The prevalence of mental disorders, mainly anxiety disorders and affective disorders, in older people is high: one in three older people were affected in the course of the past year.Reference Andreas, Schulz, Volkert, Dehoust, Sehner and Suling1 According to the World Health Organization, dementia is the leading cause of dependency and disability among older people. Dementia currently affects around 10 million people in Europe, and its prevalence is expected to double by 2030.2
Effects on mental health
Several studies have examined the effectiveness of multidisciplinary home treatment models for elderly patients with mental illness.Reference Klug, Gallunder, Hermann, Singer and Schulter3 Data show significant positive effects on relevant parameters such as fewer symptoms of depression,Reference Banerjee, Shamash, Macdonald and Mann4,Reference Klug, Hermann, Fuchs-Nieder, Panzer, Haider-Stipacek and Zapotoczky5 an improvement in global and psychosocial functioningReference Klug, Hermann, Fuchs-Nieder, Panzer, Haider-Stipacek and Zapotoczky5,Reference Stobbe, Wierdsma, Kok, Kroon, Roosenschoon and Depla6 and better quality of life.Reference Klug, Hermann, Fuchs-Nieder, Panzer, Haider-Stipacek and Zapotoczky5 Furthermore, the findings discussed by Klug et alReference Klug, Hermann, Fuchs-Nieder, Panzer, Haider-Stipacek and Zapotoczky5 indicate fewer admissions to nursing homes, fewer in-patient days spent in psychiatric hospitals and, subsequently, lower costs of care. Therefore, geropsychiatric home treatment (GHT) for elderly patients has been implemented in several parts of Austria. This treatment model includes social workers, psychiatric nurses, psychologists and psychiatrists, and offers an individually tailored home treatment for the patients in contrast to treatment as usual (TAU).
Effects on physical health
So, GHT has positive effects on older people in regard to mental health. But what about its effects on physical health? Studies indicate a relationship between physical and mental health in general,Reference Ohrnberger, Fichera and Sutton7–Reference Kisely and Goldberg10 but specific studies in this field are scarce. Several authors refer to a significantly increased risk of chronic physical health problems in people with mental illness;Reference Park, McDaid, Weiser, Von Gottberg, Becker and Kilian11,Reference Firth, Siddiqi, Koyanagi, Siskind, Rosenbaum and Galletly12 Ohrnberger et alReference Ohrnberger, Fichera and Sutton7,Reference Ohrnberger, Fichera and Sutton13 stated that little is known about the dynamic cross-effects between mental health and physical health. They found that the indirect effect of past mental health on physical health is mediated by lifestyle choices and social interactions. There is solid scientific evidence that social relationships affect a range of health outcomes, including mental health, physical health, health habits and mortality risk.Reference Umberson and Montez14 People with mental illness are less likely to have protective relationships, and when their social links are poor, their recovery is compromised and they are at heightened risk of relapse.Reference Pevalin and Goldberg15 Furthermore, they are disadvantaged concerning recognition and treatment of physical health problems.Reference Coghlan, Lawrence, Holman and Jablensky9 Hummel et alReference Hummel, Weisbrod, Boesch, Himpler, Hauer and Hautzinger16 demonstrated the effectiveness of cognitive–behavioural psychotherapy regarding improvement in physical and functional parameters in elderly patients. Callahan et alReference Callahan, Kroenke, Counsell, Hendrie, Perkins and Katon17 and Camacho et alReference Camacho, Davies, Hann, Small, Bower and Chew-Graham18 discussed a collaborative care management for late-life depression and its association with improvement in physical functioning. Taking all these findings into account, we ask whether it is indeed possible that a focused GHT not only improves mental health, but can also reduce the need for physical treatment?
Thus, the aim of the present study was to examine the effect of this special GHT model on physical health for older people with mental illness, by the number of contacts with health services, number of prescriptions concerning medical drugs except psychotropic drugs as primary outcomes, number and length of hospital stays, number of prescriptions regarding psychotropic drugs and number of consultations with psychiatrists as secondary outcomes. It was hypothesised that patients in this particular treatment will have a significantly lower number of contacts with health services, prescriptions and hospital stays compared with patients receiving TAU.
Method
Study design
A data-based, retrospective matched-pair study was conducted to analyse the possible effects of the GHT model for the utilisation of medical care. Patients in GHT were allocated to the intervention group. For each patient in GHT, two statistically comparable patients in TAU were chosen by 1:2 matching and then allocated to the control group. Matched case–control study designs are commonly implemented in the field of public health and medical literature,Reference Rose and van der Laan19,Reference Burden, Roche, Miglio, Hillyer, Postma and Herings20 for example, in cancer researchReference Ishikawa, Yasunaga, Matsui, Fushimi and Kawakami21 and psychiatric research.Reference Osimo, Brugger, De Marvao, Pillinger, Whitehurst and Statton22,Reference Fond, Pauly, Bege, Orleans, Braunstein and Leone23
Data from the regional medical insurance company (RMIC) in Styria (a regional branch of the National Health Insurance in Austria) and data from the public hospitals in Styria were combined for both groups, and the patient pathways within 2016 were analysed for the statistical computing. The insurance data refer to the number of prescription drugs and the number of consultations with general practitioners (GPs) and extramural specialists in internal medicine and psychiatry, either panel doctors or private doctors of one's choice, whose bills are fully or partially paid by the health insurance in Austria.
Written informed consent was obtained from all participants despite only standardly compiled data being used; all data were pseudonymised. In this case, no ethics approval for the study was required from the ethics committee in Austria.
Setting
The study was conducted in Graz, the capital city of Styria, and in three rural regions in Styria, one of the nine states in Austria. At the beginning of 2016, about 18% of the 280 000 inhabitants of Graz were aged ≥65 years. The percentage was slightly higher in the three rural regions, with a total of approximately 228 000 inhabitants.
All potential participants received full routine care within the Austrian healthcare system. The additional multi-professional treatment (GHT) was provided by the regional psychosocial services (PSS), i.e. three publicly funded, non-profit organisations specialising in mental health services in the community (Gesellschaft zur Förderung seelischer Gesundheit, Rettet das Kind Steiermark and Hilfswerk Steiermark). All psychiatric in-patient, out-patient and community services in the area could refer individuals to GHT.
The patients in the intervention group had to be in GHT in 2016 for at least 2 months, and had to be in active treatment between July and December.
Intervention
All participants in both conditions had free access to all aspects of healthcare as routinely provided by the Austrian healthcare system, including input from GPs, psychiatrists, day centres with social and occupational activities and, if required, nursing care in the individual's home.Reference Klug, Hermann, Fuchs-Nieder, Panzer, Haider-Stipacek and Zapotoczky5
In addition to routinely provided care, patients in the intervention group received a GHT offered free of charge. First, a multi-professional comprehensive geropsychiatric assessmentReference Pinto, Gautam and Awasthi24,Reference Reuben25 and psychiatric interviewReference Varghese and Dahale26 took place. This assessment was carried out by a multi-professional team comprising a psychiatrist specialising in geriatric psychiatry and therefore familiar with somatic diseases in old age, psychologists, social workers and psychiatric nurses. However, in the rural regions, resources were partly limited to psychiatrists, psychologists and social workers. Subsequently, each patient in GHT was assigned to a primary keyworker who was one of the members of the multi-professional GHT team.
All team members specialised in dealing with the complex socio-psychiatric problems elderly people are confronted with.Reference Klug, Hermann, Fuchs-Nieder, Stipacek and Zapotoczky27 In accordance with Levin and Miya,Reference Levin and Miya28 the service (originally based on psychosocial rehabilitation) is highly individualised and focuses on recovery and strengths depending on the needs and resources of the patients. A detailed description of the setting has been published elsewhere.Reference Klug, Hermann, Fuchs-Nieder, Stipacek and Zapotoczky27
The cost-efficiency of GHT has already been proved in a previous study by Klug et al,Reference Klug, Hermann, Fuchs-Nieder, Panzer, Haider-Stipacek and Zapotoczky5 therefore it was not assessed in the present study.
Patient selection and matching
Patients were referred to the intervention group if they met the following inclusion criteria:
a psychiatric diagnosis according to ICD-10 criteria,29 age ≥65 years, main residence in one of the four regions, living independently at home, active treatment (GHT) between July and December of 2016 and treatment duration of at least 2 months.
Exclusion criteria were as follows: no informed consent, a score of <23 on the Mini-Mental State Examination,Reference Felnhofer, Kothgassner and Kryspin-Exner30 no regional medical insurance and an incomplete data-set (e.g. treatment duration <2 months, dropped out, relocated, indicated intention to give up independent living and move to a nursing home).
Matching
Patients for the control group were selected by 1:2 exact matching. For building the control group, the variables described above from the standardly compiled PSS data of all patients in the intervention group were transmitted to the RMIC, who identified potential controls from the standardly compiled data of all patients in Styria in 2016, using these matching criteria: no GHT in 2016, identical age in years, identical gender and identical residential area.
Next, the comparability of the control group was assured regarding psychiatric medication and the potential requirement of psychiatric care. For that to happen, the cohort was further limited by applying the following criteria: at least one consultation with a specialist in psychiatry in 2016, and prescriptions of psychotropic drugs in 2016 with at least one of these active ingredients: selective serotonin reuptake inhibitors, diazepine, oxazepine, thiazepine and oxepine, benzodiazepine derivates, other antidepressants and beta-adrenoreceptor antagonists.
Finally, each patient in the intervention group was matched with two statistically comparable people in the control group from the cohort of potentially comparable people with requirement of psychiatric care via computerised random sampling.
Variables
The following primary outcomes were analysed with descriptive and inferential statistics: number of consultations with GPs, number of consultations with specialists in internal medicine and number of prescriptions of medical drugs (excluding psychotropic drugs). The following secondary outcomes were analysed with descriptive and inferential statistics: number of consultations with specialists in psychiatry, number of prescriptions of psychotropic drugs, number of hospital discharges excluding psychiatric departments, number of hospital discharges in psychiatric departments and length of hospital stays.
Data sources
The software-controlled data analyses are based on standardly compiled patient and service data from the PSS, and standardly compiled data concerning patient characteristics, extramural consultation rates and the prescriptions extracted by the RMIC. In 2015, about 74% of the Styrian residential population were insured by the RMIC. Thus, it is the biggest medical health insurance provider in Styria.
The analyses for hospital discharges and length of hospital stays are based on the standardly compiled patient, diagnosis and service data of the public hospitals in Austria.
The standardly compiled data of the PSS comprised the demographic variables (age, gender, residential area), medical insurance provider, initiation of treatment, main psychiatric diagnoses according to ICD-10 criteria,29 and the living conditions for all patients in the intervention group.
Concerning the RMIC data, demographic variables of the patients in the control group, and number of consultations (GPs and specialists) and prescriptions (including the Anatomic Therapeutic Chemical Code (ATC) of drugs) for all patients in the intervention and control group were used.
Data from the public hospitals comprised hospital discharges, length of stay, main diagnoses according to ICD-10 criteria,29 and full medical performance during the stay for all patients in the intervention and control group.
All data-sets were pseudonymised by a definite patient identifier to display the cross-sectoral healthcare pathways for 2016. For each patient, the individual care pattern was built, and the differences in the observed frequencies were statistically analysed.
Study size
The definition of the required study size and length of observation period was guided by the leading question: does the GHT model affect the number of contacts with GPs per year? The average consultation rate per year and inhabitant related to the entire population in Austria is about 13.7.Reference Hofmarcher31 It can be assumed that the number of consultations is higher in the ≥65 years age group than in all other age groups.
On the basic assumptions of inferential statistics with a type 1 error of 5%, a statistical power of 80% and an estimated effect size of r = 0.3 (minimum difference of 3.6 consultations per patient and year between both groups – medium effect size because no comparable study has been carried out in Austria), at least 1219 consultations have to be observed in the intervention group and control group within a year for statistically significant results. Based on these conservative assumptions, a sample size of 89 was required.
Statistical methods
The results concerning the characteristics of patients and the observed frequencies were analysed for the intervention group (GHT) and control group (TAU) by means of descriptive and inferential statistics. The absolute frequencies and the percentage distributions were used for description of the nominal data.
The frequencies of the intervention group and control group are described as absolute frequencies per year, mean and median. The differences in frequency were analysed by Wilcoxon rank-sum test for independent samples at a 5% significance level for a two-tailed test. For all analyses, the statistics software R (version 3.5.3 for Windows; R Foundation for Statistical Computing) was applied.
The observed frequencies of the intervention and control groups are always related to the whole of 2016: out of 91 patients in the intervention group, 44 received continuous treatment in 2016 (48.4%), 32 received treatment for half a year or more (35.2%) and 15 received treatment for at least 2 months (16.4%). For those, the observed frequencies of their individual active treatment period were considered and extrapolated to the absolute frequencies of a full year.
Results
Patient flow
A total of 482 patients were treated with GHT in 2016. A total of 91 patients met the inclusion criteria and were assigned to the intervention group. Figure 1 illustrates the patient flow and the 1:2 matching.

Fig. 1 Patient flow and matching. GHT, geropsychiatric home treatment; MMSE, Mini-Mental State Examination; RMIC, regional medical insurance company; TAU, treatment as usual.
Baseline characteristics of patients
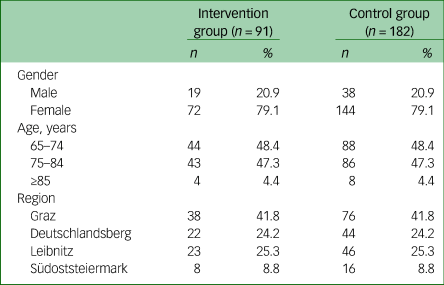
Age, gender and the residential area of the patients in the intervention group and control group are described in Table 1. The average age in both groups was 75.09 years (s.d. 6.0), and the majority of patients were female and from the Graz region. There were no differences in the baseline characteristics between the intervention group and control group because of the exact matching.
Table 1 Baseline characteristics of patients in the intervention group (geropsychiatric home treatment) and the control group (treatment as usual)
The primary diagnoses were assessed in detail according to ICD-10 criteria,29 and combined with homogenous diagnosis groups for patients in the intervention group: 38.4% had affective disorders (mainly F33 – recurrent depressive disorder and F32 – depressive episode); 26.4% had a mild form of organic, including symptomatic, mental disorders (mainly F00 – dementia in Alzheimer's disease); 25.3% had neurotic, stress-related and somatoform disorders (mainly F41 – other anxiety disorders) and 9.9% had other psychiatric diagnoses.
Main results
The observed frequencies and statistical values for the primary and secondary outcomes for the intervention group, as well as the control group, are shown in Table 2.
Table 2 Main results for the intervention group (geropsychiatric home treatment) and the control group (treatment as usual)

a. ‘Number’ refers to a whole year and to all patients (91 and 182, respectively).
b. ‘Mean’ and ‘Median’ are given for the individual patient.
Thus, the number of consultations with GPs and specialists in internal medicine per patient in 2016 was significantly lower in the intervention group than the control group. The number of prescriptions of medical drugs except psychotropic drugs per patient in 2016 was also significantly lower than in the control group.
Regarding the secondary outcomes, the number of consultations with specialists in psychiatry per patient in 2016 was significantly lower in the intervention group than the control group. Also the number of prescriptions of psychotropic drugs per patient in 2016 was significantly lower in the intervention group.
The results concerning number of hospital discharges excluding psychiatric departments, and number of hospital discharges in psychiatric departments, show that there was no significant difference between the intervention and control groups. Scheduled hospital stays (e.g. day hospital, planned surgery, in-patient chemotherapy, etc.) were excluded to minimise bias in the results.
The length of hospital stays in days was also considered. In the intervention group, the median length of hospital stays was 2.5 days compared with 4.0 days in the control group. The difference between the groups was not statistically significant.
Table 2 shows significant differences for prescriptions concerning medical drugs except psychotropic drugs, as well as prescriptions concerning psychotropic drugs. Further, the number of prescriptions in both categories was examined in more detail by analysing the subgroups based on the ATC Classification System (second level, therapeutic subgroup). There was a significant difference for the ATC subgroups ‘agents acting on the renin-angiotensin system’ (C09) and ‘psychoanaleptics’ (N06) concerning the number of prescriptions for the intervention group. In almost every other subgroup there was also a lower number of prescriptions; however, the difference between the intervention group and control group was not significant.
The results for the top 15 prescriptions (ATC second level) are given in Table 3.
Table 3 Top 15 prescriptions (ATC second level) results for the intervention group (geropsychiatric home treatment) and the control group (treatment as usual)

ATC, Anatomic Therapeutic Chemical Code.
a. ‘Number’ refers to a whole year and to all patients (91 and 182, respectively).
b. ‘Mean'and ‘Median’ are given for the individual patient.
c. Anti-epileptics are included in both categories.
Discussion
Main findings
The present retrospective, matched-pair cohort study indicates that GHT has a positive effect on parameters of physical health in elderly patients. GHT was associated with a smaller number of consultations with health services (i.e. GPs, psychiatrists and other specialists) and prescription drugs. This not only refers to psychotropic drugs but is also true for non-psychotropic drugs.
However, the cohorts did not differ significantly concerning the number of general hospital discharges and the length of general hospital stays. There was also no significant difference concerning the number of psychiatric hospital discharges.
In view of the specified duration of the study and very small numbers of in-patients, it was difficult to prove statistically relevant changes for the number of hospital admissions alone.
The findings suggest that there was a change in the mental state and medical condition of the patients. The lower number of prescriptions in relation to consultations with GPs and psychiatrists can be partly explained by the better psychiatric care in the project itself. On the other hand, the lower number of consultations with GPs could also have led to the lower number of prescriptions, as more frequent consultations with GPs most likely leads to more drug prescriptions. The high frequency of consultations with GPs in the control group compared with the intervention group could be an indicator of loneliness, missing social contacts and the GP often being the only contact person. However, the lower number of consultations with specialists in internal medicine, and especially the decrease in medication in the somatic and psychiatric areas, cannot be explained that way. The following fact is striking: the decrease in somatic medication is even stronger than the decrease in psychiatric medication. There was a slight (not significant) decrease in all somatic medication groups, but the largest decreases were in medications acting on the renin-angiotensin system, medications used for diabetes and acid-related disorders, and psychoanaleptics, including antidepressants. The decrease in antidepressants could be the result of GHT alone, but recent studiesReference Vian, Pereira, Chavarria, Köhler, Stubbs and Quevedo32 show that the renin-angiotensin system and depression are strongly correlated. Although randomised controlled trials providing definitive proof are yet to come, there are indications of centrally powerful substances from the renin-angiotensin system having an effect on the treatment of depression. One reason for this is the triggering of a cascade of stress, especially chronic stress. This rebounds on the renin-angiotensin system, triggering psychiatric illnesses and having an altogether very harmful effect on the entire organism.
One might speculate that the efficacy of the treatment in GHT is in reducing the chronic stress levels of the patients across multiple pathways. That would align with our findings of a general slight decrease of all somatic medication, but mainly with the significant decrease of drugs targeting the renin-angiotensin system, depression, diabetes and acid-related disorders. Further studies that provide all of these data are needed to prove these assumptions.
The concept of GHT affects chronic stress in various ways. First, more intensive treatment results in faster medication adaptation. The resulting improvement in the condition and the easing of related anxieties reduces the general stress level. In addition, the frequent contacts and involvement of social work lead to a significant improvement in loneliness, as well as a better socioeconomic situation (which is currently rather unfavourable, especially for older women in Austria). Worries about physical condition, social and economic insecurity, and loneliness are each massive triggers of chronic stress. The relationships connected to GHT seem to have a stabilising effect on patients.
GHT can make a difference which could explain the elusive effect on psyche and physis. Future research in this direction is urgently required to provide more clarification about the mode of action.
Comparison with the existing literature
As confirmed in other studies,Reference Ohrnberger, Fichera and Sutton7,Reference Kisely and Goldberg10,Reference Firth, Siddiqi, Koyanagi, Siskind, Rosenbaum and Galletly12 there is an association between mental and physical health. The bidirectional relationship between depression and hypertension is well known.Reference Goldstein, Carnethon, Matthews, McIntyre, Miller and Raghuveer33–Reference Meng, Chen, Yang, Zheng and Rutai35 Late-life depression is associated with a higher risk of both all-cause and cardiovascular mortality.Reference Wei, Hou, Zhang, Xu, Xie and Chandrasekar36 Traumas in old age lead to psychiatric symptoms, mainly in the form of anxiety disorders, affective disorders and substance-related disorders, and to physical symptoms like chronic pain, greater frequency of hypertension and cardio-ischemic diseases.Reference Chaudieu, Norton, Ritchie, Birmes, Vaiva and Anselin37,Reference Kütemeyer38 Clinically, multiple somatisation is more common than psychological symptoms.Reference Kütemeyer38,Reference Al Busaidi39 Effective factors (e.g. gate-keeper function, management in physical and mental multimorbidity) identified by Firth et alReference Firth, Siddiqi, Koyanagi, Siskind, Rosenbaum and Galletly12 are considered in GHT. Moreover, older people benefit mentally and physically from frequent contact with health servicesReference Troya, Babatunde, Polidano, Bartlam, McCloskey and Dikomitis40 in the form of therapeutic relationships,Reference Klug, Hermann, Fuchs-Nieder, Stipacek and Zapotoczky27 which was confirmed in the present study.
However, in contrast to other studies,Reference Klug, Hermann, Fuchs-Nieder, Panzer, Haider-Stipacek and Zapotoczky5,Reference Vulser, Vinant, Lanvin and Chatellier41,Reference Stulz, Wyder, Maeck, Hilpert, Lerzer and Zander42 there was no positive treatment effect concerning the number of hospital admissions and length of hospital stays, which might also be because of the very small number of in-patient cases, as mentioned above.
Strengths and limitations of the study
The main strength of this study is the comparability of data on psychiatric symptoms, general health and medication in GHT and TAU by using a large data-set from a national health insurance database.
Especially the cross-sectoral analysis of the patient behaviour of both groups enables a holistic view of the medical care for older people with mental illness. This approach encompasses intra- and extramural care, as well as the entire medical treatment for this group of patients. A further strength refers to the fact that there are only a few studies trying to link physical health and the effectiveness of a psychiatric treatment model.
This study has several limitations that should be taken into consideration. First, there was a difference in the team settings concerning urban and rural regions because of the non- availability of special occupational groups in the rural regions.
A certain limitation is the small case number concerning specialists and hospital stays.
The statistical projection for those patients in the intervention group who did not have a continuous treatment with GHT in the whole of 2016 might also be a limitation.
Finally, concerning matching, future studies might also want to consider further important variables such as mental and physical health status in the pre-study period.
Implications
The present study demonstrates a direct link between a multi-professional out-patient psychosocial treatment and physical health. To our knowledge, this is one of the first studies in this particular field.
The outstanding feature of GHT is the very individual and target-oriented treatment and support compared with usual treatment models. All therapies and social support are coordinated regarding content and time, and the effectiveness is continuously evaluated by the team members. The changes in prescription behaviour (reduction in quantity and type; polypharmacy) have a high potential to positively influence general health. In this way, possible side-effects and adverse effects of medicinal long-term therapies can be minimised. However, in this context it should be mentioned that although polypharmacy is undoubtedly a frequent problem in the elderly, undertreatment with regard to indicated drugs may be observed as well (see also O'Mahony et alReference O'Mahony, O'Sullivan, Byrne, O'Connor, Ryan and Gallagher43).
GHT seems to reduce chronic stress levels. It certainly needs further studies, with larger sample sizes and longer observation periods, to confirm the findings of the present study.
There is also a need to explore differences in effects depending on the diagnosis and severity of the disease.
The complexity of the relationships between health factors underlines the need for complex interventions and increased implementation of psychosocial treatments like GHT. Overall, GHT has great potential to improve both mental and physical parameters.
Funding
This study was funded by the Health Care Funds of Styria. The funder had no role in conducting the study.
Acknowledgements
We would like to thank the Health Care Funds of Styria and the Austrian Health Insurance Company – RMIC for help with data retrieval; and all colleagues at the PSS Gesellschaft zur Förderung seelischer Gesundheit GmbH, Rettet das Kind Steiermark and Hilfswerk Steiermark, for help with data collection. We also thank Professor Stefan Priebe (Unit for Social and Community Psychiatry, Queen Mary University of London) for his valuable comments on the manuscript.
Data availability
Single data-sets were made available by the Social Insurance Company, Health Care Funds of Styria and PSS; the cross-sectoral data were made available by the Institute for Health Care Strategies (guaranteed data destruction at the end of the project – official requirement to destroy the Social Insurance data). Data is available only upon new request by the data holders.
Author contributions
C.P. contributed to the conception and design of the study, project management, analysis and interpretation of the data, and drafting the manuscript. G.F. contributed to the conception and design of the study, analysis and interpretation of the data, and drafting the manuscript. W.H. contributed to the conception and design of the study, and drafting the manuscript. M.S. and G.H. contributed to scientific counselling, interpretation of the data, and drafting and revising the manuscript. G.K. contributed to scientific counselling, supervising data collection, interpretation of the data, and drafting and revising the manuscript. All authors have approved the final version of the manuscript.
Declaration of interest
None.








eLetters
No eLetters have been published for this article.