Congenital complete atrioventricular block is associated with CHD in 14%–42% of cases, while the remaining cases are isolated complete atrioventricular block. Reference Brucato, Cimaz and Caporali1 Ninety-one per cent of isolated complete atrioventricular block cases are associated with maternal autoimmune disorders, such as systemic lupus erythematosus and Sjögren’s syndrome, and 9% are idiopathic or other channelopathies. Reference Pruetz, Miller and Loeb2 Patients with isolated complete atrioventricular block often remain asymptomatic during infancy but require immediate pacemaker treatment if severe symptoms develop. Complete atrioventricular block with complex CHD is often associated with heart failure and requires pacemaker treatment at birth. Congenital complete atrioventricular block in single-ventricular patients has a high mortality rate and requires immediate intervention after birth. Some authors have reported that it is very difficult to conduct transvenous pacing via the femoral vein or internal jugular vein in neonates; however, the umbilical vein approach is simple and useful. Reference Hanséus, Sandström and Schüller3,Reference Li, Zhang and Li4 A few reports have detailed emergency pacing via the umbilical vein of neonates. None have described neonates with complex CHD.
Case report
Case 1
The first patient was a boy who was born to a healthy couple. The mother tested negative for self-antibodies. At the 28th gestational week, the patient was diagnosed with fetal bradycardia with a heart rate of 50 beats/min and congenital complete atrioventricular block. At 36 weeks, he was born via emergency cesarean section because of fetal pleural effusion. His birth weight was 2634 g and Apgar score was 8.9. His neonatal heart rate was 42 beats per minute, percutaneous oxygen saturation was 87%, and blood pressure was 67/42 mmHg. Electrocardiography revealed congenital complete atrioventricular block with a heart rate of 40–50 beats per minute, and QRS duration was 100 ms (Fig 1). Postnatal echocardiography revealed normal cardiac anatomy and noticeably decreased left ventricular ejection fraction (25%). A chest X-ray showed cardiac enlargement, and blood tests showed an elevated B-type natriuretic peptide level of 2472 pg/mL. Isoproterenol was immediately administered, but was ineffective, and we decided to proceed with ventricular emergency pacing via the umbilical vein.
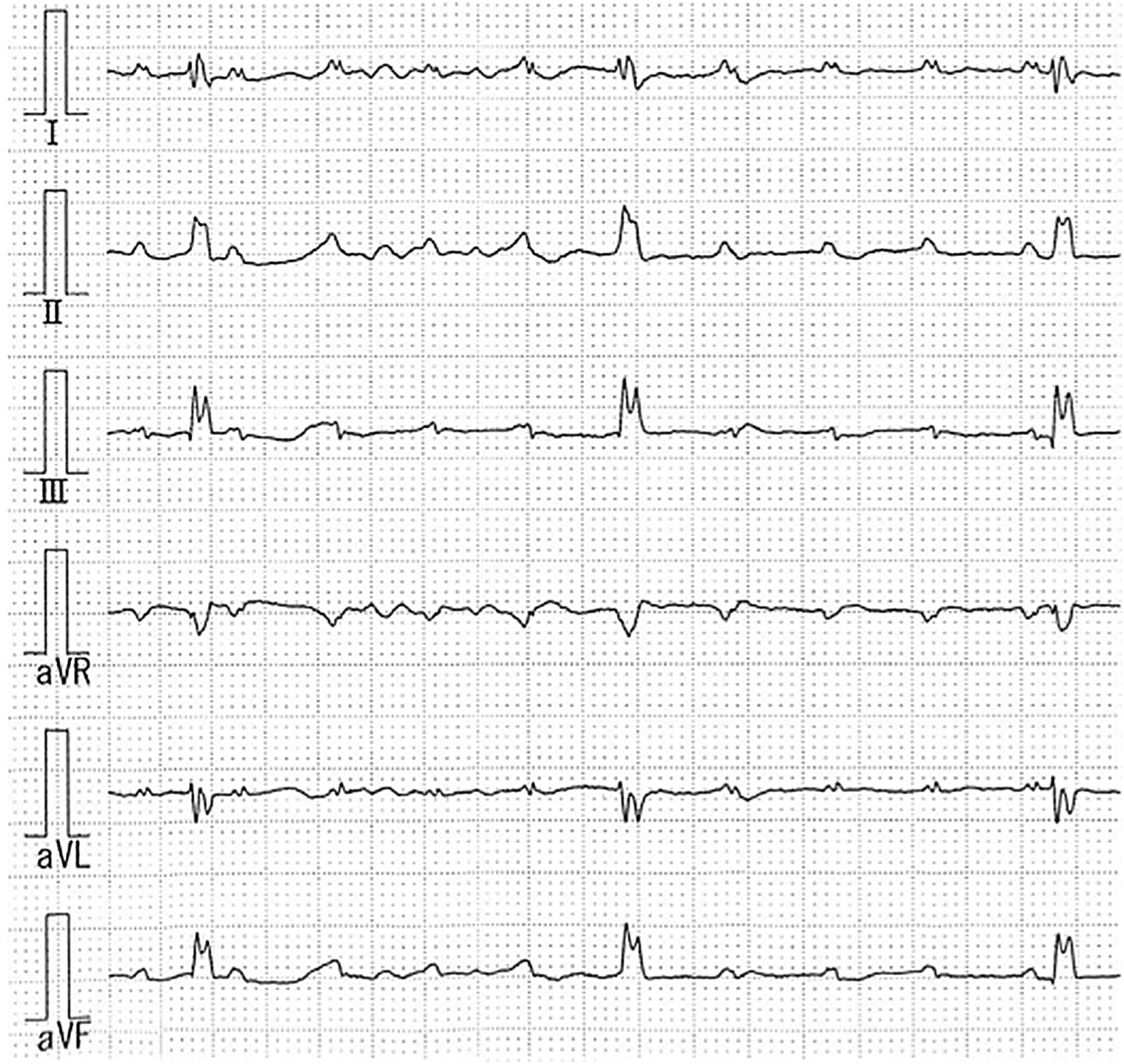
Figure 1. Electrocardiogram showing complete atrioventricular block before the temporary pacing.
We catheterised the umbilical vein using a 5-Fr single-lumen umbilical vein catheter and advanced the catheter into the right atrium under echocardiographic guidance. An EPstar (Japan Lifeline, Tokyo, Japan) 2-Fr fixed electrophysiology catheter (four electrodes; 5 mm in diameter) was easily inserted and placed directly into the right ventricle (Fig 2). After connecting to an external pacemaker running at a stimulation rate of 110 ppm, the left ventricular ejection fraction improved slightly to 35%. Under moderate sedation, heparin 10 U/kg/h was administered continuously as antithrombotic therapy.

Figure 2. X-ray showing 2-Fr fixed electrophysiology catheter in the right ventricular.
Thereafter, pacemaker implantation was performed at 4 days of age when his weight was 2477 g. A steroid-eluting epicardial lead tip was positioned on the right ventricular wall. Measurements of its position revealed a stimulation threshold of 3.5 V @ 0.40 ms, a sensing threshold of 2.8 mV and a lead impedance of 200 Ω. An additional lead loop was left in the pericardial cavity to allow further growth. A pulse generator (Medtronic Adapta ADSR01; ventricular pacing (VVI) rate, 120 beats/min) was placed in the subcutaneous pocket embedded in the abdominal wall (Fig 3A, B). Paced QRS duration was 100 ms. A beta-blocker and angiotensin-converting enzyme inhibitor were started, and he was discharged at 1 month and 8 days of age.

Figure 3. (a) X-ray image showing the permanent VVI pacemaker implanted in the neonate 4 days after birth; (b) electrocardiogram showing pacing signals after VVI pacemaker implantation.
Case 2
The second patient was a girl who was born to a healthy couple. The mother tested negative for self-antibodies. At the 27th gestational week, she was diagnosed with a complete atrioventricular septal defect, hypoplastic left ventricle (functional single ventricle), and pulmonary stenosis. She had fetal bradycardia with a heart rate of 60 beats per minute, and she was diagnosed with congenital complete atrioventricular block. Subsequently, the fetal heartbeat decreased to 50–60 beats per minute, and there were no signs of fetal oedema. She was born via scheduled cesarean section at 36 weeks and 4 days of gestation.
The patient’s birth weight was 2750 g, and Apgar score was 6.7. The neonatal heart rate was 60 beats per minute, percutaneous oxygen saturation was 81%, and blood pressure was 50/34 mmHg. Electrocardiography revealed congenital complete atrioventricular block with a heart rate of 55–60 beats per minute, and QRS duration was 60 ms (Fig 4). Postnatal echocardiography revealed a complete atrioventricular septal defect with situs inversus, d-loop ventricles, d-malposition of the great arteries {I.D.D}, a hypoplastic left ventricle, severe pulmonary stenosis, a double-outlet right ventricle, mesocardia, and a noticeably decreased left ventricular ejection fraction (30%). A chest X-ray showed cardiac enlargement, and blood tests revealed an elevated B-type natriuretic peptide level of 447 pg/mL. We diagnosed the patient with heterotaxy based on structural defects. Isoproterenol was immediately administered, but it was ineffective, and we decided to proceed with ventricular emergency pacing via the umbilical vein.

Figure 4. Electrocardiogram showing complete atrioventricular block before the temporary pacing.
However, 30 min after her birth, we attempted to catheterise the umbilical vein via a 5-Fr single-lumen umbilical vein catheter and advance the catheter into the inferior vena cava under echocardiographic guidance. Subsequently, a chest radiograph showed that the umbilical vein was located on the left side of her body, and abnormalities in the umbilical vein were suspected (Fig 5). We determined that inserting the catheter under echocardiographic guidance was dangerous and chose fluoroscopic guidance instead. Angiography showed that the umbilical vein flowed into the left portal vein and then bent to the right, connecting it to the ductus venosus (Fig 6). Strong flexion of the inflow from the umbilical vein to the portal vein was the suspected cause of insertion difficulty. Therefore, a 5-Fr sheath was inserted into the umbilical vein, and an EPstar 5-Fr fixed electrophysiology catheter (two electrodes; 10 mm in diameter) was inserted and placed directly into the right ventricle using the guidewire (Fig 7). After initiation of VVI pacing, stable circulatory dynamics were achieved, and no pacing failure due to body motion occurred. After connection to an external pacemaker at a rate of 120 beats/min, the patient’s clinical status improved immediately. The catheter was sutured to the umbilicus and secured with gauze and tape. Under moderate sedation, heparin (10 U/kg/h) was administered continuously as an antithrombotic therapy, and cefazolin (40 mg/kg/day) was administered to prevent infection.

Figure 5. X-ray showing the umbilical vein positioned on the left side of the patient’s body.

Figure 6. Fluoroscopy image showing that the umbilical vein (UV) flowed into the portal vein (PV) and then bent to the right to connect to the ductus venosus.

Figure 7. X-ray showing the temporary pacing via the umbilical vein in the eonate at 3 hours after birth.
Thereafter, pacemaker implantation was performed at 17 days of age when her weight was 2776 g. A steroid-eluting epicardial lead tip was positioned in the right ventricular wall close to the interventricular septum (Fig 8). Position measurements revealed a stimulation threshold of 0.6 V @ 0.58 ms, a sensing threshold of 4.0 mV, and a lead impedance of 664 Ω. An additional lead loop was left in the pericardial cavity to allow for further growth. A pulse generator (Abbott Solus-µII; VVI rate, 120 beats/min) was placed in a subcutaneous pocket embedded in the abdominal wall. Paced QRS duration was 120 ms. On the 29th post-operative day, the patient fully recovered and was discharged. In the 4-month follow-up period, she progressed well, and at 5 months of age, she underwent bidirectional Glenn surgery.

Figure 8. (a) X-ray image showing the permanent VVI pacemaker implanted in the neonate 17 days after birth; (b) electrocardiogram showing pacing signals after VVI pacemaker implantation.
Discussion
The incidence of congenital complete atrioventricular block is approximately 1 in 20,000 birth. Reference Brucato, Cimaz and Caporali1,Reference Pruetz, Miller and Loeb2 Isolated congenital complete atrioventricular block is a passively acquired autoimmune disease of the fetus. Implantation of a pacemaker is recommended for symptomatic patients and for asymptomatic patients presenting with profound bradycardia, left ventricular dysfunction, a wide interval, or a prolonged QT interval. Reference Bordachar, Zachary and Ploux5
Heterotaxy syndrome is an uncommon disease that comprises 0.4%–2% of structural heart disease cases and affects 1–2/10,000 live births. Reference Lim, McCrindle and Smallhorn6,Reference Escobar-Diaz, Tworetzky and Friedman7 A complete atrioventricular block is commonly associated with heterotaxy syndrome. Reference Lim, McCrindle and Smallhorn6–Reference Buca, Khalil and Rizzo9 Patients with heterotaxy syndrome, and atrioventricular block, or bradycardia diagnosed prenatally have a low survival rate (63%). Reference Lim, McCrindle and Smallhorn6 Although the survival rate of patients with heterotaxy syndrome has improved in recent years, its prognosis is suboptimal. Hydrops, cardiac dysfunction, prematurity, and low ventricular rates are predictors of death. In neonates with isolated congenital complete atrioventricular block, pacemaker implantation is recommended if the patient develops severe heart failure or if the heart rate is < 55 beats per min. Reference Bordachar, Zachary and Ploux5,Reference Brugada, Blom and Sarquella-Brugada10 Guidelines indicated permanent pacemaker implantation in neonates/infants with complete atrioventricular block and complex CHD when bradycardia is associated with haemodynamic compromise or when the mean ventricular rate is <60–70 bpm. Reference Shah, Silka and Silva11 There is a report of two fetuses with cardiac dysfunction, both of whom had complete atrioventricular block in heterotaxy with ventricular rates of <55 beats per minute and died in utero soon after the diagnosis of hydrops was made. Reference Escobar-Diaz, Tworetzky and Friedman7
For patients with severe heart failure, like these cases, who require emergency postnatal pacing, permanent pacemaker implantation immediately after birth is invasive, and temporary pacing using the umbilical vein approach is a good way to manage heart failure. Fuchigami et al reported a staged approach to pacing in high-risk newborns/infants, as with temporary epicardial wires. Reference Glatz, Gaynor and Rhodes12,Reference Fuchigami, Nishioka and Akashige13 Temporary pacing using the umbilical vein approach is a less aggressive procedure in the immediate postnatal period, but it should be performed with caution and attention to vein perforation due to abnormal venous anatomy, thrombosis, infection, and dislodgement, etc. Nakanishi et al reported the limitation of temporary pacing via the umbilical vein of a very low-birth-weight infant because the infant’s umbilical vein was too narrow to insert the lead. Reference Nakanishi, Takahashi and Kawasaki14 Our policy is to perform pacing via the umbilical vein in patients requiring emergency postnatal pacing. The advantage of pacing via the umbilical vein is the relative ease of catheterisation. The catheter is advanced from the inferior vena cava into the right atrium under echocardiographic guidance, and endocardial pacing provides stability. The disadvantages are that the catheter passes through a fragile vein and requires careful handling, whereas the pacing catheter requires fixation. In Case 2, the umbilical vein flowed into the venous duct through the portal vein and directly into the right atrium. We could not advance the 5-Fr single-lumen umbilical vein catheter into the inferior vena cava under echocardiographic guidance because the junction of the umbilical vein with the portal vein was acutely bent at an acute angle. It was possible to safely place the electrode catheter and perform pacing under fluoroscopic guidance. Considering that there are such cases when pacing using the umbilical vein approach is performed, the technique should be performed cautiously with attention to the perforation.
Permanent cardiac pacemaker treatment in infants and children has improved considerably over the past two decades, mainly due to a combination of a more suitable size of the newer-generation pulse generators, better leads, and refinements of the implantation technique. Although transvenous pacing is now well established, even in small children, recommendations for infants remain under discussion because of the anatomical limits resulting from low body weight. In Case 1, the placement of a pacing lead onto the left ventricle (LV) wall was considered invasive and difficult due to the posterior LV position; therefore, the lead was placed in the right ventricular free wall. In this case, the lead position was subsequently changed to that of the left ventricle at 1 year and 9 months old because of ventricular dyssynchrony with pacemaker. We should have placed a pacing lead onto the LV wall because with an epicardial approach, LV pacing seems to preserve LV systolic function better than other pacing sites. Reference Janousek, Van Geldorp and Krupickova15,Reference Silvetti, Muzi and Unolt16 In Case 2, the epicardial lead position was located in the right ventricular wall close to ventricular septum whenever possible. In both the cases, a bipolar lead was implanted to prevent oversensing. We chose the ventricular rate response pacing (VVIR) system because of the pocket size, and the rate of ventricular capture in both cases was 100%. In the future, we plan to upgrade this system to a dual-chamber system.
Acknowledgements
None.
Financial support
The authors received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.











