Introduction
A classification of attic retraction pockets based on the depth and erosion of the pocket by otoscopic, microscopic or endoscopic examination has been presented.Reference Vijayendra, Mahajan, Vijayendra and Ramdass1 The extent of retraction and erosion of the ossicles and scutum, and the attic retraction pocket contents determine the grade of attic retraction pocket.
This study presents the strategy for reconstruction of the lateral epitympanic wall and ossicles after attic retraction pocket removal. Previous studiesReference Νankivell and Pothier2 have questioned whether attic retraction pockets should simply be observed, and the majority recommend excision and reconstruction, cautioning that the lateral epitympanic wall should be reconstructed with cartilage to prevent attic retraction pocket reformationReference Park, Kim, Park, Lee and Kim3,Reference Kasbekar, Patel, Rubasighe and Srinivasan4 and secondary formation of cholesteatoma.Reference Comacchio, Mion and Pedruzzi5
This study presents our recommended reconstruction after attic retraction pocket excision based on data showing the subsequent conditions of the tympanic membrane and hearing. To facilitate the readers’ understanding, we then present an earlier series of our own less-effectively assigned reconstructions and their outcomes. Finally, we present the outcomes of revision surgical procedures of the complications of the original series when our final modified strategy is applied. With these three series, we demonstrate how to tailor the reconstruction to the grade of attic retraction pocket, to secure long-term benefits. In addition, we compare our attic retraction pocket recurrence rates to earlier reports of attic retraction pocket repair.Reference Pappas6–Reference Pfleiderer, Ghosh, Kairinos and Chaudhri9
Materials and methods
This retrospective study was reviewed by the Vijaya ENT Care Super Speciality Otology Centre's Ethics Committee, and received approval (protocol number: 2020–07).
Patients
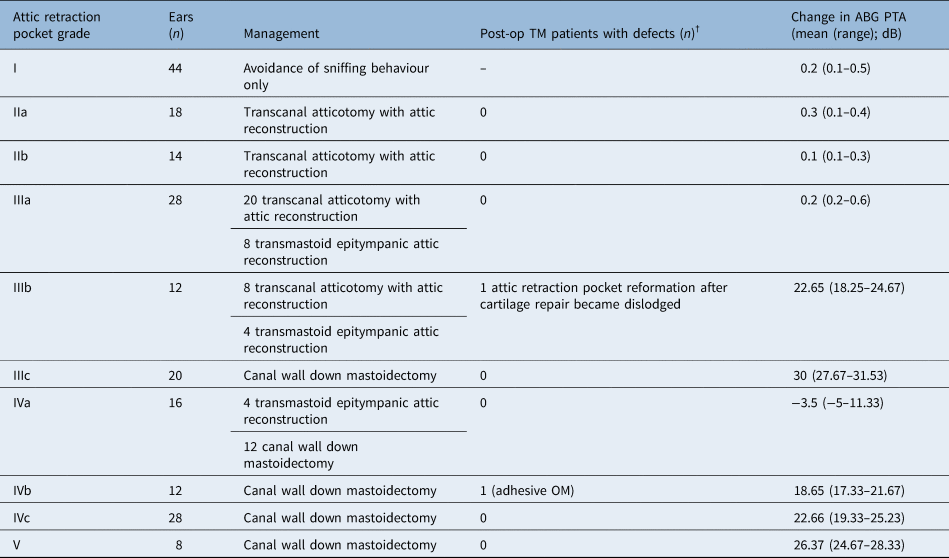
The medical records of 192 patients (250 ears) who presented between January 1999 and December 2019 to our tertiary referral otology centre in India were reviewed retrospectively. All clinical examination, otoendoscopic examination and audiological evaluation data were collected. All patients were classified using the attic retraction pocket classification system, from grades I to V, as detailed in Table 1, and were managed surgically depending on the attic retraction pocket grade, as detailed in Table 2.Reference Honnurappa, Mahajan, Vijayendra, Ramdass and Redleaf10
Table 1. Grades of attic retraction pockets

Table 2. Recommended resection and reconstruction based on attic retraction pocket grade

Parenthetically, we clarify here that 60 per cent of patients who initially presented with grade II ears dropped out of regular follow up. Of the remaining 40 per cent who did attend for follow up, 50 per cent progressed to higher grades of retraction pocket. Of these 40 per cent who came for follow up, 6 per cent showed progression to cholesteatoma. Hence, to prevent this progression, and to preclude cholesteatoma, we treated these grade II ears surgically.
Patients with pars tensa and flaccida retractions, or middle-ear effusions, cholesteatoma, tympanic membrane perforations, or previous ear surgery, were excluded.
Operations
Forty-four grade I ears were observed in this protocol and 250 ears underwent surgical procedures. Two hundred ears (156 patients) underwent our recommended resection and reconstruction management, as outlined in Table 2; their post-operative results are reported in Table 3. The depth and anatomy of the attic retraction pockets were determined by microscopic and endoscopic examination. All operations were performed by the same senior surgeon using an operative microscope.
Table 3. Outcomes of patients who underwent the final reconstruction strategy*

Total of 156 patients (200 ears). Two of the 200 ears had complications (1 per cent). The mean follow-up duration was 84 months (range, 36–240 months). *As outlined in the Materials and methods section. †Post-operatively, a non-intact tympanic membrane, attic retraction pocket reformation, tympanic membrane perforation or evidence of cholesteatoma formation. Post-op = post-operative; TM = tympanic membrane; ABG = air–bone gap; PTA = pure tone average; OM = otitis media
The operations conducted were atticotomy, and canal wall up and canal wall down tympanomastoidectomy procedures. In order to reconstruct the scutum and attic lateral wall, the tympanic membrane with intact pars flaccida was dissected intact and reflected forward to allow scutal removal and opening of the lateral wall of the attic. The bony barriers were reconstructed with the patient's conchal cartilage and crushed perichondrium. The intact tympanic membrane was then returned to its original location. There was therefore no tympanic membrane graft, and the mastoid cavity and epitympanum were not left exposed.
In order to reduce or obliterate the mastoid bowl after canal wall down mastoidectomy, the mastoid cortex was lowered to the level of the sigmoid sinus. Peri-cranial free grafts were placed into the additus ad antrum / tegmen mastoideum area, and a posteriorly-based peri-cranium flap was recruited and draped down into reduced antrum. Finally, the skin of the meatoplasty was sectioned horizontally from lateral to medial, and tacked back to the obliterative peri-cranial tissue.
Post-operative care for the reduced or obliterated mastoid cavities included acetic acid administration for 15 days to avoid granulation formation.
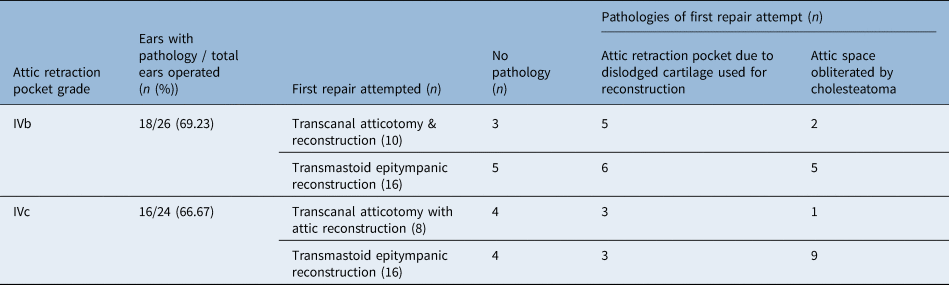
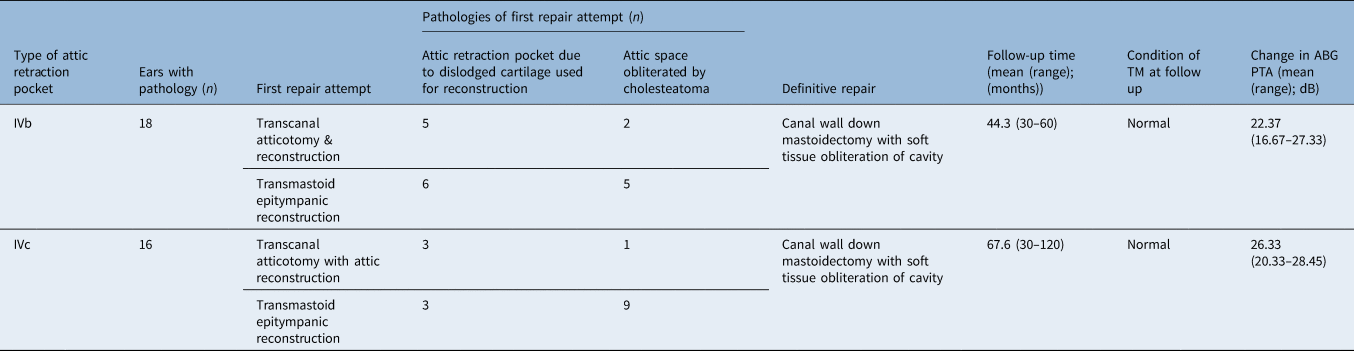
The remaining 50 ears (36 patients) had attic retraction pocket grades IVb and IVc that had not initially undergone our recommended resection or reconstruction as outlined in Table 2. Thirty-four of these ears had complications after their first surgical procedures, and underwent resection or reconstruction, as recommended in Table 2, only as revision operations. Their outcomes after their first surgical procedures are reported in Table 4 and their outcomes after revision are reported in Table 5. In summary, 250 ears were operated on and of these 250, 34 underwent a second revision surgical procedure. The numbers of patients who declined surgical procedures in each group or who failed to return for follow up were calculated.
Table 4. Outcomes of patients with attic retraction pocket grades IVb and IVc repaired with atticotomy and epitympanic reconstructions

Total of 36 patients (50 ears). Complication rate of 68 per cent (34 of 50 ears). Mean follow-up duration of 55.9 months (range, 30–120 months).
Table 5. Outcomes of 34 IVb and IVc attic retraction pockets that received revision surgery based on the revised reconstruction strategy

The patients with IVb attic retraction pockets were followed up for a mean of 44.3 months (range, 30–60 months) and those with IVc attic retraction pockets were followed up for a mean of 67.6 months (range, 30–120 months). TM = tympanic membrane; ABG = air–bone gap; PTA = pure tone average
Outcomes
The condition of the tympanic membrane on microscopic evaluation and changes in the pure tone average air–bone gap were recorded post-operatively. Pure tone average was calculated from 0.5, 1 and 2 kHz frequencies.
Data analysis
Pre- and post-operative air–bone gap pure tone averages were compared using paired t-tests for the patients reported in Table 3. The outcomes of the 50 ears that underwent surgical procedures not in accordance with the recommendations in Table 2 are reported in Table 4. These outcomes were compared, using paired t-tests, to the outcomes of the 34 of the 50 patients who underwent revision operations as reported in Table 5. The SPSS program was used for statistical analysis.
Results
A total of 156 patients (200 ears) underwent the recommended strategy for attic retraction pocket reconstruction (outlined in Table 2), as shown in Table 3. These patients comprised 75 females and 81 males, with an average age of 38.3 years (range, 16–54 years). The mean follow-up duration was 84 months (range, 36–240 months). One ear needed a revision surgical procedure for a recurrent attic retraction pocket after a dislodged cartilage scutal reconstruction. Another ear showed adhesive otitis media after reconstruction. These 2 (of 200) ears indicate a surgical complication rate of 1 per cent. Post-operative care for the reduced or obliterated mastoid cavities involved acetic acid administration for 15 days to avoid granulation formation. Ten per cent of these reduced bowls required acetic acid administration for 1 month instead of 15 days. No obliterated bowl had drainage or persistent granulation. Air–bone gaps improved in most instances: minimally (<1 dB) in the lower grade attic retraction pocket repairs and to 20 dB or above in the higher grades (p < 0.05). In this group, six patients declined surgery and three were lost to follow up.
Thirty-six patients (50 ears) with grade IVb and IVc ears who initially underwent reconstruction not in accordance with our recommended strategy are listed in Table 4. They were 20 females and 16 males, average age of 39.7 years (range, 18–49 years). Follow-up duration was a mean of 55.9 months (range, 30–120 months). According to our final management template, each of these patients should have received a canal wall down mastoidectomy as their initial surgical procedure. Instead, they had undergone atticotomy and cartilage reconstruction of the lateral epitympanic wall with subsequent attic retraction pocket reformation or cholesteatoma formation in 34 out of 50 ears (68 per cent). In this group, two patients declined surgery and one was lost to follow up.
These patients with post-operative complications (34 ears) underwent second operations for treatment, which were all canal wall down mastoidectomies, as reported in Table 5. The patients classed as attic retraction pocket grade IVb were followed up for a mean of 44.3 months (range, 30–60 months) and showed intact tympanic membranes without evidence of attic retraction pocket recurrence or cholesteatoma. The mean air–bone gap pure tone threshold improvement was 22.37 dB (range of 16.67–27.33 dB, p < 0.05). The patients classed as grade IVc were followed up for a mean of 67.6 months (range, 30–120 months), and showed intact tympanic membranes without evidence of attic retraction pocket recurrence or cholesteatoma. Mean air–bone gap pure tone threshold improvement was 26.33 dB (range of 20.33–28.45 dB, p < 0.05). In this group, no patients declined surgery and none were lost to follow up.
Discussion
This study, which has a level of evidence of five, describes three series of reconstructions: 200 ears which were reconstructed per our protocol (Table 3), 50 ears which were basically undertreated (Table 4) and 34 ears which underwent a second corrective revision surgical procedure (Table 5). The study shows the outcomes for our recommended attic retraction pocket surgical management. The recurrence rates, complication rates and post-operative hearing outcomes of this series indicate that the final surgical strategies, stratified by attic retraction pocket type, are acceptable, perhaps even optimal. Of the 200 ears, 1 ear showed recurrent attic retraction pocket and 1 ear showed adhesive otitis media after 84 months of follow up (range, 36–240 months). This operative template was created in response to the failures reported in Table 4: 34 (68 per cent) of the 50 patients who received initial atticotomy and epitympanic reconstruction for grade IVb and IVc attic retraction pockets showed recurrence of the attic retraction pocket or new-onset cholesteatoma, but none of these 34 who were revised per the final template showed recurrent cholesteatoma or other complications after 56 months of follow up (range, 30–120 months) (Table 5).
Comparison of our results to historical series also shows the efficacy of the other operative strategies that we report here. An early report from 1984 found that ‘several’ of 25 attic retraction pockets repaired with dura for scutal reconstruction had recurrent retractions and effusions in the 26–41-month follow-up period.Reference Cross7 A 1994 report of surgical management of attic retraction pockets found that 17 per cent of attic retraction pockets treated with Bondy mastoidectomy had cavity myringitis and granulomas.Reference Pappas6 Follow-up times were not reported. In 2003, repairs with cartilage and with bone paste resulted in 57 and 21 per cent, respectively, of patients with recurrent attic retraction pockets.Reference Pfleiderer, Ghosh, Kairinos and Chaudhri9 The mean time to recurrence was 29 months (range to recurrence, 10–98 months), but the full follow-up times were not reported. More recently, in 2010, 22 per cent of attic retraction pockets showed recurrence after endoscopic treatment and repair.Reference Marchioni, Alicandri-Ciufelli, Motelni, Genovese and Presutti8 Mean post-operative follow-up duration was 20 months, but the range is not reported.
One strength of this study was the length of follow up for patients who underwent surgical procedures, which suggests that the prescribed operative repair is stable. Another strength was the opportunity to review the results of patients who did not undergo the surgical procedures recommended in Table 2 (Table 4) and to see the outcomes when the recommended reconstruction strategy was subsequently implemented (Table 5). The patients described in Tables 4 and 5 in effect served as our controls for this study, and because their outcomes guided future surgical planning, ethically we were reassured that their recurrences were not the result of randomisation to an inadequate treatment arm. A weakness of this study was our lack of a full understanding of the 32 per cent of patients in Table 4 who appear to have escaped attic retraction pocket recurrence. Overall, the principal lesson from this study is which operation to perform for which grade of attic retraction pocket.
A second lesson is the use of endoscopes to evaluate the depths and extensions of the attic retraction pockets. We and others have found them very useful for diagnostic purposes,Reference Marchioni, Villari, Mattioli, Alicandri-Ciufelli, Piccini and Presutti11 while our colleagues have also found them useful to preserve middle-ear and epitympanic airflow passages.Reference Marchioni, Alicandri-Ciufelli, Motelni, Genovese and Presutti8 In our work, the use of endoscopes has helped to determine which reparative operation should be performed.
• The otological endoscope allows more precise assessment of the extent of attic retraction pockets than previously possible with the operating microscope
• A grading system for attic retraction pockets has been previously presented
• This study outlines the successful reconstruction strategy based on attic retraction pocket grade
• Pairing operative reconstruction to attic retraction pocket grade showed long-term stability of the tympanic membrane, middle ear and hearing
Finally, brief consideration must be given to past studies of attic retraction pocket formation and repair, and the long history of difficulties. In the 1970s, Sade detailed the stages of retraction of the pars flaccida and tensa with adhesive otitis and ossicular erosion.Reference Sade12 In the 1970s and 1980s, Paparella and colleagues,Reference Paparella13,Reference Paparella and Jung14 and Wallenborn,Reference Wallenborn15 described the frustrations of repairing attic retraction pockets and other retractions coupled with adhesive otitis media. The various repairs, with fascia, dura, bone paste and cartilage,Reference Cross7–Reference Pfleiderer, Ghosh, Kairinos and Chaudhri9 as well as the surgical techniques, have been described by multiple authors.Reference Pappas6,Reference Marchioni, Alicandri-Ciufelli, Motelni, Genovese and Presutti8,Reference Sade12–Reference Sanna, Facharzt, Russo, Lauda, Pasanisi and Bacciu16 The main cause of attic retraction pocket formation and the primary obstacle to successful repair appears to be dysventilation syndrome, which occurs when the lateral incudo-malleolar fold and the tensor folds are intact,Reference Tarabichi, Marchioni and Kapadia17 as they usually are, but the isthmus between the long process and the manubrium is blocked.Reference Marchioni, Alicandri-Ciufelli, Molteni, Artioli, Genovese and Presutti18 We present our attic retraction pocket series, with recommended repair strategies, and compare our current results to our earlier non-advantageous repair strategies and to previous series’ results. We believe our data show a useful approach to this age-old problem.
Competing interests
The authors declare none.