was still developing, with a potential associated learning curve. These issues do not preclude procedural failure, which may occur in any choanal atresia surgery, especially if performed in patients aged under six months.Reference Stamm and Pignatari9 The combined success rate for both studies is thus 90 per cent.
Patient age at surgery
In a recent study by our group,Reference Karligkiotis, Farneti, Gallo, Pusateri, Zappoli-Thyrion and Sciarretta19 statistical analysis determined that patient age of below one year at the time of surgery was a predictive factor for restenosis (p = 0.053), and age younger than five years was a predictive factor when considering only unilateral choanal atresia (p = 0.030). Based on these results, choanal atresia patients under the age of one year at the time of surgery have a higher risk of post-operative stenosis and the need for revision surgery. Therefore, in patients with unilateral choanal atresia, delaying surgical intervention until after the first year of life, or even later (if not contraindicated), may increase success rates.
Conclusion
The cross-over technique for choanal atresia has a high success rate, 100 per cent in our series, and low morbidity, without the need for post-operative stenting. Use of mucoperiosteal flaps to cover the vomer and sphenoid rostral exposed bone, removal of the posterior vomer, and minimal instrumentation to the lateral nasal wall are the best ways to avoid post-operative stenosis.
Acknowledgement
We thank Şehriyar Cem for providing the artwork.
Competing interests
None declared




