Introduction
This chapter will review the societal and political context in which there was an evolution of approaches to address the mental health needs of children and young people.1 In the 1960s and 1970s, stimulated by socio-cultural changes, new innovations in therapeutic approaches were introduced, including family therapy and cognitive behavioural therapy (CBT). The first major longitudinal and epidemiological research studies were carried out. In the 1970s and 1980s, there were challenges to the state’s capacity to deal with a variety of social problems and various forms of child maltreatment were identified. A national multidisciplinary assessment and management framework was introduced aimed at protecting the child, supporting families and developing appropriate treatment initiatives. In the 1990s and 2000s, further interventions were developed to reverse the impact of social exclusion – for example, Sure Start. There was a consolidation of practice, including both general and highly specialised services, and further development in research and training.
The Societal Context: 1960s and 1970s
During the post-war years, the promotion of national growth and well-being had been a priority with the establishment of the National Health Service (NHS) and the welfare state.2 Then, as a result of post-war fertility and the baby boom, demographics tilted towards youth; by the 1960s and 1970s, fuelled by the ‘youth culture’, there was a marked change towards an anti-establishment cultural phenomenon in the Western world. Disaffected young people rebelled against the Vietnam War. Socially progressive values grew, encompassing feminism, women in leadership roles, environmentalism, civil rights, a sexual revolution relaxing social taboos, easier birth control, repeal of sexist laws and gay liberation. There were also increasing stresses, family break-ups, divorce and single parenthood.
Traditions: Child and Adolescent Psychiatry in the 1960s and 1970s
The Child Guidance Movement
The child guidance clinic model was established in the 1930s: the ‘trinity’ of a psychiatrist seeing the referred child, a social worker engaging with the mother and an educational psychologist testing the child and liaising with the school.3 Many child and adolescent psychiatrists underwent psychoanalytic training. Psychiatric social workers trained in casework skills and educational psychologists had a background in teaching.
Regular sessions were offered to the child or young person, promoting an attachment through a child-centred approach, using play and artistic materials to encourage the expression of feelings. The approach gave the child the experience of an adult creating a warm, positive attachment and facilitated reflecting on their lives, sharing traumatic and stressful events and trying to make sense of their anxieties and depressed mood as well as managing behaviours, solving problems and finding solutions. Casework with mothers to support them in the challenging task of parenting provided an opportunity for mothers to reflect on their own experiences, current and historical stresses, and relationships, which were influencing their parenting. They were helped in managing their children’s challenging behaviour as well as being emotionally responsive and understanding. The psychologist supported the child or young person in the educational context. By 1970, there were 367 clinics in the UK.
Child Psychotherapy
There was significant controversy in working therapeutically with children and young people.4 Anna Freud’s approach at the Hampstead Clinic emphasised the supportive ‘ego-strengthening’ role of the therapist and the use of play materials, games and activities to promote growth and resilience. Kleinian approaches at the Tavistock Clinic centred on the object-relations, transference and counter-transference interpretation of children’s play and responses to the therapist in order to resolve early sources of anxiety and promote maturation.
Winnicott, a paediatrician and psychoanalyst who gained renown from his wartime broadcasts, supported an independent/‘middle’ group approach – illustrated through his demonstrations of ‘squiggle’ drawing encounters with children. The child and the therapist challenged each other to turn a shape into an image, thus reflecting experiences which could be built on as part of a creative encounter. Winnicott built on the notion of transitional space underpinning play and creativity (see also Chapter 15).5
The Association of Child Psychotherapists, established in 1949, fostered different approaches and maintained a continuity of traditions of training in working intensively with children, adolescents and young people. Work developed with special populations of children – in residential and care contexts and with autistic spectrum disorders and learning/intellectual disability. Related creative forms of therapeutic work have developed – play therapy, art and music therapy and educational therapies.
Innovations: 1960s and 1970s
Developments of Family Therapy and Multidisciplinary Practice
Although effective, the child guidance clinic model proved static and unresponsive to the changing societal dynamics. A striking development was the growth of family therapy.6 Bowlby introduced family meetings to reinforce individual therapy; Skynner, a group analyst, worked with the family as a group. A seminal paper by Bateson, ‘The Double-Bind Theory of Schizophrenia’, in 1962, asserted that disordered communication led to pathological outcomes. Children’s mental health difficulties were triggered and maintained by pathological family interactions. Minuchin developed ‘structural’ approaches, working with family communications, boundaries and alliances aiming to alter interactions between family members and improve the functioning of the child. The model was transmitted widely by videos of therapeutic work, large-scale dramatic demonstrations and public media forums, an approach which contrasted vividly with traditional more private and reflective approaches.
Therapists were trained in experiential approaches such as ‘moving family sculptures’ and ‘role play’ to facilitate the development of skills and understanding. Live supervision of clinical work took place through one-way screens and electronic bugs in the ear. Despite reservations, there was an enthusiastic take-up of the approach. Child and adolescent psychiatrists, psychologists and social workers started working with families and collaborated to establish training, which led to the founding of the Association of Family Therapy in 1976, rebalancing the dynamics between the different professionals. Therapeutic skills could be developed and effective therapy delivered to children and their families by a range of professionals across health and social care as well as education.
Developments in Cognitive Behavioural Therapy (CBT)
CBT emerged as an amalgam of behavioural and cognitive theories of human behaviour.7 Behavioural therapy had been developed in the 1960s and included Patterson’s parent-training model, introducing consistent approaches to managing challenging disruptive behaviour. An increased awareness of the role of cognition led to the transition to CBT in the 1970s. Internal thought processes (e.g. self-talk) began to be viewed as both targets and mechanisms of change, with an emphasis on improving cognitive skills linked with modifying behaviour. Self-instruction emerged to teach impulsive children how to control their behaviour.
Psychological disorders were attributed to maladaptive cognitive processes, with psychological vulnerabilities developing as a result of early socialisation experiences within the family. Specific CBT approaches for children and young people incorporated parent training and the development of children’s mastery over their own environment. Specific protocols emerged for the treatment of anxiety and depression, trauma-focused CBT and parent training. The Triple P and Incredible Years programmes have been widely adopted. CBT has become a well-established, online, self-guided approach, which is as effective as face-to-face treatments in appropriate circumstances.
Developments in Research and Practice in Child and Adolescent Mental Health
Attachment
Bowlby’s 1951 review of maternal deprivation in Maternal Care and Mental Health had a significant influence on the development of research in the field.8 He highlighted the core role of maternal attachment for the secure development of the child. Psychoanalytic colleagues criticised his emphasising the role of real-life experiences rather than the inner world. Rutter praised positive consequences, for example parents staying with their children in hospital but echoed feminist criticisms that even brief daily maternal separations were assumed to be harmful.9 He observed that the controversy generated empirical research about children’s development, family relationships and the importance of good-quality alternative care. The ‘attachment’ concept has played a key role in professional and public awareness about the care of children and the security and organisation of attachment and mental health and as a target for therapeutic work.
Research Methodologies, Assessment and Measurement
Assessing and measuring the nature, extent and severity of mental health difficulties is an essential component of research and practice.10 Questionnaires, interviews and observational approaches help to identify the presence of disorders, including depressed mood, anxiety, traumatic responses, anti-social behavioural symptoms and concentration difficulties.
Longitudinal research identified cohorts of children at birth followed through to adulthood, establishing continuities of mental health disorders between childhood, adolescent and adult life, identifying harmful and protective influences on development. Following the development of children through to adulthood has also been a popular theme in TV documentaries.
The 1970 Isle of Wight Study, led by Rutter,11 was a key development in epidemiological research, demonstrating the value in screening whole populations and interviewing children, adolescents, young people and families. The epidemiological model has examined many influences on children and young people’s development, including prenatal factors, smoking and alcohol misuse; family factors – parental mental health, neglect and abuse, separation and divorce; and community and school influences. This knowledge has influenced public health, preventative approaches, support for parenting and clinical practice.
Measures of family and parenting relationships include attachment quality and parenting capacity. The Multiaxial Approach to Diagnosis, introduced in 1975, provided a way to describe complexity – the nature of the presenting disorder, the level of intellectual functioning, medical factors and the psychosocial factors, including family characteristics. Assessing the effectiveness of therapeutic approaches in research and practice enhances professional and public awareness of the value of treatments.
Specific Disorders of Emerging Public Interest
Self-harming suicidal behaviour, anorexia nervosa, and other eating disorders are the main mental health conditions in young people which can lead to death.12 Widely publicised tragic cases of young people with talent and promise self-harming – cutting, over-dosing, killing themselves – led to demands for improved and accessible mental health services. Increasing numbers of young people were presenting with self-starvation, distorted body image and a fear of fatness, associated with obsessive self-control of eating and calorie counting. There is continuing debate about societal aspirations for an idealised slim body shape and young people identifying with models or dancers.
Autistic disorders and attention deficit hyperactivity disorder (ADHD) are key neurodevelopmental disorders. Rutter delineated autism as a separate, specific disorder with deficits in social skills, empathy, problems of speech and non-verbal behaviours as well as repetitive stereotyped behaviours.13 High-functioning individuals were identified with Asperger’s syndrome and sometimes showed areas of abilities, talents and exceptional skills – for example, mathematical, musical and artistic, an interest fostered by films and TV series.
ADHD is a neurodevelopmental disorder with a classic pattern of short attention span, inattentiveness, hyperactivity, and impulsiveness, and is recognised in schools and families.14 Treatment with psychostimulants improved concentration and educational attainment and demands for treatment followed, evoking controversy about the potentially harmful effects of medication in general and on children’s growth and development.
The Recognition of Child Maltreatment: 1970s and 1980s
The Battered Child
A key to recognising child maltreatment was the publication in 1962 of Kempe and colleagues’ highly influential paper ‘The Battered-Child Syndrome’.15 Images of bruising and broken bones focused the thinking of child health practitioners worldwide. The sequence of identification in society of different forms of maltreatment followed:
Physical abuse – burns, fractures and bruises; a child ‘deserving punishment’
Neglect and failure to thrive – unawareness of the needs of the child
Emotional abuse – rejection and scapegoating
Exposure to violence – domestic violence and abuse
Sexual abuse – sexual interest and exploitation of the child and young person.
There was also the recognition that a rare unintended consequence of mothers staying with children in hospital was that, despite appearing loving and close, some came to be understood as seeking support through having a sick child. Symptoms could be falsified or exaggerated, resulting in factitious illness states – Munchausen’s syndrome by proxy or non-accidental poisoning.16
Epidemiological research revealed the extent of maltreatment, its under-reporting and the long-term impact on physical and mental health.17 Finkelhor described ‘polyvictimisation’, the exposure to multiple forms of maltreatment over childhood.18 As maltreatment can be defined as a criminal action, a social problem or a health disorder, a multidisciplinary response was advocated, led by social services. Practitioners from the police, health and social care and education were encouraged to ‘Work Together’ to recognise the signs of child maltreatment, carry out the necessary assessments, ensure the child or young person is protected though legal processes if necessary and provide intervention to help the child and family. This included appropriate treatment for complex parental mental health issues, including alcohol and substance abuse. Prosecution was reserved for the most serious injuries. There was increasing awareness of the intergenerational traumatic impact on children’s health and development and the need to provide a range of therapeutic interventions.
Recognition of Sexual Abuse
Our survey of professionals working with children in 1981 revealed that the sexual abuse of children was recognised as a crime not a focus of child protection,19 an attitude which has persisted. Following wider publication on the issue, many individuals who had suffered sexual abuse and exploitation in silence came forward to speak about their persisting traumatic experiences. There is continuing evidence about the pervasive impact of harmful sexual exploitation of vulnerable children by individuals with power – in families, communities, churches, schools, sports and entertainment.
A family and group treatment programme was established at Great Ormond Street Children’s Hospital in 1981,20 providing diagnosis and treatment for children, male and female victims, young people, protective mothers and abusive young people and parents. A rehabilitation approach based on family systemic principles was initiated, including, where possible, individuals in prison, who could take responsibility directly for abusive behaviour, albeit with stringent safeguards. A BBC Horizon documentary ‘Prisoners of Incest’ in 1984 demonstrated the approach but was controversial from feminist perspectives that raised concerns about an inappropriate accommodation to perpetrators, who were at risk of continuing abusive behaviour.
Public Recognition of Maltreatment
The reality of child maltreatment was brought home by the tragic case in 1974 of Maria Colwell, a child subjected to extensive physical abuse.21 This was the first in a series of thirty public inquiries into serious child maltreatment, with the most recent being Victoria Climbié in 2000 and ‘Baby P’ in 2009. There was extensive media coverage, detailed accounts about what had gone wrong and questioning of the current state of policy and practice. Social work professionals who had been made responsible for child protection were named, vilified and harshly criticised for accommodating to parents, failing to recognise and not using their statutory powers to protect children.
The secrecy and threat associated with sexual abuse make diagnosis through interviews and physical examination complex and challenging. In 1986, the paediatricians Hobbs and Wynne described a series of sex rings in a northern city and the criteria for diagnosis of boys and girls who had sustained anal abuse.22 The Cleveland affair in the summer of 1987 focused on the work of two paediatricians and a social worker.23 More than 100 children had been removed from their families over a short period, based in part on physical findings associated with possible sexual abuse. The findings were fiercely criticised as dubious in the media and parliament. The widely reported inquiry that followed highlighted the risk of professional intervention on questionable grounds and criticised the ‘over-enthusiastic’ use of medical science. The inquiry supported the rights of parents, in practice, undermining the attempts of practitioners to find ways to amplify the voice of the child who had been silenced. Our facilitative approach to interviews using anatomically correct dolls was also challenged.
Social Context: The Children Act
Implicit in the narrative of failure, incompetence and ‘over-zealous’ approaches to protect children were a criticism of social welfare approaches. The 1980s were characterised generally by an increasing disillusionment with the ability of the social democratic state to manage the economy and overcome a range of social problems. There was a rise in violence and a decline in social discipline. An alternative, individualised concept of relationships and market forces was advanced, aimed at shrinking the state. The family was seen as a predominantly private domain, excluding the state unless violence was being perpetrated.
This thinking underpinned the establishment of the Children Act 1989.24 The Act provided a legal framework which emphasised the importance of providing support for families and established criteria for a child being at risk of ‘significant harm’ to justify removal from a parent’s care. Mental health professionals played a key role in helping the courts understand the risks, the prospects for rehabilitation, the provision of treatment services and the possibility of the need for alternative care or, ultimately, adoption.
In parallel, the United Nation’s Convention on the Rights of the Child (1989) was established to ensure that services were provided to enable children to participate in society, to have a voice and to be protected from violence and exploitation.
Consolidation of Mental Health Services for Children, Adolescents and Young People: 1990s to 2010
Social Policy Context
This period was marked by the last phase of Thatcherism, which extended market rationalities and focused on the individual rather than governing through society.25 New Labour from 1997 to 2009 espoused the ‘third way’, combining individualism and egalitarianism and thus reconciling apparently conflicting cultural projects: personal self-realisation and rights to autonomy; and membership and community. Initiatives focused on reversing social exclusion, stressing the need for early intervention and prevention, including the Sure Start and Children’s Fund programmes. Despite significant investment, there was no full-scale attempt to reduce social inequality, although more than a million children were lifted out of poverty. The final year of this period, following the financial crash, saw the re-election of a Conservative–Liberal Democrat coalition government destined to pursue a programme of austerity, a reduction in public services, shrinking of the state and a further drive towards the privatisation of public services.
Development of Services
By the 1990s, child and adolescent mental health had a higher profile in both the public and the professional worlds. More academic chairs and departments of child and adolescent psychiatry were established, and training and accreditation programmes were developed. Research developed across the fields, including in genetics, molecular biology and neurobiology (see also Chapter 16).26
A four-tiered framework of CAMHS (Children and Adolescent Mental Health Services) as a health service was established in 1995, replacing child guidance clinics:
Tier 1 Advice and treatment provided by practitioners working in a variety of settings in the community, in general practice, in schools and in agencies working with maltreated children – e.g. the NSPCC (National Society for the Prevention of Cruelty to Children).
Tier 2 Generic multidisciplinary teams – providing core community services for children, adolescents and young people.
Tier 3 Specialist multidisciplinary services.
Tier 4 Highly specialised services providing outpatient and inpatient care for young people presenting with early psychotic illness, eating disorders or displaying sexually harmful behaviour.
A highly specialised service that attracted much attention and controversy was the establishment of the Tavistock Gender Identity Development Service in 1989.27 Following rigorous assessments and therapeutic help, a young person’s wish to transition and develop their gender identity could be facilitated through medical and psychological intervention. During the controversy, it was asserted on the one hand that, lacking maturity, the deeply held wishes of young people should not be supported until they reached adulthood; on the other hand that there should be respect for the emerging individuality and autonomy of the young person.
The NHS organisation NICE (the National Institute for Clinical Excellence, later renamed as the National Institute for Health and Care Excellence) was established in 1999 and recommended the most effective approaches to help children and young people with mental health problems. The IAPT (Improving Access to Psychological Treatment) programme provided access to these effective therapies and was introduced to adult services in 2008 and children’s services in 2011.28 MindEd training was introduced to complement IAPT and to provide online training in emotional and behavioural ‘first aid’ and essential therapeutic skills.
One of the treatments recommended by NICE was the extensively researched CBT, with the risk that other modalities would be dismissed. Later research demonstrated that well-structured family/systemic or psychodynamic approaches were equally effective. In addition, much research focused on single disorders. The reality is that comorbid disorders are the rule rather than the exception. An alternative has been the development of integrative approaches, bringing different modalities together.29 The common treatment element approach identified and categorised common features of treatments which can be integrated to meet complex needs,30 an approach we adopted to reduce the harmful effects of all forms of maltreatment.31
Young Offenders Services
Young Offenders Services were established in 1998, with special school, youth courts, residential care and young offender institutions. However, the age of criminal responsibility remained at ten years. The world’s press had heard a blow-by-blow account of the killing of James Bulger by two vulnerable eleven-year-olds in 1993 in an adult court. Popular judgement was that the children were ‘evil’ and ‘devious’ and deserved to be in prison for life. Growing knowledge was ignored about the way the young person’s brain matures and responds to earlier trauma, undermining their capacity for judgement and control of impulsivity.
Our follow-up study of sexually abused boys demonstrated that sexually harmful adolescent or adult behaviour was more likely if they had also witnessed violence and suffered rejection.32 Attempts to change the age of criminal responsibility have been firmly resisted. The aggressive behaviour of adolescents and young people has continued to be a societal and media preoccupation – with gangs, knife crimes, bullying and ‘children who kill’.
Developments in Child Protection: Trauma-Informed Care
In 1988, in describing adverse childhood experiences (ACEs), Felitti and colleagues extended the concept of maltreatment to include household dysfunction and instability resulting from domestic violence; parental substance abuse; mental illness; imprisonment; and separation.33 They found that the more types of ACEs that individuals reported in their childhood (e.g. emotional, physical or sexual abuse; physical or emotional neglect; mother treated violently; household substance abuse or mental illness; incarcerated household member; and parental separation or divorce), the greater their risks of health-harming behaviours (e.g. smoking or sexual risk-taking) and both infectious and non-communicable diseases (NCDs), including substance abuse, mental health problems and violent behaviour.
The Framework for the Assessment of Children in Need and Their Families, in 2000, broadened the approach and provided a model for practitioners across children’s social care to describe the child’s needs in the context of parenting, individual and community factors. We were commissioned to develop and provide training in evidence-based approaches to assessment, analysis and intervention.34 Trauma-informed care in the community was introduced in 2005, integrating policies, procedures and practices as well as identifying potential paths for recovery.
The Internet: Beneficial and Harmful Influences
The World Wide Web, launched in 1989–90, gained massive popularity in the mid-1990s and was a near-instant communication aid and way of registering knowledge and information.35 The development of online therapeutic work and training has grown. Young people embraced the Internet, using it for social networking, communicating, expanding their interests, enriching their lives, entertainment, gaming, connecting and learning. Important issues, including gender identification as male, female or transsexual, could be debated. The Internet gives a voice to children and young people and may provide informal support and advice about managing specific problems, for example self-harm and anorexia.
The harmful impact of the Internet has also dominated social discourse, including exposure to age-inappropriate material online, pornography, violence or hate speech. Child pornography is circulated on the Web, and children may be groomed into creating and circulating images of sexual activities. Perpetrators have falsified their identities and groomed young people as a way of meeting and exploiting them sexually. Self-harm, suicide or anorectic behaviour can be encouraged online. Children and young people can abuse each other by sexting (sending sexual images, thus risking blackmail), cyber-bullying, harassment, disclosure of personal information or threats of social exclusion may trigger self-harm and suicidal responses.
The issue of the safety and control of the Internet is a constant and continuing theme. Childline, established in 1986, currently receives multiple calls about abuse over the Internet. Offenders can be helped anonymously to break the addictive cycle through ‘Stop it Now’.36 Children, young people and parents can be helped to understand the beneficial and harmful risks associated with internet use.
Conclusion
In their masterly review of the history of child and adolescent mental health 1960–2010 Rutter and Stevenson concluded: ‘there has been an amazing revolution in child and adolescent psychiatry … As a consequence, the body of knowledge, and the range of therapeutic interventions have increased in a way that would have seemed scarcely conceivable 50 years ago.’37 This review has confirmed these conclusions, focusing on the interface between society and mental health; promoting developments in therapeutic approaches and services to the community; and identifying and managing the pervasive and lifetime harmful impact of child maltreatment and adversity.
Key Summary Points
From the 1960s to the 1980s, in parallel to societal changes from welfarism to the counterculture, the legacy of the child guidance movement and psychodynamic approaches gave way to more active, transparent and fast-moving therapies. Family/systemic therapy involved the whole family and trained practitioners from all disciplines. Cognitive behavioural therapy (CBT) was developed as a new, effective psychological treatment.
Different longitudinal and epidemiological research approaches developed, providing a variety of ways of measuring the presence and impact of mental health problems. Conditions such as anorexia nervosa of childhood, self-harming and neurodevelopmental disorders – autism and ADHD – have been identified. These developments established a significant profile of child and adolescent mental health in professional practice and public awareness.
Despite attempts to ‘shrink the state’ in the 1980s, a continuing theme has been the recognition of the hidden yet pervasive traumatic impact of maltreatment many children suffer. The concept has been enlarged through the recognition of adverse childhood experiences (ACEs), adding exposure to family dysfunction and instability. There is a lifespan impact of adversity on mental and physical health and a need for a trauma-informed care approach.
Fostered by an investment in social inclusion in the 1990s to the 2000s, multidisciplinary Children and Adolescent Mental Health Services (CAMHS) were established, providing general to highly specialised treatment. Academic units promoted training and research in genetics and neurobiology. The National Institute for Clinical Excellence, later renamed the National Institute for Health and Care Excellence, gathered the growing research information on intervention and recommended best practice.
The introduction of the Internet in the 1990s has been both beneficial and harmful. The voice of the child as a person can be amplified, including the right to determine their gender. However, the Internet may also provide a route for some people to gratify inappropriate sexual interests in children and young people and to hurt them physically and emotionally. Safety and protection require constant vigilance.
Introduction
In 1960, mentally disturbed people over about sixty years of age were widely assumed to have irreversible senility. Little attention was paid to Martin Roth’s research which showed conclusively that mentally unwell older people were not all senile but suffered from a range of disorders. In the nomenclature of the time, those were affective psychosis, late paraphrenia, acute confusion and arteriosclerotic and senile dementia.1 Only two hospitals in the UK routinely offered older people thorough psychiatric assessment and treatment. One was a ward at the Bethlem Royal Hospital led by Felix Post, primarily for people suffering from ‘functional’ illnesses, mainly depression, schizophrenia and other psychoses. The other was a comprehensive old age psychiatry service, including day hospital, outpatient and domiciliary services, plus assessment, infirmary and long-stay wards, which Sam (Ronald) Robinson established at Crichton Royal Hospital, Dumfries.
This chapter aims to explain how Roth’s, Post’s and Robinson’s ideas gradually influenced clinical practice and service provision across the UK, shifting from typical custodial inactivity and neglect of patients assumed to be irreversibly senile to the creation of proactive ‘psychiatry of old age’ (POA) services. The chapter comprises two sections: 1960–1989 and 1989–2010. The first focuses on the development of the specialty until it was formally recognised by the Department of Health in 1989. It was the subject of my PhD thesis.2 Regarding the second section, I started as a senior house officer in POA in 1989. For this section, I have also drawn extensively on the Royal College of Psychiatrists’ (RCPsych) Old Age Faculty commemorative newsletter ‘21 years of old age psychiatry’ published in 2011.3 Although the essence of much National Health Service (NHS) policy is UK-wide, specific details and implementation plans may relate to one or more of the constituent countries. Given the brevity of this chapter, I have focused mainly on developments in England.
1960–1989
Liberal ideas about personal autonomy, choice and independence emerged internationally in the 1960s. New legislation in the UK on suicide, race relations, homosexuality and abortion reflected this. Changing agendas permitted younger people to make choices, even if risky, but older people were perceived as inevitably vulnerable and, despite their experience of life, their wishes were frequently ignored. According to Pat Thane, retirement was a mid-twentieth-century change which ‘increasingly defined old people as a distinct social group defined by marginalisation and dependency’.4 Alongside negative public perceptions, retirement was associated with a marked fall in personal income and reliance on the state pension.5 With poverty came disadvantageous health inequalities.6
In the early 1960s, more than a third of psychiatric hospital beds were occupied by people aged over sixty-five. The social scientist Peter Townsend identified many older people in long-stay accommodation who ‘possess capacities and skills which are held in check or even stultified. Staff sometimes do not recognise their patients’ abilities, though more commonly they do not have time to cater for them.’7 The sheer size of wards with up to seventy beds made providing satisfactory standards of nursing care almost impossible. These wards compared unfavourably with hotbeds of activity on those for younger people which used state-of-the-art medications, psychosocial, rehabilitative and therapeutic community approaches, and planned for discharge. After the Mental Health Act 1959 (MHA), with steps taken to begin to close the psychiatric hospitals and develop alternative services in the community and in district general hospitals (DGHs), younger people were discharged leaving older people behind.
For older people, clinically and scientifically, things edged on, albeit slowly. In 1961, Russell Barton and Tony Whitehead at Severalls Hospital, Essex, established a service based on Robinson’s at Crichton Royal. In 1962, Nick Corsellis demonstrated that senile dementia had the same pathology as Alzheimer’s disease: senility was therefore not just a worn-out ageing brain but a disease process requiring further research, aiming for prevention and cure. The same year, Post published an optimistic follow-up study of 100 older patients treated for depression.8 In 1965, his textbook of old age psychiatry,9 the first of its kind, was published, and the World Psychiatric Association (WPA) hosted an international symposium in London, Psychiatric Disorders in the Aged.10 These developments provide insights into clinical, epidemiological and neuroscience achievements at the time and indicate mounting interest in older people’s mental well-being. Neuropathology was discussed in terms of air encephalograms, post-mortems and electron microscopy. There were no validated brief cognitive assessment tools, and antidepressants consisted of tricyclics, monoamine oxidase inhibitors and electroconvulsive therapy. The WPA event included remarkable and charismatic leaders such as Post, Roth and Robinson, Tom Lambo (a Nigerian psychiatrist) and V. A. Kral of ‘mild cognitive impairment’ fame (who had survived incarceration in Theresienstadt Nazi concentration camp). Among the delegates were junior doctors Tom Arie, Klaus Bergmann, Garry Blessed and Raymond Levy, all inspired by the people they met and by the academic content.
Reports of scandalously low standards of care on long-stay wards in geriatric and psychiatric institutions reached the headlines in 1967 when Barbara Robb published Sans Everything: A Case to Answer (see also Chapter 7).11 Arie, dual trained in social medicine and psychiatry, and shocked by the Sans Everything revelations, applied for a consultant psychiatrist post to work with older people at Goodmayes Hospital, Essex (‘an unposh place … Most people thought I had taken leave of my senses!’).12 Arie’s team had a low hierarchical structure and high morale, able staff were eager to join it and patients began to get better.13 Arie wrote in 1971: ‘I have never before been in a professional setting where intellectual and emotional satisfaction go more closely hand in hand.’14
Arie and a few other newly appointed POA consultants, including Bergmann, Blessed, Whitehead and Brice Pitt – a ‘happy band of pilgrims’ as Pitt called them – began to meet as a ‘coffee house’ group. The group was in the right place at the right time: in the wake of Sans Everything, the government was taking more interest in the mental well-being of older people. Through Arie’s social medicine links, including being personally acquainted with the chief medical officer, the group ‘heavily influenced’ a Department of Health and Social Security (DHSS) blueprint, Services for Mental Illness Related to Old Age (1972).15 For the growing number of old age psychiatrists, this declaration of intentions became a bargaining tool to use with the DHSS or local NHS authorities when they failed to respond to identified needs.
Since, in most hospitals, younger people were discharged and older people were not, by 1973 almost 50 per cent of psychiatric hospital patients were over sixty-five,16 far in excess of the 14 per cent in the general population. Almost two decades after Roth’s research, undiagnosed but potentially treatable conditions contributed to this, particularly depression. This was also a personal tragedy, as Whitehead explained in the Guardian:
Old people may spend their last years in dreadful misery because severe depression has been wrongly diagnosed as senile decay … If you are anxious and depressed, and more and more people start treating you as if you were a difficult child, and you are finally incarcerated in a ward full of other elderly people who are being treated in the same way, it is likely that in time you will give up and take on the role of not just a child, but a baby.17
Two events in 1973 were central to the development of POA services: the coffee house group became the RCPsych Group for the Psychiatry of Old Age (GPOA; which in 1978 became the Section for the Psychiatry of Old Age (SPOA); later the Faculty) and the international economy took a turn for the worse with the oil crisis, the stock market crash and curbs on public sector expenditure. Promises of new services for an undervalued sector of the community were particularly vulnerable to political and economic fluctuations. Reduced public spending generated competition for resources rather than collaboration. For older mentally ill people, this was further complicated by ambiguities about who should take responsibility for their care – geriatricians, general psychiatrists or old age psychiatrists. Responsibility for the care of patients with long-standing severe mental illness who had grown old in hospital was a bone of contention between old age and general psychiatrists who were ‘dead keen to get us to take their old schizophrenics’, recollected Pitt many years later. Both general psychiatrists and geriatricians were happy when old age psychiatrists took mentally disturbed older patients off their hands. Categories of ‘dementia horizontalis’ and ‘dementia verticalis’ (i.e. more mobile, restless and often disturbing to other patients, requiring much POA nursing expertise) were one way of determining who should manage which patients, but the British Geriatrics Society and RCPsych jointly created more robust guidelines for collaborative working.18
Despite liaising closely with the DHSS, POA was not officially recognised as a NHS specialty. As a result, relevant age-based mental health data were not collected because ‘sub-specialty’ statistics were ‘ignored … coded under the appropriate main specialty’.19 This resulted in excluding POA from plans, such as for training psychiatrists and appointing staff. In 1978, for example, the DHSS recommended five consultants in ‘adult’ psychiatry and one in child psychiatry for a district of 200,000 people, with no mention of POA.20 Building projects for DGH psychiatric units also overlooked older people’s needs and innovative architectural designs to promote their independence.21 Sometimes, the DHSS admitted to only including older people when it feared that not doing so would leave them ‘wide open to severe criticism’.22 A different sort of data predicament arose when statistics derived from death certificates were used as a proxy for morbidity and health needs and underpinned NHS resource distribution; ‘dementia’ was generally subsumed under ‘old age’ making it invisible.
The government’s discussion paper A Happier Old Age (1978) acknowledged that services were ‘often less than satisfactory, making effective treatment or care difficult’ and that older people should be more involved in decision-making related to their health and social care.23 The Royal Commission on the NHS (1979) recommended additional resources for older people, but these were couched negatively in terms of ‘the immense burden these demands would impose’, a reiterated defeatist sentiment likely to discourage provision. In 1979, the new Conservative government was committed to controlling inflation, reviving the economy and holding back on public spending;24 and two years later, the DHSS’s Care in the Community was subtitled A Consultative Document on Moving Resources for Care, its real objective. The emphasis was on the role of the community, self-help and families to ‘look after their own’. This was unrealistic. The challenges for carers of people with dementia were well known,25 central to the origins of the Alzheimer’s (Disease) Society (founded 1979) and reflected in the title of the book The 36-Hour Day.26
Establishing POA services was entwined with policy, politics, public opinion and stereotypes (Figure 22.1), and its leaders had to fight for every penny. Economic analyses of NHS provision tended to blame the difficulties on more older people living longer, ignoring other factors, such as rising costs of staff salaries, drugs, health technology and the cost of high dependency and palliative care at any age. They ignored increasing longevity which allowed older people to be active for more years, often contributing to the economy despite not being formally employed. The government, however, attributed rising costs of health care to remediable inefficiency within the NHS,27 which required administrative reorganisation.28 Sir Roy Griffiths, managing director of Sainsbury’s supermarkets, led a NHS management inquiry and introduced solutions from the commercial sector, particularly ‘general management’ with professional managers responsible for planning, implementation and control of performance (see also Chapter 12).29 This was particularly abhorrent to POA which had evolved almost entirely through clinical leadership. The restructuring, like NHS reforms before and since, offered rhetoric about providing for older people rather than the means to do so.
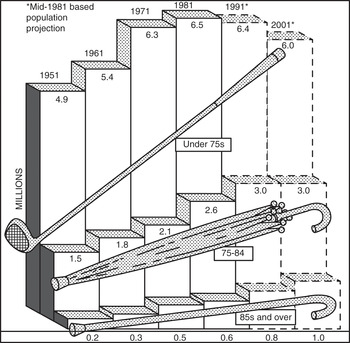
Figure 22.1 Official ageist stereotyping: ‘numbers of the elderly by broad age groups’, 1951–2001.
Amid the gloom, the ever enthusiastic and determined POA leadership found beacons of light. In neuroscience, the acetylcholine hypothesis of Alzheimer’s disease emerged and the Alzheimer’s Society helped push dementia higher in public awareness and onto national policy and research agendas. Clinical POA became more multidisciplinary, adding strength to services and to previously medically led arguments on the need for them.30 The British Psychological Society established their old age special interest group in 1980. Geriatricians established the first memory clinic in 1983 at University College Hospital, London.31 Old age psychiatry was putting down academic roots, with four professors by 1986: Arie in Nottingham and Levy, Pitt and Elaine Murphy in London. Murphy became editor of the first dedicated POA academic journal, the International Journal of Geriatric Psychiatry, from 1986. Some hospitals established joint geriatric-psychiatric units, based on the model Arie devised and used in his professorial unit. However, the Royal College of Physicians (RCP) recommended that geriatric medicine should integrate more closely with general medicine, partly because of recruitment difficulties, and this took precedence over a holistic approach to older people’s health care.32 In 1987, older people’s mental disorders were still not routinely included in nurse training, neither were they discussed in the Royal College of General Practitioners’ Preventive Care of the Elderly. Older people were also excluded from much medical research, hazardous in the context of them being likely beneficiaries of that research.33
Each step forward had to be fought for. With the DHSS reluctant to create old age services, and with responsibility delegated to professional managers, undervalued specialties were easy to neglect. Inadequate data, ambiguities over responsibility for health care in old age, the DHSS and the main body of psychiatrists prioritising younger people before older, as well as the tendency for the NHS to prioritise physical over mental illness, ensured, intentionally or otherwise, that psychogeriatric services lagged behind. Nevertheless, the specialty grew, from a handful of old age psychiatrists in 1970, to 120 in 1980 and 280 in 1989. Old age psychiatrist Professor John Wattis, by his spurious use of statistics, commented humorously: ‘You could draw a graph which showed that the number of old age psychiatrists was increasing exponentially and by the year 2000 there would be no doctors who were not old age psychiatrists!’34 Inspiring teachers and a charismatic leadership – such as Arie, Wattis, David Jolley and Nori Graham – demonstrated POA’s truly holistic approach to health and social care and the rewarding nature of the work and drew keen recruits into it. The SPOA wanted their specialty to be recognised by the DHSS to ensure dedicated data collection, training schemes and allocation of resources but the DHSS argued against it. One reason was their fear of recruitment difficulties for an ‘unpopular’ specialty but that was incompatible with evidence of more POA consultants leading more services.
There was little movement within the RCPsych to support official recognition of POA. However, the RCP was disgruntled about older, mentally unwell people on medical wards. Sir Raymond Hoffenberg, its president, established a working party about POA services. The outcome: a recommendation by the RCP and RCPsych for specialty recognition to facilitate service developments, education, training and research. The DHSS could hardly ignore the joint recommendation.
1989–2010
In 1990, the NHS and Community Care Act enshrined the NHS purchaser/provider split and the role of social services in assessing need while delegating care to the expanding private sector (see also Chapter 10). Instead of unifying old age services, it fragmented them, especially tricky for older patients who required coordinated multidisciplinary, cross-agency care. Despite ongoing challenges, old age psychiatry services multiplied across the country but many organisational goals and individuals’ needs were still unmet. Greater provision was required.35 By 1995, more than 400 POA consultants in the UK worked mainly in comprehensive catchment area and domiciliary-based services, a tried, tested and successful model of care.
The model of service provision began to change after the first acetylcholinesterase inhibitor for Alzheimer’s disease, donepezil, was licensed in 1997. It was expensive, around £1,000 per patient per year. Dementia was prevalent, the population ageing, the potential demand excessive and the NHS required it to be rationed. In 2001, the National Institute for Clinical Excellence (now the National Institute for Health and Care Excellence (NICE)) ensured this happened by recommending that donepezil be ‘initiated’ by a specialist. This was widely interpreted to mean making the diagnosis and prescribing the medication in secondary care. Memory clinics multiplied. From being mostly research-based in a few university centres, they became local diagnostic and treatment services countrywide. More technology and ‘real medicine’ may have helped to reduce stigma and encourage public discussion. However, memory clinics also had drawbacks. These included transferring people with uncomplicated dementia into secondary care rather than developing skills in primary care as for other common disorders such as depression, diabetes and hypertension. They also diminished time available for expert staff to provide the mainstay of psychosocial interventions required by patients with the most complex and distressing dementias. More resources from a finite pot going into dementia services also detracted from providing services for older people with functional mental illnesses. This was worrying when dementia affected 5 per cent of people over sixty-five at any one time, while depression alone among the functional disorders affected more than 20 per cent.36
The pattern of officialdom allowing older people’s mental health service provision to lag behind that for younger adults persisted. The National Service Framework for Mental Health (1999) was for ‘working-age’ adults. Substantial extra funding accompanied it. The National Service Framework for Older People arrived eighteen months later. It was comprehensive, including functional disorders and dementia, but without the money attached to facilitate implementation. Observing improvements made in services for younger patients caused much frustration among old age psychiatrists.
The POA leadership had to advocate persistently for older people to receive appropriate levels and ranges of care equitable with those provided for younger adults. In 2005, the RCPsych Faculty of Old Age Psychiatry pointed out that ‘liaison psychiatry’ (psychiatric services for physically unwell patients in general hospitals) for working-age adults had ninety-three dedicated consultant posts in the British Isles but, for older people, consultant liaison input was additional to their general catchment area responsibilities.37 In 2006, a joint RCPsych and RCP report stated: ‘Ageist neglect of older people with mental illness must stop.’38 It did not stop and more inequity of provision followed, such as the Improving Access to Psychological Therapies (IAPT) programme (2008). IAPT was based on the premise that improved treatment of anxiety and depression for working-age adults would reduce their unemployment rates and thus pay for itself, or even generate notional surplus. IAPT excluded people over the age of sixty-five, even though they could benefit from the treatments offered. There was no acknowledgement that alleviating their mental symptoms could enable them to contribute more to society, such as in voluntary roles, and enhance independence, thus reducing the need for statutory support services, all of which could benefit the economy.
Other changes affected care for mentally unwell older people. The Mental Capacity Act (MCA) 2005 came into force in 2007. It provided a statutory framework to empower and protect vulnerable people who were unable to make their own decisions. Although idealistic and important for older people, implementing it, particularly the Deprivation of Liberty Safeguards, brought new layers of bureaucracy at great financial expense, removing resources from direct care.
The financial crisis of 2008 preceded another much-needed and well-intentioned initiative, the National Dementia Strategy,39 and probably hampered its outcome. The Strategy aimed to help people ‘live well with dementia’, by encouraging early diagnosis; improving education and research; and attending to the needs of people with dementia and their carers in the community, care homes and general hospitals. It had money attached: £150 million over two years to support implementation. This was very welcome. However, in the context of direct costs of health and social care for dementia of around £8.2 billion annually, it was a drop in the ocean. Early problems with the Strategy included a baffling range of organisations – statutory, private, not-for-profit, health and social care – and a flurry of vaguely titled new job roles such as ‘advisors’, ‘navigators’ and ‘co-ordinators’, hardly straightforward for people with dementia and their carers to negotiate. The POA activists Professors Susan Benbow and Paul Kingston observed this and commented:
sexy new solutions implemented by managers can have the opposite effect to that intended. We need to stop our headlong rush into implementation and look at the evidence for these new roles, to consider what added value they bring, and how they can be governanced and supported. Only then will we do justice to the people and families living with a dementia.40
In the wake of the Strategy, NHS England appointed Professor Alistair Burns as National Clinical Director for Dementia. Potentially beneficial, this added to the worries of many in the field of POA: should dementia be syphoned off as a separate entity, and what about the rest of old age psychiatry? Depression and psychosis in old age, key concerns for POA, were barely talked about outside specialist circles. The Strategy’s protagonists had hoped that the issue of dementia would spearhead developments to benefit older people’s mental health, well-being and dignity more broadly. The sentiments were admirable but the outcomes complex, multifaceted and mainly after 2010, so outside the scope of this chapter.
The Equality Act 2010 proved to be a hindrance as well as a help for POA: it could not abolish deep-rooted societal ageist attitudes. These contributed to (mis)interpreting the Act in ways which affected service provision, such as by depriving older people with non-dementia mental illnesses of specialist facilities and treatment and placing them instead in ‘all-age’ or ‘ageless’ services. This failed to take into account their needs which differed from those of younger people, including frailty; multiple comorbidities; risks from drug side effects and polypharmacy; different presentations of the same disorders; and different psychosocial, cultural and financial contexts.
Conclusion
Major drivers of change included dictates of fashion, supposed economy and non-validated theoretical perspectives, often imposed from a top-down template. Policies and implementation patterns derived from managerial rather than POA clinical leadership demonstrated ageist perspectives. National directives advocating uniformity of service provision could be good, ensuring access to an agreed range of services at acceptable standards and avoiding a postcode lottery. However, uniformity ignored the need for variation to fulfil local needs and undermined innovative service delivery responses. It also destroyed morale, particularly when it led to the dismantling of trusted service components which fostered expertise and humane practice, such as joint geriatric-psychiatric units, services for ethnic minority populations and long-stay NHS units for people with the most difficult to manage mental disorders. Some dismantled services required painful reconstruction when policy changed.
By 2010, there was unease about the future of the specialty. Baroness Elaine Murphy commented that some social care services, essential in POA, were in ‘meltdown’,41 and Professor Robin Jacoby wrote an article on POA called ‘Of pioneers and progress, but prognosis guarded’.42 Ageism, despite the Equality Act, plus fiercer NHS business models of health care and seeking to maintain a corporate image, contributed to the difficulties. Despite the challenges, the rewards of making the lives of older people and their families more hopeful, dignified and fulfilling, by combining individual care and aiming to improve service delivery and linked to new frontiers of neuroscience research, exemplified the interactions between Mind, State and Society and continued to attract dedicated clinicians.
In 2018, a RCPsych report was entitled, Suffering in Silence: Age Inequality in Older People’s Mental Health Care.43 In 2020, NHS England’s website stated ambiguously that older people’s mental health ‘is embedded as a “silver thread” across all of the “adult” mental health Long Term Plan ambitions.’44 Both Suffering in Silence and the ‘silver thread’ blow an icy wind of ongoing ageism and under-resourcing, failing to allow older people to have the most humane treatment and failing to learn from history.
Key Summary Points
Liberal ideas about personal autonomy, choice and independence emerged internationally in the 1960s. Changing agendas permitted younger people to make choices, even if risky, but older people were perceived as inevitably vulnerable and, despite their experience of life, their wishes were frequently ignored.
For older people, clinically and scientifically, things edged on, albeit slowly.
Promises of new services for an undervalued sector of the community were particularly vulnerable to political and economic fluctuations.
The POA leadership had to advocate persistently for older people to receive appropriate levels and ranges of care equitable with those provided for younger adults.
Ongoing and ageist themes over the fifty years have included prioritising services for younger patients; the double whammy of stigma of mental illness plus old age; and policy decisions based on short-term economic calculations rather than likely health and well-being outcomes.
The transition from asylum life to the everyday world is a stage of peculiar difficulty with the recovered patient. The home and family life to which he returns may be unsuitable or unsympathetic; employment may be hard to obtain, and friends may be unable or unwilling to help.
Introduction
The social and organisational development of community psychiatry in the UK has been covered in other chapters in this book (see also Chapters 10, 30 and 31). The best overall description of the meaning of ‘community psychiatry’, however, was provided by Douglas Bennett and Hugh Freeman in their magisterial 1991 textbook in which they outlined its principles, its origins and its progress.2 Key features of the latter were, of course, the 1959 Mental Health Act; the process of ‘normalisation’ in the asylums; the discovery of chlorpromazine and other effective psychotropic medications; and the social underpinnings of whatever was meant by the term ‘community’. The rising critique from the anti-psychiatry movement, and the notion that psychiatric illnesses were understandable reactions to social stress (rather than formal illnesses that could be medicalised), became a dominant theme (see also Chapter 20). Yet different localities proceeded at a different pace in terms of developing actual community care resources, there being no formalised process. Stumbling out of the fog of change came the Community Mental Health Teams (CMHTs) and, more specifically, in 1991, the Care Programme Approach (CPA),3 developed by the government’s managerialist Department of Health. Likewise, evaluating the effectiveness of community care teams has been extremely difficult and often very localised. Numerous thoughtful papers on the process of community care have been published (e.g. ‘Deinstitutionalisation: From hospital closure to service development’ by Graham Thornicroft and Paul Bebbington)4 and there have been endless policy papers published (e.g. Better Services for the Mentally Ill in 1975)5 as well as the National Service Framework for Adult Mental Health (NSF) in 1999,6 these rarely involving or consulting frontline practitioners (see also Chapter 12).
As a result, the term ‘community care’ has come to be mocked in, for example, TV comedies and public attitudes and has been associated with public homelessness (see Chapter 26) and inquiries into homicides (see Chapters 27, 28 and 29) as well as being considered as indicating the neglect of psychiatric services. In a 2001 paper, Julian Leff asked, ‘Why is care in the community perceived as a failure?’7 Having developed the model TAPS project for the closing down of Friern Barnet Hospital in North London,8 he admitted that ‘a comprehensive community psychiatric service, catering to all the needs of the catchment area population, exists nowhere in the British Isles and will never be achieved’. He noted at the time that few people were aware that ‘of the 130 psychiatric hospitals functioning in England and Wales in 1975, only 14 remain open, with fewer than 200 patients in each’.
From the point of view of a practising consultant psychiatrist working in the system, this chapter will therefore be an impressionistic understanding of how community care has developed and not developed and the extent to which it can be seen as a success or failure. The former is reflected in patients’ greater personal freedoms in choosing their daily lifestyles and the latter in the doubling of the prison population over the last forty years as well as the concomitant institution of numerous medium-secure forensic health units. This process has been labelled ‘reinstitutionalisation’.9 There has also been a rise in the use of the Mental Health Act and the pernicious development of ‘risk assessment’ as the driving factor in working with patients (see Chapter 27). This is despite the fact that there is no evidence that risk assessment protocols show any effectiveness in terms of predicting who will or will not go on to become a ‘mentally disordered offender’ (see also Chapter 29). One could even consider that the primary role of the asylums, to deal with the neglect and corruption of the private madhouses, has now been reversed, in that private provision for the seriously mentally ill has become dominant.
Moving into the Community
There is no clear definition of ‘community psychiatry’ apart from the belief that it is not hospital-based. The original term for it was ‘extramural’, and the initial programme involved the gradual sizing down of the asylums (often many thousand strong) into smaller units with the development of general hospital psychiatric units. Thus, in 1974, if you developed a serious mental illness in Hackney in East London you were put in an ambulance and taken to one of the larger Surrey hospitals/‘bins’ outside to the southwest of the capital or possibly to Friern Barnet in North London. By 1975, the link between Hackney and the large asylums had been broken, with the setting up of specific, local psychiatric wards in Hackney Hospital. This hospital was an old workhouse infirmary and looked as grim as anything could, but it was local.
A feature of this development was also the need to establish clear catchment area limitations for any psychiatric hospital unit, a local responsibility arrangement harking back to the old parish responsibilities of the nineteenth century. This was because the theorisation of community psychiatry seems to have forgotten that a key feature of psychiatric treatment, particularly in the inner city, was the use of the Mental Health Act for patients lacking insight into their condition and their needs – the application of the Act requiring the engagement of local social services. Thus, variably unwilling asylum physicians had to move into general hospitals (often to the dismay of fellow consultants) and try to look after CMHTs, which in themselves were undefined and variably developed. The practicalities of doing this were never carefully outlined and, although the asylum bed numbers declined gradually, the detention rates soared and the shortage of psychiatric beds (illustrated by often being 120 per cent occupied!) became a dominant concern, particularly from the 1980s onwards.
In Manchester, for example, in the late 1990s, it was reported that there were more than twenty patients detained under the Mental Health Act but awaiting admission.10 NHS resources often could not fund proper bed availability, this depending on the extent to which psychiatric professionals (especially consultants) were able to bully managers into making appropriate provision; and although CMHTs were primarily focused on looking after those with psychotic conditions (‘the new long-stay’), there grew a rising demand for the treatment of common mental health problems, which some dismissed as the concerns of ‘the worried well’. These patients were asking for help with depression and anxiety in the context of heavily advertised new antidepressant medications such as Prozac and the better recognition of the meaning of depression.
In essence, therefore, the process to deinstitutionalise and move towards community care was stumbled upon by accident, rather like the British Empire. A number of charismatic psychiatrists had led the way, for example Maxwell Jones at Belmont (his book Social Psychiatry was published in 1952; see also Chapter 20).11 Yet the practical problems of setting up a CMHT depended substantially on the goodwill between NHS and local social services. Trying to get community psychiatric nurses (CPNs), consultant psychiatrists, psychologists, occupational therapists, social workers, senior and junior, and the ‘lowly’ support workers to live and work together required immense time and effort and there were often fractures in the teams, who differed in terms of background culture, training and pay grades. Latterly, the primacy of primary care in terms of funding local resources has generated a particular demand from GPs to have CPNs and psychologists working for their primary care resource, thus further depriving specialist mental health services of staff who might otherwise have been available.
Another key feature of community care has been the regularity of shocking newspaper exposés – for example, the 1980s articles by Marjorie Wallace in The Times and the relentless publication of homicide inquiries (e.g. the report on Christopher Clunis produced by Ritchie in 1987).12 In this regard, whenever a lurid headline or TV news report announced yet another murder by a psychotic patient in the community, every thinking psychiatrist’s first reaction was to find out where the event had taken place (hoping it wasn’t in their catchment area). Fear of being called to appear before an Untoward Incident Inquiry, therefore, became part and parcel of being a consultant psychiatrist, certainly in the inner city, and the ultimate insult was when the process of inquiries was in itself privatised.
Homicide Inquiries
Homicide inquiries became the hallmark of psychiatric care in the 1980s and 1990s, gradually fading out only as pressure on the newspapers not to publish them too often started to work. This was achieved in terms of anti-stigma campaigns. The most offensive of these inquiries was the Luke Warm Luke case,13 running to some £75,000 in costs (thanks to the chair, Baroness Scotland) and several volumes of standardised prose, largely rewriting the CPA and adding nothing new to our understanding of the management of serious mental illness. The incident was due to the girlfriend of a psychotic patient refusing CMHT advice that she not visit him at home and her ending up murdered by the patient. As noted, however, the most influential report was the inquiry into the care of Christopher Clunis,14 which outlined all the problems of providing care in the community in a fractured framework of varying local mental health provision (see also Chapters 28 and 30).
Christopher Clunis was first detained in hospital in Jamaica (see Tables 23.1 and 23.2) and diagnosed with paranoid schizophrenia. Subsequently, however, he was detained in a number of different hospitals, mainly in London, with diagnoses changing constantly. Like many difficult patients, he ended up with being ‘diagnosed’ as having a ‘personality disorder’. Records showed his constantly assaultive behaviours were noted but tended to improve with appropriate medication. Like many insightless patients with paranoid schizophrenia, however, he would not continue medication on discharge from hospital, and one night in North Finsbury station (in North London) he stabbed Jonathan Zito in the eye, killing him. This assault very much reflected Clunis’s own psychotic experience of feeling that people were somehow interfering with him by looking at him, and he had assaulted a number of other people in the eyes beforehand.
Table 23.1 The Clunis inquiry: diagnoses, 1986–92
| 1986 | paranoid schizophrenia |
| 29.6.87 | schizophrenia with negative symptoms |
| 2.7.87 | schizophrenia or drug-induced psychosis |
| 24.7.87 | depression |
| 1.1.88 | drug-induced psychosis, or manipulation for a bed |
| 29.3.88 | psychotic or schizoaffective illness |
| 3.5.88 | schizophrenia, drug-induced psychosis or organic illness |
| 7.6.89 | paranoid schizophrenia |
| 23.7.91 | schizophrenia |
| 5.5.92 | paranoid psychosis |
| 14.8.92 | paranoid schizophrenia |
| 26.8.92 | (diabetes) |
| 10.9.92 | normal mental state, abnormal personality |
Table 23.2 The Clunis inquiry: lengths of stays, 1986–92
| 1986 | Bellevue Hospital, Jamaica | Not known |
| 1987 | Chase Farm Hospital | 25 days, 4 days |
| 1988 | Chase Farm Hospital | 3 days, 4 days |
| King’s College Hospital | 7 days | |
| Dulwich North Hospital | 9 days | |
| Brixton prison | 21 days | |
| Dulwich North Hospital | 169 days | |
| 1989 | St Charles Hospital | 110 days |
| 1991 | St Thomas’s Hospital | 21 days |
| 1992 | Belmarsh Prison | 24 days |
| Kneesworth House Hospital | 80 days | |
| Guy’s hospital | 34 days |
The Clunis case can be seen as a template for the problems in community care. None of the members of the teams standing in the rain outside his front door trying to assess him in North London on more than one occasion had ever seen him before, thus he was able to walk out of the house without being recognised. The disjunctions of care between South and North London were noted, as was the tendency of mental health staff to downplay assaultive behaviours and their significance. The subsequent criticisms directed at the team ultimately landed with assessing him were unfair (they had minimal information and none of them had ever assessed him before), but the outline of the problems of community care was well adjudged. An important corollary was the development of a voluntary organisation called the Zito Trust (led by Jayne Zito, wife of the murdered man) which developed a full review of homicide inquiries, some 120 reports having been published by 2002, summarising and outlining them to a helpful degree.15 Like many other such voluntary organisations, for example Marjorie Wallace’s development of SANE, the general view of the concerned public was that asylums should not have been closed so quickly and that there should be more hospital beds. As noted, bed shortages have been, perversely, the dominant theme in the community care debate.
The impact of homicide inquiries on the morale of CMHTs was substantial. Staff felt stigmatised by their work and reports regularly considered failures in communication and the inappropriate use of CPA documentation as problematic. The use of complex forms to be filled in at every assessment became a negative, however, with some CPA documents taking up nine to ten pages and requiring regular reiteration when each clinical review was carried out. This was despite there being no evidence at all that filling in such a form correctly predicted the outcome for individual patients. Homicide inquiries were infused with the problems of hindsight and the counterfactual thinking generated thereby.
Along with the development of CPA and risk assessment, there was an attempt by the government in 1999 (Patients in the Community Act)16 to introduce supervision registers. These required doctors to fill in a form to determine the risk of every patient in their care, a bit like filling in the ‘proscription’ levels as noted in ancient Rome or being asked to identify potential Jews in your locality in Germany in the 1930s. Such central government impositions on practice were driven by a managerialism that has become intrinsic to NHS organisations, with little input from frontline clinicians, whether nurses, doctors, psychologists or social workers. The notion of community care as ‘outdoor relief’ or the transferring of care away to untrained staff on part-time contracts became increasingly part of our understanding of ‘care in the community’, CMHTs generally having to work out their own ways of managing patients. Heroically, supervision registers were mainly ignored.
Later Developments
In 1999, the Blair Labour government introduced the National Service Framework (NSF),17 this demanding that Trusts set up specific teams for the assessment of crisis intervention (for acute and severe mental health problems), early intervention (for patients with first-episode psychosis) and assertive outreach (for those patients whose mental ill health was thought to cause serious concern but who were not engaging with mental health services follow-up). From the organisational point of view, the need to develop a series of teams that could be specific and could not be diluted by other NHS demands (as many mental health initiatives have been) enabled the NSF and funding for it to be forced through the NHS system (see also Chapters 10 and 11). This was a clever piece of government initiative but it imposed significant limitations in terms of how mental health teams operated. In particular, the dividing up of the CMHTs into these sub-teams generated arguments as to who looked after whom and created unrealistic expectations in those given, for example, early intervention services. After being moved on from their early intervention service (with its high inputs and regular support), they were in fact referred on to the badly resourced CMHTs.
While the government’s introduction of these specialist teams was welcomed in terms of funding and resources, the role of the standard CMHT remained deracinated and uncertain. Furthermore, the crisis intervention teams took on the burden not only of seeing people in crisis (however defined) but also of being the ‘gatekeepers’ to admission to hospital. This led to arguments with consultant psychiatrists, who had known patients for many years, who were advised they had to resort to a nurse and social worker (relatively untrained compared to them) in a crisis care team to allow admission. The earlier difficulties of putting together multidisciplinary CMHTs were recreated and psychiatrists were deskilled, as their clinical activities became limited to certain interventions such as crisis management or early intervention. The ability to look after a patient right across their lifestyle and their lifetime, whether as an inpatient or outpatient, reviewed in the community, became limited. This fragmentation of services went against the standard findings of all homicide inquiry reports, namely that there should be connected services right across the spectrum.
Debates about the value of specialist teams went on in community care forums, with considerable division as to whether they were effective or not. A number of psychiatrists enjoyed the limitations of, for example, just doing assertive outreach, despite losing their skills in terms of managing patients with depression, anxiety and other non-schizophrenic disorders. Many assertive outreach teams became essentially rehabilitation teams, and a number have been gradually phased out in this context.
Overall, therefore, while the NSF engendered increased funding for psychiatry, the break-up of CMHTs generated limitations in the kind of work that could be provided. For example, new trainees found themselves either just in a crisis team or in an assertive outreach team or in an early intervention team and not seeing the overall picture in terms of management of patients with a range of conditions, in the community and in hospital wards. Thus, they missed out on being part of what has been called the ‘general psychiatry’ attitude. This imposition of excessive specialisation has been amplified by the hiving off of forensic psychiatric care into locked units (indoor psychiatry) and the push for many practitioners now to just conduct ‘primary care psychiatry’.
Primary Care Psychiatry
Regarding primary care psychiatry, this again has developed in a patchwork way, depending on the willingness of GPs to have psychiatrists in their surgeries. As a keen young psychiatrist in the 1980s, my offer to see patients at GP surgeries was met with varying degrees of perplexity and receptivity. A number of thoughtful practices were very welcoming but other smaller practices found it difficult to accept having another doctor sitting in their offices (and often there was no room to do so). While GPs have been known to be at the front line of psychiatric services for many years,18 their main engagement has been with patients with non-psychotic conditions and meeting the requirements of advice as to therapy as well as the best antidepressants and anxiolytics to prescribe. There could also have been a fruitful exchange of information between GPs and psychiatrists, in terms of the complex social and physical conditions that patients present with and the appropriate use of medications or other treatments. However, it is not untypical to review a patient’s GP notes (a rich source of information) and find that they have been prescribed three or four different antidepressant selective serotonin reuptake inhibitors (SSRIs) over the years, with limited benefit and with no review of the patient’s compliance or underlying mental state. Many patients asked about old prescriptions will often say they did not take the pills for very long, if at all.
Fortunately, the improvements generated by the IAPT (Improving Access to Psychological Therapies) programme have helped very much with the provision of cognitive behavioural therapy (CBT) for common mental conditions (see also Chapters 10 and 33). Resources, however, have varied from area to area. This has been one of the genuine positives of community care. The fact that many GPs, having undergone a psychiatric attachment in their rotation, are now trained in identifying and managing mental health problems has also enhanced the ability to develop appropriate psychiatric services in conjunction with GPs. This is in contrast with the failure of the Royal College of Physicians and the Royal College of Surgeons to embrace psychiatric education as any part of their training programmes.
Conclusion
The development of community care in the UK has been haphazard, deriving from theory rather than practical consideration. The human resource problems of putting together CMHTs in different areas have been little understood by central government, and the development of such teams has largely been based on the goodwill of local professionals to ensure communication and provide office space and support. The regular negative views of community psychiatry in the public perception have further limited the development of services. The impositions of paperwork and additional documentation based on risk management have led to many CMHT members spending half their day at their desks doing paperwork. This over-engagement in paperwork is well known throughout the NHS, and one only has to review a typical patient’s GP notes to realise that most of what is written there is reduplicated and not clinically necessary. For example, blood test findings are mentioned under various different categories. The notion that ‘every form filled out means a kindness foregone’ can be seen as a key difficulty of community-based care.
As ever, psychiatry has been substantially undermined by the persistence of stigma (see also Chapter 27) and the intrusions of a powerful, socially generated belief that mental distress can be distinguished from mental illness. The battle to get mental illness back on the agenda has been prolonged, but a number of Trusts continue to downplay the need for a formal diagnosis and it is now possible to have an assessment for your mental health needs carried out by an individual who has no training as a psychiatrist but who may well be called a ‘high intensity practitioner’. While the diminution of the consultant psychiatrist’s role from their predominance in the old asylums has its benefits, in terms of introducing other expertise into the management of those with mental health problems, the need for expertise in psychiatric diagnosis, the management of psychopharmacology and leadership of a team with many diverse backgrounds is central to what a psychiatrist has to do whether in hospital or in the community care sphere.
The rise of risk management has been a dreadful negative, in terms of looking at the role of a consultant psychiatrist and in terms of the importance of carrying out an appropriate mental state assessment and diagnostic review. The prevalence of criminalised drug usage (e.g. cannabis and cocaine in particular) has further complicated matters. Given the vulnerability of mentally ill patients using drugs to improve their mood or lower their anxiety, this drugs ‘prohibition’ policy has major negative effects in terms of criminalising the mentally ill (see also Chapters 28 and 29). The extension of low-secure and medium-secure mental health units (often privatised) reflects the reinstitutionalisation of mental health care generated by a risk avoidance strategy and a more punitive attitude towards those with mental illness. The extraordinary rise in the number of prisoners in the UK (as noted in the Introduction to this chapter) is a key reflection of Penfold’s theory that there is an inverse relationship between prison and asylum care.19 Visiting HMP Pentonville in the late 1990s, I was advised by one of the senior prison officers that ‘this is the largest medium secure unit in the country’. This imprisonment of the mentally ill is against the background that the number of homicides committed by mentally disordered offenders has not increased since the 1950s,20 by contrast to the numbers of homicides committed by ‘normal’ citizens, which has increased markedly.
Key Summary Points
The process of de-asylumisation into a community care–based mental health system has been a messy business, a social crusade rather than a clinically thought-out process.
Concomitants like modern psychopharmacology and the effects of the Royal College of Psychiatrists’ anti-stigma campaigns have helped but care has varied substantially in quality across the country.
Community care has relied on the qualities of individual psychiatrists and CMHT members, as well as local GP and/or social services support, and generally has not been helped by the numerous government White Papers.
The reversion to medium-secure mental health units and reinstitutionalisation has been a core feature, publicly unrecognised.
Mental health services have coped to varying degrees despite their core asylum resource being stolen from them, and the key need now is for the elimination of the primacy of risk assessment and the maintenance of the generality of general adult psychiatry.
Introduction
The fifty years since 1960 cover one of the major periods of change in services for people with intellectual disability as the service model based on colonies, with isolation and ‘protection’, was dismantled and a new model of care in the community enforced. This required a massive change in public attitudes, policy, funding, professional roles and training and in medical and social infrastructure. These various facets have not operated in synchrony, so it has been a prolonged journey through some turbulent waters which has not yet reached the tranquil lake. This chapter briefly discusses some of these issues but concentrates on the policies of England and Wales. The terminology has changed over time from mental deficiency to mental handicap, learning difficulties, learning disabilities and the current intellectual disabilities or disorders of intellectual development. The terminology at the time discussed is used in this chapter, even though the terms used then are seen today as objectionable. The reason for using the terms used at the time is that they referred to varying concepts and subgroups.
Where Did We Start From?
From 1913 to 1959, the model of care was dominated by the 1913 Mental Deficiency Act, derived from the 1908 Royal Commission on the Care and Control of the Feeble Minded.1 It concentrated on the need to identify ‘mentally defective’ persons who were not adequately supervised in the community and maintain them in ‘colonies’ operated by local authorities. The purposes of the colonies were later stated in their nurses’ manual to be:
1. A training school for mentally defective children or adults for whom suitable training outside is not available.
2. A shelter for those who are homeless, neglected or otherwise in need of a home and protection.
3. A hospital for those who are of low grade or physically helpless or epileptic and who require nursing care which cannot be provided in their own homes.
4. A place of control for those who are mischievous, destructive or harmful or who are a danger to themselves or to others if left in the community.2
With the formation of the NHS, the colonies were removed from the local authorities and transferred to the NHS in 1948 as hospitals. This immediately reinforced the assumption that ‘mental deficiency’ was a mental health condition and not a social concept. In addition, having the entire health budget for the country in one pot made governments reluctant to face the increasing cost of need while also facilitating the diversion of longer-term care monies to bail out the more prominent and bankrupt acute hospitals.
The 1957 Royal Commission on Mental Health Law recommended community care and a change in the law. The resulting 1959 Mental Health Act changed the legal concept of social defectiveness contained in ‘mental defective’ to that of ‘mental subnormality’, excluding many who were previously included. It also changed the assumption of compulsory admission to that of voluntary admission. The change of law changed the clinical concept. At the start of the 1960s, many of the more able patients became voluntary patients who immediately left hospital and lost contact with their services as they created their own lives in the community.
In 1960, most people with ‘mental subnormality’ lived in the community but almost all state-provided care for them came via special schools or ‘subnormality’ long-stay hospitals. These ‘hospitals’ commonly held 200–400 residents each, but there were 5 reaching more than 2,000. In these, men, women and children were still segregated as in the old Victorian workhouses. Most wards housed 50–60 patients with 2 staff to care for them. Staff would be sacked for mistreatment but keeping order relied on institutional intimidation. Everything had to happen in groups – patients queued for baths or shaving (razor blades changed only after a set number of people had been shaved); there was no personal clothing; and work was mundane. Abuse was widespread. Families were not allowed to visit the wards but were assured their loved ones were well cared for.
1960–1980: The Need to Act and First Steps
By 1960, the pressure to change was international and reforms started that still dominate the system. John F. Kennedy’s family experiences enabled key legislation in the United States such as the 1963 Maternal and Child Health and Mental Retardation Planning Amendments.
The principles of ‘normalisation’ were being developed in Scandinavia with Bengt Nirje of the Swedish Association for Retarded Children at the forefront. In 1971, the United Nations’ Declaration on the Rights of Mentally Retarded Persons stated such people should have the same rights as others as far as feasibly possible, should have economic security and should live in the community with their families.
In the UK, the 1960s saw campaigns for better services for people in the community taking hold. Local authorities started to create large institutional day centres (often called training centres) as well as respite hostels. Activities were structured like a continuation of school, but many centres emulated the new industrial therapy ideas of mental health with the more able attendees spending much of their week on simple assembly lines. The hospitals had lost a lot of the people who operated their farms, cleaned their wards and cared for the less able but were refilled from the long waiting lists of families desperate for care. The inpatient population became more demanding at a time when there were still usually only two staff per sixty residents. They were also universally overcrowded, often holding 20 per cent more patients than designed for. Scandals started to proliferate.
On 20 August 1967, the News of the World published allegations of abuse at Ely Hospital in Wales. Farleigh Hospital near Bristol was visited by the police in December 1968. Each triggered a formal inquiry that fed the newspapers sensational news of abuse. These scandals continued through the 1970s with inquiries at Coldharbour by Sherbourne in 1973; South Ockenden in Essex in 1974; Brockhall in Lancashire in 1975; St Ebba’s in Epson in 1976; Mary Dendy in Lancashire in 1977; and the Normansfield in 1978. In addition, the media published various investigations inspired by the scandals. On 29 May 1972, the prime-time television programme 24 Hours showed a devastating 20-minute programme on the state of Stoke Park Hospital, showing staff struggling against all odds. The senior staff described parts of the hospital as a slum, comments that echoed around the country. The message was clear and reinforced over ten years: relatives were no longer to trust the old institutions or the reassurances that their loved ones were well cared for. Things had to change.
In England, four new policies emerged:
The Local Authority Social Services Act of 1970 brought together many of the social care services under the responsibility of local authorities to enable more coordinated care.
The Education Act of 1971, which in accordance with the UN declaration explicitly included all children as the responsibility of the local authorities’ education boards and no longer excluded ‘subnormal’ children who were in hospital training centres.
The 1974 reorganisation of the NHS into district health authorities ended the local management separation of the mental handicap hospitals from the acute general hospitals. Local budgets were dominated by the needs of the acute hospitals, but this enabled closer co-ordination with general hospitals and with the coterminous local authorities.
These structural changes underpinned implementation of the 1971 White Paper Better Services for the Mentally Handicapped which set out the new direction for all services. It included the principles of non-segregation, access to ‘stimulation, social training and education and purposeful occupation’ and wanted residences to be as homely as possible.
The White Paper recommended a large increase in the residential care provided in the community and training centres, alongside halving the hospital beds. It promulgated new 24-bed hospitals scattered around the community with new local authority homes of a similar size. No new hospital should exceed 100 beds and no old large site should be added to (except with temporary buildings to relieve current overcrowding).
At the time, this was a radical plan to move to a lifestyle closer to the ideology of normalisation, but it was still based on using rather large low-staffed units only half the size of the usual long-stay hospital villas. In addition, the White Paper looked only at ‘mental handicap’ services and did not consider whether the generic services were able to provide a non-discriminatory service.
In 1975, the government created the National Development Team for the Mentally Handicapped to advise their social service planners. Several pamphlets were published, including one describing the creation of Community Mental Handicap Teams and several local services were visited when requested to advise on local service developments. It was recognised that any move from long-stay hospital to local authority residential care would involve the development of care expertise in local authority settings. There were attempts to move nursing staff, along with the smaller health service hostels/hospitals, to local authorities, but this was resisted by the unions, despite the 1979 Jay Report declaring an end to mental handicap nursing.3
The changes of the 1970s reflect the impact of scandals in hospital care which produced pressure for local authorities to develop services in the community and to close hospital wards or at least improve them with temporary buildings. However, they occurred in a decade of financial crisis, so resources were limited. Despite this, by 1980 new financial structures for community care were developing alongside day services and some Community Mental Handicap Teams (using hospital staff). In addition, there were some hospital improvements and some reductions in hospital numbers, particularly removing children from long-stay hospitals.
1980–2000: In Search of a New Model As the Old Hospitals Close
In 1980, the Department of Health and Social Security (DHSS) published a review of progress since the 1971 White Paper.4 It concluded that it had overestimated the need for hospital places and estimated that 3 out of 1,000 of the general population needed special mental handicap services. It noted the problems of finance and the need to explore alternative models of transitioning. The next decade saw investment for new academic departments researching models of care. As a result, the policymakers had more evidence about specific models attracting public campaigns.
The pressure from campaigning groups trying to shape policy increased. The Campaign for the Mental Handicapped (CMH) had responded to the 1971 White Paper by publishing Even Better Services for the Mentally Handicapped. In 1981, it published The Principle of Normalisation: A Foundation for Effective Services by John O’Brien and Alan Tyne. O’Brien published his five principles in 1991 and they dominated service design in Britain for the next decade, being cited in almost all local policy and planning documents. The King’s Fund also published a series of influential booklets and project papers, including An Ordinary Life in 1980 and People First in 1984. In 1984, the self- advocacy group People First was founded as the voice of people with ‘learning difficulties’ – and it was increasingly referred to by government when developing policy. Their campaign, summed up in the 1990s by Nothing About Us Without Us, became accepted by most policy organisations. In response to their campaign, the government abandoned the term mental handicap for the new term learning disability (LD). The general message from these campaigns was clear: the old colony ‘mental defectives’ were now people with learning disabilities (PWLDs) who were to be treated as equal members of the community and therefore would want to live in ordinary houses and integrated within the community, with useful employment. However, there were alternative voices: The National Society for Mentally Handicapped People in Residential Care (Rescare) was established in 1984 as the national voice of many League of Friends for the old hospitals. They expressed fears about their loved ones moving into the harsh community and advocated turning the hospital sites into residential campuses.
Alongside this, there was a new Education Act of 1981, inspired by the 1978 Warnock Report, with needs assessment to secure the resources to enable a child with learning difficulties to be educated in mainstream schools with additional support or in special schools. This was an advance in integration, which was set back later when school attainment tests reduced the popularity of low-performing pupils. Higher education colleges were also financially encouraged to admit students with severe learning difficulties, though cuts in the next millennium reduced this incentive as well.
The 1980s saw the active planning for closure of most of the large old long-stay hospitals. After ten years of planning, the first large hospital to close was Darenth Park in 1988.5 Financial pressures and bureaucratic problems delayed other closures or forced some closures to include decanting patients to more local hospitals or large homes.6 Nevertheless, by 2000 most of the large hospitals had closed or were near to closure.
In the 1980s, central government awarded a standard sum to people moving into community care homes to fund their care and community services. This was independent of need and encouraged many new small care settings, owned by ex-hospital staff, to take the more able out of hospitals. The escalating costs of the funding system changed with the 1990 NHS and Community Care Act, making it the responsibility of local authorities to assess the care and support needs of people and to fund according to need after means testing. The Act also brought in the purchaser/provider split (see also Chapter 10), ending the provision of care by local authorities and enabling a plethora of care providers to develop.
In 1992, the media reported one of the first major care scandals in a community care home. It was revealed that residents of the Long Care group in Buckinghamshire had been systematically physically, emotionally and sexually abused by some staff.7 The main outcome was to remove inspection from local authorities to a new national social care inspectorate – which, after many reorganisations, has become part of the current Care Quality Commission.
2000–2010: Gaining Rights and Tackling Mainstream Services
In this decade, the persistent attitudes of the public and mainstream services came under the spotlight and the rights of PWLDs were consolidated. The White Paper Valuing People was published in 2001 (Scotland had published The Same As You a year earlier). Both emphasised the need for equality and inclusion in the mainstream community, including in all health services, education, work and accommodation. Person-centred care planning was mandated and advocacy promulgated. Valuing People highlighted the fact that most health care for PWLDs had always come from mainstream health services. Now GPs were financially encouraged to identify their patients with LD and to carry out annual health checks. Liaison LD nurses were recommended to facilitate access of PWLDs to mainstream health services. In 2004, the Green Light Toolkit encouraged mainstream mental health services to audit how they served PWLDs, as many had continued to see this as the only responsibility of specialist services.
In 2006–7, Mencap publicised how LD patients were neglected by mainstream services and criticised staff attitudes there. The publication of Their Death by Indifference forced the government to commission a systematic review of deaths of PWLDs, which confirmed the high rate of potentially avoidable premature deaths. There was also a growth in the number of care scandals in the community. Several NHS Trusts had seconded their staff to community homes rather than transferring their employment and now a series of reports showed the dangers of this producing poor surveillance and allowing institutional abuse.8
The 2000s witnessed the growth of supported living as the model for meeting the residential needs of PWLDs. In some cases, this meant care homes legally changed into being blocks of rented bedsits. People with high support needs were often placed in individual placements with dedicated 24-hour staffing. The pressure on local authority budgets escalated dramatically. Day care also followed the trend for more individual services with day care centres being replaced by individually supported activities, though financial constraints often limited the hours and range of activities provided.
There were other legal changes. The Mental Capacity Act of 2005 (changed from the Mental Incapacity Act after pressure from People First) set out a clear legal basis for deciding care when a person does not have the capacity to decide. The Convention on the Rights of Persons with Disabilities was adopted by the United Nations in 2006 and came into force in 2008. This promulgated the rights of PWLDs to equality of opportunities in education, employment and family life. Its oversight committee advocated supported decision-making rather than substituted decision-making as occurs in the UK. The end of the decade saw the Autism Act 2009 – the only specific disability Act in England. The Equalities Act 2010 highlighted the need to make reasonable adjustments to enable equality of opportunity.
By the end of 2010, all the old long-stay hospital beds had closed, though some of the old sites had forensic beds or new ‘assessment and treatment’ units. There was a rapid increase in private hospital beds concentrated on a few sites for those PWLDs with mental health and/or behavioural problems and challenging needs. As an example, in the Bristol area the 3,400 hospital beds of 1960 had reduced to 12 NHS beds and 24 private hospital beds. In 2011, those private beds in Winterbourne View were closed following widely publicised reports of abuse. This triggered the national Transforming Care project to close most of the remaining private and NHS specialist beds for PWLDs. By 2015, there were no specialist hospital beds in the Bristol area.
Staff Changes with Community Care
The roles of staff working with people with ‘mental deficiency’ were defined by the operational needs of the colonies. With their closure, professionals working there were forced to redefine their role to work in the community. This was most marked for psychiatry and nursing.
Psychiatry
The colonies were supervised by the same national board that supervised the psychiatric asylums. This board required a psychiatrist to be in charge of a colony/hospital as in psychiatric asylums. However, the colonies dealt with training and supervision and did not deal with comorbid psychiatric disorders. If you needed psychiatric treatment, you went to the asylum.
When the new Royal College of Psychiatrists was created in the 1970s it considered abandoning ‘mental handicap’ as a psychiatric specialty, as the hospitals were closing. It was decided to transform the specialism into the mental health aspects of ‘mental handicap’. Publications on the special features of mental illness in ‘mental handicap’ started to appear during the 1970s,9 and over the following years the psychiatry of mental handicap became a flourishing specialty within psychiatry, with its own training schemes, and a subspecialty within child psychiatry was created during the new millennium.10 However, the specialty has remained defined by its treatment of people with intellectual disability rather than its more general skills in neurodevelopmental psychiatry.
Nursing
Mental deficiency nursing first became a specialty in 1919 when the Medico-Psychological Association (MPA) developed a training course and qualification. A nursing manual was published in 1931,11 known as the Green Book to distinguish from the Red Book of psychiatric nurses. The book was mainly concerned with causes of mental deficiency, basic concepts of training inpatients and ward management. Mental illnesses such as depression and dementia were not mentioned in the book and epilepsy took up less than a page.
Nurses were seen as ward managers and carers.12 The consequence was the 1979 Jay Report into the future of mental handicap nursing, which recommended the specialism change with community care to one based on a certificate in social services. As the hospitals closed, this change seemed inevitable as care homes did not advertise for registered nurses and few could maintain their nursing registration when working in care homes.
However, the Community Mental Handicap Teams still needed nurses, albeit ones who were more versatile. The early teams comprised only a nurse, a social worker and a part-time psychiatrist. Other clinicians and professionals were added later as patients moved into the community. In addition, nurses with expertise in mental illness and learning disabilities were required for the new specialist mental health services and liaison services for physical medicine.
As a result, the profession was transformed. The training courses changed and many existing nurses underwent further training in mental health, epilepsy, dementia care or behaviour modification. Like psychiatry, the nursing specialism changed to be closer to that of other nurses, with additional expertise defined by the health needs of the population they treated.
Care in the Community
The fifty years covered in this chapter saw the development of a wide range of community services and supports by different organisations. Local authorities now assess and fund care needs and provide safeguarding services rather than direct care. However, few PWLDs are in employment, despite this having been a target for fifty years.
As the LD hospitals closed, the skills of generic health services provided in the community became an issue. GPs are now expected to be able to assess PWLDs. Salaried dentists have increased in number to cater for PWLDs as they present special issues and take longer to treat. Some general hospitals now have liaison nurses to support staff working with PWLDs requiring assessment and treatment.
The early Community Mental Handicap Teams have tended to divide into two: one service providing support to GPs and the work of social workers, usually based within community primary care services; and the other dealing with ‘challenging behaviour’ and/or mental health aspects of care, often based within mainstream mental health services.
Conclusion
Just as the name of their condition kept changing (we now have disorders of intellectual development in the eleventh edition of the International Classification of Diseases, or ICD-11), services for PWLDs were also radically transformed between 1960 and 2010. The service started as one based on the eugenic model of confining and training nuisance ‘mental defectives’ in institutions built large to reduce costs with little provision for those who lived in the community. Over fifty years, the model became one of total inclusion as equals in the community with equal opportunities in employment, accommodation and family life. Policymakers had to negotiate a massive change of policy, service provision and associated funding mechanisms to do this. The frequent scandals of care probably helped provide impetus and funding.
During this time, there was a massive development in ideological models, including self-advocacy and safeguarding, as well as research into the causes of LD and how to empower PWLDs. Now the issue is how people experience the dream in reality. The law requires equality of treatment and lack of discrimination, but it is not clear if this will eliminate negative attitudes held by others.
For the author, there have been cycles of care: I was first the psychiatrist for a 200-bed hospital but with no empty beds and with little support for community emergencies. Eventually, I had a large supportive community team and an admission unit. Then, the community team came under four different employers who relocated their staff and the inpatient service closed. Continuity of care was lost and admissions could be 100 miles away. Now PWLDs have individualised direct support but the services around them are more fragmented, as is the case for anyone living in the community.
Key Summary Points
In 1960, services were based on ‘hospitals’ which had been mental deficiency ‘colonies’.
The 1970s saw the start of the recognition of a right to live in the community as equals.
It took thirty years to close the old hospitals and develop an entirely community-based service. This needed changes to policy, funding agencies and the benefits system.
This also involved changing the skills of previous staff and changing skills and attitudes in mainstream services.
We now have a rights-based system, which is more fragmented and more challenging for PWLDs to negotiate.
Introduction
In the UK, the number of deaths due to substances far exceeds other preventable deaths such as melanoma, suicide, road traffic accidents and AIDS, which total around 10,000 per annum. The death rate due to drugs in the UK is now the highest in Europe: opiate and cocaine deaths are at an all-time high (Figure 25.1). Alcohol is responsible for approximately 25,000 deaths every year and is now the leading cause of death in men under fifty years of age. Tobacco still leads to 80,000 deaths every year. See Box 25.1 for definition of terms used in this chapter.
Box 25.1 Terminology
The terms addiction and dependence will be used interchangeably, as will the terms ‘drug’ or ‘substance’.
The terms ‘drug’ and ‘substance’ cover those psychoactive substances that are legal or licit and commercially available (tobacco and alcohol) as well as those that are illegal or illicit.
These terms will also be used to describe ‘street’ use of drugs which includes:
drugs bought over the Internet;
prescribed medication (e.g. benzodiazepines, opiate, opioid and gabapentinoid drugs) used in a manner not indicated or intended by a medical practitioner; and
use of over-the-counter preparations such as codeine-based products (e.g. cough medicines, decongestants).
Illicit drugs include:
cannabinoids (tetrahydrocannabinol or THC and cannabidiol) and synthetic cannabinoids (‘spice’);
central nervous system depressants such as opiates and opioids (e.g. morphine, codeine, heroin; and buprenorphine, oxycodone, methadone, fentanyls);
stimulants (e.g. cocaine, crack cocaine, amphetamines and 3,4-methylenedioxymethamphetamine, known as MDMA or ecstasy, khat);
hallucinogens: lysergic acid diethylamide (LSD) and psilocybin (magic mushrooms); and
novel psychoactive substances (NPS).
The health, social and criminal justice systems currently in place are not able to provide the flexible response in which the public can have confidence and to which they can adhere. Moreover, vindictive policies which criminalise people with substance dependence are therefore also unlikely to yield positive outcomes as addicts are suffering from a clinical disorder which requires treatment and support rather than indiscriminate sanctions.1 Addictions exact a high price in preventable illness, disability and deaths and are a marker of deprivation and inequality.2
Social Epidemiology, Medical Treatment and Drug Laws: 1960–1990
Current policy ambition is to reduce use rather than the harms caused by substances, and tobacco consumption has decreased but alcohol consumption has doubled over the last fifty to sixty years. Deaths from liver disease have demonstrated a steep rise between 1970 and 2006, 80 per cent of which are alcohol related and 20 per cent due to viral hepatitis (see Figure 25.2). Alcohol consumption increased as it became more affordable and sales from corner shops and supermarkets for off-premises consumption became legal. The pattern of drug use, too, has changed markedly over the last 100 years. Between 1920 and 1960, drug use was very low and mostly by people with other conditions. The Dangerous Drugs Act prohibited the sale of drugs without a medical prescription.3 Medical prescription to addicts was allowed as a last resort. This came to be known as the ‘British System’.
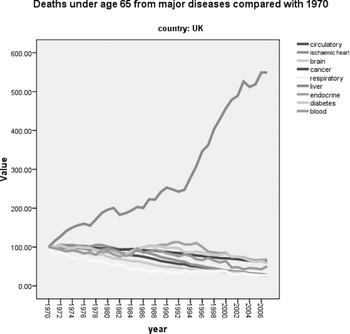
Figure 25.2 Standardised mortality rates from different diseases in the UK
Note the remarkable rise in deaths from liver disease as compared with other medical conditions: 80 per cent of these are due to excessive alcohol use and 20 per cent to viral hepatitis
From the 1960s, there was a new development: young drug users associated with the music scene appeared. Apart from the obvious link with entertainment, drugs such as cannabis, amphetamine or ‘uppers’ (in the form of an over-the-counter Benzedrine inhaler) and LSD came to symbolise their new ‘alternative’ identity with the hippy youth protest movement, its political values and new ways of dressing and behaving. This aroused suspicion and even anger in both the public and politicians. The Advisory Committee on Drug Dependence established the independent expert Wootton Committee review of cannabis and concluded that, despite the fact that the dangers of cannabis use had been exaggerated, it should stay illegal but in a lower class of the Misuse of Drugs Act 1971, that is, cannabis-related offending should be regarded as less serious than that related to opiates and cocaine and penalties be reduced.4 This advice was ignored and some forms of cannabis stayed in Class A and the rest in Class B.
During this time, the Home Office spotted that notifications of cases of heroin addiction had increased from 50 in 1958 to 1,299 in 1967 and that 80 per cent of users were under the age of 29. They were mainly young men who injected intravenously and were perceived as some threat to society. As this new cohort differed markedly from the few older middle-class people who were treated under the ‘British System’, the second Brain Committee in 1964 concluded that heroin use was a ‘socially infectious condition’.5 Its recommendations included new specialist addiction treatment units (Drug Dependence Units, or DDUs) under psychiatric leadership; compulsory notification of new cases; licences for doctors to prescribe heroin or cocaine at these centres; and, importantly, abstinence rather than maintenance with heroin or a substitute medication. Withdrawal treatment became the treatment of choice, and when this failed, addicts sought alternative treatment or drugs. This strategy appeared to curb the drug problem to an extent but not entirely.
Cannabis remained popular and convictions increased. During the 1970s, injection of barbiturate drugs became the most common form of death from overdose, but this subsided when Southwest Asian heroin began to make an appearance on the black market and benzodiazepines replaced barbiturates as they were considered a safer and non-addictive sedative medication at the time. Furthermore, as prescribed injectable amphetamine and illicitly produced amphetamine powder, which was either snorted or injected, became available, it became the most widely used drug after cannabis. Services remained focused on heroin users but, because of the HIV/AIDS epidemic, all injecting drug users became an increasing cause for concern.
A new heroin epidemic emerged in the 1980s when cheaper black market heroin was imported from the Golden Crescent (Iran, Afghanistan and Pakistan). This cohort differed in that now it was adolescents and young adults who were inhaling (‘chasing’) heroin, and although this route of use protected against HIV, many did turn to injecting and suffered serious complications. Use of cocaine and crack also increased and intravenous use of the benzodiazepine temazepam emerged as a problem. While it is estimated that in 1994 there were about 67,000 people in treatment for drug misuse, by 2007 there were 195,000.6
Following on from these developments, the revision of the Dangerous Drugs Act led to the Misuse of Drugs Act 1971.7 The Misuse of Drugs Act 1971 (MDAct 1971) has two separate dimensions, classes and schedules. Schedule 1 contains all drugs that have no medicinal value. Schedules 2–5 define the degree of safekeeping that different medicines require; this is because of the medicinal value of many ‘misused’ or recreational drugs.
Classes define the penalties for illegal possession. Three classes of drugs emerged: those continuing to enjoy recognition as medically useful but also associated with abuse (e.g. opioids, amphetamine); those that lost recognition as medicines and continued to be associated with abuse (e.g. cocaine, LSD, MDMA, magic mushrooms); and those that had never enjoyed recognition as medicines and continued to be associated with abuse (e.g. crack cocaine and ketamine analogues). Within each class, penalties intending to serve as deterrents differ in severity, depending on whether they are for possession for personal use, dealing, supply or importation. These penalties are meant to indicate the relative harms of the different drugs and act as a deterrent to use/supply. Severity of penalties is related to the potential of each drug for individual harm rather than cumulative social harm, which arguably would be more rational. They reflect the predominant UK policy of prohibition of recreational drug use that has been in place for nearly a century. As the costs of this undertaking in terms of social and personal damage are not inconsequential, there is a case for considering the proportionality of the penalty to the harms that may accrue both socially and individually.
Emergence of Public Health and Harm Reduction Approaches
There were a range of responses to the heroin epidemic of the 1980s, including the national campaign ‘Heroin Screws You Up’ aiming to prevent its initiation, and expansion of facilities for medical treatment. New multidisciplinary services offered residential rehabilitation. The objective was to persuade addicts to abstain. However, the epidemic of HIV/AIDS transformed this strategy. Accordingly, a flexible harm reduction policy was recommended by the Advisory Council on the Misuse of Drugs (ACMD). Implemented under the Thatcher government, it further expanded services and instituted needle exchange and methadone prescription. It was credited with the less than expected increase of HIV infections in drug users; in fact, the UK had the lowest in Europe. Despite these measures, during the 1990s heroin use continued to increase, especially among adolescents and young people, and ecstasy (MDMA) use started to materialise as part of the rave dance scene. This development caused significant disquiet and stirred up much debate within criminal justice, political and health settings.
Over the previous decades, illicit drug use itself was being increasingly conceptualised by younger people as ‘normal’ behaviour, while smoking was considered a more ‘deviant’ practice and perceived as a ‘drug’. It was argued that, had tobacco been discovered at the same time, it would not have been a legal substance. Restrictions on smoking and drinking and relaxation of the drug laws began to be examined. Continuing recreational use of licit substances, such as prescription drugs, added increasing complexity.
A model of public health, derived from that applied to tobacco, began to influence thinking on drugs and alcohol. Epidemiology became the research tool which underpinned the investigation of alcohol and drug use at the population level and represented a steer away from a strictly ‘medical’ model.
Thus, alcohol policies, though led by psychiatrists, also embraced a more varied group of disciplines and organisations such as the voluntary sector, the law and the police. This was because alcohol was conceptualised as a problem of the many, not just the few severely affected by the ‘disease’ of alcoholism. A landmark study by Edwards and colleagues in 1977 compared the impact of structured, individual advice, with the full treatment paraphernalia in use at the time. Advice, by and large, did as well as the already prevalent more complex treatment at twelve‐month follow-up.8 Encouraging the general population to reduce both smoking and alcohol consumption by ‘brief interventions’, mainly in primary care, was promoted.
Following the election of the Conservatives in 1979, this became problematic for politicians who were wary of imposing restrictions on advertising, increasing taxation and introducing licensing. During this time drug treatment had moved from primary care–based treatment to that which was led by psychiatric specialists. This was underscored by the need to notify the Home Office (rather than the Department of Health) of new cases, much like infectious disease control, as drug use was considered a ‘socially infectious disease’. Ideas around risk and the health of the population formed part of the thinking. Lifestyle, self-help and control as well as abstention were now entwined with the public health agenda. So, the impact of substance use on the whole population, as well as the individual who needed treatment, mattered.
This overall strategy of harm reduction was instituted after Labour came to power in 1997. It was implemented through an expansion of treatment programmes in 2000 which did reduce the rising death toll from opioids (see Figure 25.3). As penalties for drug offences were also rising, Drug Treatment and Testing Orders were introduced to engage users in treatment which meant that drug treatment became inextricably linked to criminal justice. In 2004, an Alcohol Harm Reduction Strategy was introduced to combat the massive rise in alcohol harms (e.g. Figure 25.2) and it was also based on the model of drug harm reduction.
In parallel, as the drug scene unfolded, since 1960 there had also been significant progress in the understanding of addiction and, to some degree, the associated harms to the individual and to society. The UK played an important role in the growth of this advancement. One key development in the 1970s was that novel terminology replaced the term ‘addiction’: the concept of ‘dependence’ was born and it could be applied to all substances. Dependence was defined by a set of criteria to diagnose or categorise the condition, be it because of drug, alcohol or tobacco use. Momentum around this conceptual breakthrough gathered so that, in due course, dependence came to be regarded as a chronic relapsing brain disorder.9
Towards an Understanding of Mechanisms and Harms: The Contribution of Neuroscience
Historically, addiction disorders have been portrayed – or understood – as a moral failing, a bad habit. Substance misusers may be treated in the acute phase of their illness in medical settings but, if left untreated, as they often are, they are then prone to poor medication adherence, poor control of common disorders such as hypertension and diabetes, increased risk of cancers and decreased effectiveness of treatments for pain. Substance misusers have not been considered worthy of first-class care compared to people with other preventable or treatable long-term conditions.
The remarkable contributions of neuroscience over half a century, 1960–2010, have demonstrated the biological basis of substance misuse, which can become a chronic medical condition, much like diabetes and hypertension. Recent research has demonstrated that a drug that induces dependence initially produces changes in reward neurotransmitters and neural circuitry which are (perhaps permanently) affected after repeated use. Eventually, the user loses control due to the development of negative physiological and emotional states and habit entrenchment. This neuroscience-based analysis in no way precludes an appreciation of the social, cultural and political factors that influence initiation and continuation of substance use.
Over this time, effective and innovative pharmacological treatments have forged ahead and continue to do so. There is a diversity of medications based on detailed knowledge about how they block the action of drugs such as opiates, stimulants, benzodiazepines and cannabis. Methadone has been and continues to be prescribed to those with heroin dependence and nicotine replacement to tobacco smokers. Newer medications such as buprenorphine and naltrexone for opiate dependence and acamprosate for alcohol dependence now form part of the pharmacological treatment options available. Psychological treatments, too, have found favour with service providers, and a combination of psychosocial interventions and medications are often recommended.10
It has become much clearer that the lack of response to treatment, rather than being due to poor character, lack of willpower or self-control, has very likely been rooted in an inadequate understanding of the nature of the problem. Refusing to recognise that the provision of resources to effectively treat, research and educate professionals and the public about addiction diminishes legitimate optimism derived from this substantial body of research.
As important are fair and appropriate drug policies, that is, public laws and regulations which can be expected to reduce harms to society while minimising unintended consequences. This stance recognises that psychological, social and political processes may lead to exacerbate and even thwart access and responsiveness to appropriate treatment. It also acknowledges that the biological and psychosocial drivers of addiction are unlikely to disappear even if abstinence is achieved. Understanding of brain mechanisms can be translated within the individual and wider social context.
Drug Laws in the UK: Lessons Learnt?
The justification for the illegality of many drugs is that they are harmful and hence criminal sanctions are necessary to reduce the harms to society and to individuals because they will act as a deterrent to their use.
For the last sixty years, the UK drugs policy has been controlled under two Acts of Parliament. Medicines are controlled under the Medicines Act and recreational drugs under the Misuse of Drugs Act 1971. In practice, many drugs – for example opioids, ketamine, benzodiazepines and stimulants – are controlled under both Acts which makes the position unnecessarily complicated as they come under the control of two different ministries of state.
Up until the early 1970s, rather than the policy debate around the drug laws centring on harms, it was focused on the morality of drug taking. In an attempt to redress this to some extent, the Misuse of Drugs Act in 1971 was introduced. This included understanding of the perceived harms caused by drugs, but they were not as well understood then as now. The ACMD was established to ‘keep the drug situation under review and to advise ministers on the measures to be taken for preventing the misuse of drugs or for dealing with problems connected with their misuse’. One of its key objectives is to decide on the relative harms of drugs and so locate them within the classes A, B and C.
Since 1971, there has been some movement of drugs between classes. Ketamine and GHB have come under the control of the Act. Methamphetamine has moved from Class B to Class A. Magic mushrooms have been made Class A and benzylpiperazine Class C. Cannabis has moved from Class A/B to C and then back to Class B. Until 2009, all governments had followed the advice of ACMD, but then, for the first time, their recommendations about cannabis and ecstasy were not heeded.
The public, policymakers and scientists need to act in unison to produce an evidence-informed, balanced and workable response as substance use and misuse remain a feature of everyday life in the UK today. Arguably the most important example of the divergence between science and policy is in the classification of what constitutes a ‘legal’ or ‘illegal’ drug. Alcohol, which is, of course, legal and widely available, produces considerable harm. Tobacco, too, is highly addictive and harmful but legal. Cannabis, on the other hand, remains illegal in many countries following the ban in 1961 by the UN convention but does relatively little harm.11 As another example, some ‘drugs of abuse’ have medicinal value – for example, opioids, benzodiazepines, amphetamines and constituents of cannabis – so the regulations make allowance for these. However, other drugs such as psychedelics (e.g. psilocybin) and MDMA with lesser harms and arguably with therapeutic potential for alcohol dependence, obsessive-compulsive disorder and PTSD (post-traumatic stress disorder) are not currently available legally.12
This issue has been examined in a multi-criteria decision analysis incorporating sixteen parameters of health and social harms of different drugs as illustrated in Box 25.2.13 The results demonstrate a striking lack of correlation between harms and the degree of prohibition (see Figure 25.4). This has been internationally replicated in Australia and Europe.
Harms to users:
Drug-specific mortality
Drug-related mortality
Drug-specific harm
Drug-related harm
Drug-specific impairment of mental functioning
Drug-related impairment of mental functioning
Loss of tangibles
Loss of relationships
Harms to others:
Injury
Crime
Economic cost
Impact on family life
International damage
Environmental damage
Decline in reputation of the community
One key element underpinning the value of systematic harm assessment of different drugs is that the availability of less harmful drugs leads to lower levels of harms to users. One of the most remarkable natural experiments that support this was the rise and subsequent fall of mephedrone in the UK (see Figure 25.5). This synthetic cathinone was legal in 2008 when it became popular in the UK. Within a few months, it had commandeered a significant part of the recreational stimulant market. This led to huge media hysteria with exaggerated claims of harms that, in effect, forced the Labour government to ban it just before the 2010 general election. Several years later, it became clear that mephedrone use had very significantly reduced deaths from cocaine and amphetamines. It appears that a significant proportion of the users of these drugs had switched to mephedrone, probably because it was legal, easily available and comparatively safe. Once mephedrone was made illegal, they switched back to their original stimulant and deaths from cocaine and amphetamine have reached all-time highs.
At this point, it is worth noting that the use of tobacco and alcohol products falls under separate age of purchase controls and taxation and are regulated food or commodities.
As the historical overview outlines, the profile of users changes as do the type and pattern of use of substances changes over time. Substance users can be very variable in terms of social status and health conditions. They have multiple needs, including being stigmatised, socially deprived and having traumatic life histories, mental health problems and living on the margins of society: the homeless, migrants, refugees and asylum seekers.
Substances are now commonly consumed in combination, and some combinations are more dangerous than others. New drugs emerge and, sometimes, if a particular drug becomes difficult to obtain because of either a change in the law or reduced supply, a more potent drug is developed. Several examples of this are cannabis and heroin which have been supplemented by synthetic cannabinoids or fentanyl. Very often users are not aware of what precisely is contained in the drugs they are using and so are not aware of the risk to which they are exposing themselves. Laws and policies need to take account not only of the type of drug and extent of use but also of these changing profiles of both drug and user.
Future Directions: 2010 and Beyond
In 2007, Sir David King, former UK chief scientific adviser, predicted improved treatments for addiction and other mental health disorders and the development of newer recreational drugs, some of which may lead to fewer harms and lower risks of addiction than the substances in use today.14
In 2009, one of us, David Nutt was dismissed as Chair of the Advisory Council for the Misuse of Drugs after pointing out that current government policy and the Misuse of Drugs Act 1971 were not evidence-based. Specifically, he commented that among the most harmful drugs in the UK were legal ones – that is, alcohol and tobacco – and the current government approach to focus on ‘illegal’ drugs was a missed opportunity to reduce overall drug harms. His removal was justified on the grounds that, as the chief government advisor, he should not be opposing government policy which failed to acknowledge that these were drugs.
Since then, with the advent of ‘austerity’, the UK has witnessed the decimation of treatment services for drugs, alcohol and smoking cessation, with numbers of consultant addiction psychiatrists and trainees dramatically reduced.15 This is a false economy: the stark increase in deaths is a chilling reminder of the gravity of the state of play.
There have been new issues and new substances as well as new groups of substance misusers. While much of the debate has centred on younger people, including children and adolescents, attention has recently turned to older people who are misusing cannabis and heroin as well as over-the-counter and medically prescribed medications.16 For example, there is now an appreciation that addiction is a lifetime problem for some and accumulating evidence that older people are vulnerable to the impact of legal and illegal use.17 In addition, we see the emergence of an ever-growing number of designer ‘novel’ psychoactive substances, available through the Internet; the popularity of e-cigarettes (vaping) for many substances apart from nicotine; and the changes in the legal status of cannabis so that it can be prescribed as a medicine. There is exciting potential for the development of new pharmaceutical agents for the treatment of substance misuse.
What half a century has shown us is that, overall, deaths from substance use have risen. There are a broad range of factors that contribute to this sad situation. The last years can be characterised as having seen prohibitionist developments in UK drug laws, while those evidence-based policies that could reduce the use of alcohol, especially minimum unit pricing, have not been introduced universally. Scotland and, recently, Wales have introduced these changes and preliminary data from Scotland suggest a decrease in alcohol use and its harms. However, in England, encouraged by the drinks industry, the government has resisted any change. There have been some significant steps forward in that smoking advertising has been banned and there are restrictions on smoking in public places, bars and restaurants, but the alcohol industry has managed to avert similar controls. These strategies have failed to achieve their goal and sometimes have even led to the development and use of more harmful substances. Particularly disturbing perhaps is that the Schedule 1 controls make it very difficult to use certain drugs for medical research.18
As is the case in many countries now, policy regarding substances is best placed within health care departments rather than the Home Office. For example, in the Netherlands, testing and regulated access to some substances has largely eliminated deaths from new recreational drugs; and in Portugal, the provision of appropriate comprehensive treatment interventions and facilities has significantly reduced opioid deaths. Further examples include prescription of medicinal cannabis as an alternative to opioid analgesics and the development of safer injecting/drug consumption rooms for those who have tried other methods.
Conclusion
The last sixty years has been an extraordinarily dynamic period in terms of both the rapid march of scientific progress and the changing landscape of drug use, drug harms and drug policy. It is fitting to end with prescient excerpts from an interview by Griffith Edwards, the quintessential figure in addiction psychiatry in the UK between 1960 and 2010 and editor-in-chief of the journal Addiction between 1979 and 2004:
Addiction science at its most productive knows no substance boundaries. There is great benefit in comparing across substances the mechanisms of dependence, distributions of consumption, treatment processes, policy and control responses.
He valued:
Daring to provoke debate, but with respect for everyone’s opinion.
He summarised key components as follows:
Our agenda themes (include) to encourage debate on the ethical dimension (in journal publishing), the relationship between science and policy, to promote internationalism (and) enhancing the quality of science.19
Key Summary Points
Substance use and misuse remain a feature of everyday life in the UK today. They are a cause of death and disability and a marker of deprivation and inequality. The health, social and criminal justice systems currently in place are not able to provide the flexible response in which the public can have confidence and to which they can adhere.
While much of the debate has centred on younger people, including children and adolescents, attention has recently turned to older people who are misusing cannabis and heroin as well as over-the-counter and medically prescribed medications.
The remarkable contributions of neuroscience over half a century, 1960–2010, have demonstrated the biological basis of substance misuse, which can become a chronic medical condition, much like diabetes and hypertension.
There is exciting potential for the development of new pharmaceutical agents for the treatment of substance misuse.
An aspiration we have is towards a new public understanding of addiction through education so that people can make informed choices based on realistic policies.
Introduction
Today, in the UK, homelessness is a hot topic. In 1960, it was not. One memory of my first few weeks in London in 1971 was of large numbers of men sleeping on the streets ‘under the arches’ in Charing Cross. Very few people at the time really seemed to view this as a problem. The prevailing view was that most homeless people were alcoholics who had chosen to live like that. There was, therefore, nothing you could do for them, so it was pointless to try. Unbeknown to me, there were thousands more homeless men (and some women) living in the deteriorating remnants of the workhouse system and nineteenth-century dosshouses for the poor. Insofar as homelessness and mental illness were thought of at all, they were seen as different phenomena, with little or no connection between them. Back then, mental health professionals were preoccupied with new developments in pharmacological and group interventions – and, of course, the issue of mental hospital beds, which had been closing since 1955.
Background
There is a historically documented association between homelessness and mental illness.1 In England and Wales, throughout the nineteenth century some 20–25 per cent of all known pauper lunatics had been accommodated in workhouses rather than asylums.2 However, in 1960 the stereotype of the single homeless man (for most homeless people at that time, then as now, were men) was that of the alcoholic. Most were not sleeping out on the street but were accommodated in one of the many large hostels for homeless men (and a few women) that punctuated the urban landscape.
Little research had been done in this area by psychiatrists or anyone else. Americans had suggested in 1939 that mental illness was more common in what they called ‘the disorganised community’.3 Two roughly equivalent descriptive classifications of the homeless were constructed, describing three categories of itinerant workers, itinerant non-workers and non-itinerant non-workers. An American sociologist called these respectively hobos, tramps and bums;4 and, thirty years later, a French psychiatrist described such groups as ‘errants, vagabonds and clochards’.5 These arbitrary and stigmatising classifications served neither to clarify issues nor to provoke further thought or research. The few academic papers concerning the mental health of homeless people were focused on alcohol problems.
Hostels for the homeless were situated in the middle of working-class areas of housing. Local people had learnt to tolerate rather than love them. They might be ‘reception centres’ (see below), Salvation Army hostels or Rowton hotels, established in Victorian times for the working poor. There was usually no formal connection between these institutions and local health services, apart from the occasional appointment of a visiting GP at some of the larger hostels, such as the Camberwell Reception Centre. Their residents were often as hidden in these institutions as they would have been in any of the large mental hospitals.
The first sign of interest was a UK paper in 1956, which looked at psychiatric admissions to a south London observation ward.6 Of these admissions, 8 per cent were of ‘no fixed abode’, a synonym for homelessness which continues to be used (and misused) to this day. This was a much higher proportion than would have been expected from the numbers of homeless men in the local area. A third were diagnosed as suffering from schizophrenia, mostly with delusional ideas; and those with this diagnosis tended to be living in the most impoverished circumstances, such as night shelters, rather than common lodging houses. The author suggested that
When he falls ill, the down and out should, ideally, be treated in a separate institution … where his environment was as near his normal habitat as possible. He would then be more likely to stay … it would be an advantage if he could be committed to the institution for a definite period, and as so many appear in court, this should be possible.
This was the first clear acknowledgement of excess morbidity for psychosis in the homeless and the first call for a specialist service – but one that remained unheard for thirty years.
The 1948 National Assistance Act, passed by Attlee’s Labour government, had formally abolished the Poor Law system that had existed for four centuries, where the only recourse for the indigent had been the workhouse. The Act established a safety net for those who could not work and could not pay national insurance contributions (such as the physically handicapped, unmarried mothers – and the homeless).
As part of this effort, it also established the National Assistance Board (NAB) so that ‘persons without a settled way of living may be influenced to lead a more settled way of life’. In other words, it aimed to reduce or abolish homelessness. The Casual Wards of the old workhouses were rebranded as ‘reception centres’ to provide temporary accommodation The high levels of employment at the time and the provisions of the new welfare state meant that demand for such beds plummeted and the NAB closed 136 of the 270 centres it had taken over. By 1970, there were just seventeen left. However, echoes of the workhouse remained. There was still a ‘work task’ that had to be completed before an individual could leave after an overnight stay, and conditions were still miserable. A study of reception centres as late as 1968 revealed that residents had suffered from severe malnutrition.7 Conditions in other large hostels were often no better.
The Act did theoretically have the power to keep people off the streets, but problems remained. In 1966, a pair of Birmingham psychiatrists reported that 23 per cent of men admitted to their urban acute psychiatric ward were of no fixed abode and that this proportion seemed to be rising quickly.8 Of these homeless patients, 74 per cent had had previous hospital admissions. The authors were driven to comment that ‘Their plight is evidence that the initial enthusiasm evoked by the new act (1959 Mental Health Act) for the discharge of psychotics into the community was premature and has resulted in the overwhelming of community services’. However, they acknowledged that this was not the whole story. They noted the housing shortage created by the closure of ‘lodgings available for persons of no fixed abode’.
In 1968, Griffith Edwards and his team interviewed the entire population of the Camberwell Reception Centre – one of the largest homeless hostels in the country.9 He found that 25 per cent of the residents had been previously admitted to a mental hospital – and this was equal to the proportion of those with alcohol problems. This was, perhaps, the first epidemiological evidence to challenge the idea that alcoholism was the cardinal mental health problem of the homeless man.
Although we are focusing on homeless men, it is worth mentioning the furore that was stirred up in 1966 by a BBC television play called Cathy Come Home. It portrayed a young working couple who, due to accidents and the rigidity of legislation and provision, move from a settled, self-sufficient domesticity to street homelessness and separation from each other and from their children. This created a media storm and encouraged support for Shelter, a housing charity that had been formed just before the programme was broadcast. It also prompted the foundation of the housing charity Crisis and was named in 2005 as the UK’s most influential TV programme of all time.10
Yet, for all the concern this programme aroused, the only practical difference it really made was that homeless fathers could now stay with their wives and children in hostels. It did not really touch the single homeless person. One specific problem was the limited access to medical care in these institutions. This meant that mental health needs would not usually be identified unless the person were to behave in a violent or disruptive way. The subsequent response would usually have been ejection from the hostel rather than a referral for a medical assessment.
At the end of the decade, a survey of a Salvation Army hostel in 1969 noted that it had been ‘conducted in an area with good psychiatric after-care services and an active local authority Mental Health Department. There is one psycho-geriatric hostel and one hostel for the subnormal, but no hostel for discharged psychiatric patients.’11 The Salvation Army was serving as an unacknowledged, de facto aftercare service for many patients discharged from psychiatric wards (see Figure 26.1). They concluded: ‘In our survey, 34 per cent of the residents had been in mental hospitals and 20 per cent were schizophrenic. It is surely not right to unload onto a voluntary organization, whose function is not to act as a therapeutic agency, patients who still need community care?’ Willing but untrained housing workers were shouldering the burden of supporting those who should have been supported by mental health services.

Figure 26.1 Salvation Army hostel, 1985
1970s
Occasional enthusiasts continued to take an interest. A doorstep survey of two Salvation Army hostels for men found that 15 per cent of the residents had a diagnosis of schizophrenia and 50 per cent had a personality disorder.12 On this occasion, both hospital and community care were criticised: ‘The small number of schizophrenics who were receiving treatment suggests both a failure of community care and inappropriately early discharge.’
David Tidmarsh and Suzanne Wood restated the idea that there might be ‘a need for services for the destitute men and women at present residing in common lodging houses and reception centres’.13 They showed that, on a given night, around 150 men, mostly with schizophrenia and without contact with services, were sleeping in the Camberwell Reception Centre. Ironically, this ‘invisible asylum’ was just over a mile from the Maudsley Hospital, a major centre of British psychiatry.
Robin Priest’s 1976 Edinburgh survey took a more sophisticated approach. He compared a general survey of the homeless population with those who were admitted to psychiatric hospital.14 He noted the unusually high prevalence of schizophrenia in the homeless population (32 per cent) but also that the prevalence of schizophrenia was greater in the general homeless population than in the subgroup that had presented to psychiatric services for treatment. Homeless men outside hospital were more likely to suffer from schizophrenia than those in hospital. So those with schizophrenia appeared to be less likely than their peers with other diagnoses to find their way to hospital treatment.
In 1977, parliament passed the Housing (Homeless persons) Act.15 For the first time, this placed a statutory duty on local authority housing departments to permanently house some categories of homeless people, if that person had been found to be:
In priority need (including vulnerability).
Unintentionally homeless – that they had not made themselves homeless.
Connected to the area – ‘local connection’.
It sought to provide for:
Those in ‘priority need’ for rehousing, regarded as ‘fully homeless’ and deserving of support. These were households with, or about to include, a dependent child.
‘Vulnerable’ lone people, or households without children, who could not reasonably be expected to fend for themselves, such as frail older people or those made homeless by an emergency – such as a fire or flood. Such households could be rehoused in local, funded social housing.
Under these criteria, people who were homeless, but did not appear particularly vulnerable (and did not have dependent children) were viewed as being able to support themselves. They came to be known as ‘single homeless people’ or as ‘non-statutory homeless people’, as they fell outside the main provisions of the new legislation and so were only entitled to advice and assistance from the local housing department. Homeless mentally ill people should have fitted well into the ‘vulnerable’ category, but three issues complicated matters, each of which I saw operating during my years of clinical practice:
It was often hard to establish vulnerability in someone with a mental health problem, especially if they were not in contact with a psychiatric service.
If, as a consequence of their mental illness, someone had behaved badly, not paid their rent or had neglected the care of their accommodation, it was easy for them to be viewed as having made themselves ‘intentionally homeless’. They would then find themselves outside the provisions of the Act.
Even if a person had been sleeping on the street in an area for many years, it could be argued that, as they did not have an address, then they did not have a local connection – and so, again, they fell outside the scope of the Act.
Moreover, the Act was only a general statute. A Code of Guidance was provided, but this left considerable room for interpretation. If you could not make your case, you were excluded from the provisions of the Act. This was particularly problematical with the criterion of not having made yourself intentionally homeless, containing as it did an echo of the notion of the ‘undeserving poor’. The effectiveness of such provision was further challenged, in 1995, when it was ruled that local authorities could discharge their obligation by providing merely temporary accommodation.16
1980s
The Thatcher government of the 1980s created the right for tenants in England and Wales to buy their council flat. This was couched in terms of extending to everyone the right to have your own home, even those on low incomes. Although it was seen by many as a cynical attempt to buy working-class votes for the Tory party, it proved popular with those at whom it was aimed.17 However, it also kick-started a drastic reduction in the social housing available to those who could not afford commercial rents, either because they were not employed or because they could not earn enough, even in full-time jobs. Thereafter, homelessness increased. Households accepted for assistance under the terms of the 1977 Act doubled from 53,110 households in 1978 to 112,730 in 1987 – and this rose to a peak of 144,780 in 1991.
At the same time, a silent and unpublicised process had begun – the closure of the large old hostels for homeless men and women. Much was written both for and against the closure of mental hospitals from the 1960s to the 1980s, and it was a matter of public knowledge and open debate. However, over the years from 1980 to 1995, the traditional large hostels for the homeless were also closed, with little public discussion or debate. This affected not only the Department of Health and Social Security (DHSS) reception centres/resettlement units but also Salvation Army hostels, Rowton houses and night shelters. The closures took place for a variety of reasons, similar in many ways to those leading to the closures of mental hospitals.
In London, in 1981, there were 9,751 bed spaces in the wider network of direct-access hostels, 6,000 of these in large, traditional hostels for the homeless. The London Boroughs Association (LBA) described them as ‘at once a resource and a problem’:18 a resource because of the shelter provided; a problem because of the often-appalling physical conditions and catastrophically inadequate staffing. This was illustrated by a crisis in 1983, when local authorities directed the owners to improve conditions in three Rowton houses – and the company promptly threatened to evict all the residents.19 The local authorities subsequently bought the three hostels, intending to close them within five years.
Nationally, the DHSS had wanted to close resettlement units for some time.20 It took the view that centrally funded institutions were inappropriate in an age of local social services and housing departments. Such large institutions were also seen as unsuitable places for influencing people ‘to lead a more settled way of life’, to use the original words of the NAB. So the decision was taken to close all the resettlement units and to replace them with locally run projects, with a system of grants to encourage voluntary sector organisations and local authorities to take on this task.21 The closures started with the Camberwell Reception Centre, the largest of the old NAB reception centres, in September 1985.
The LBA report had recommended the opening of 600 beds each year to replace the old hostels but acknowledged the financial and planning difficulties that such schemes faced. Belated enforcement of fire regulations led some hostels to reduce in size and others to close. By 1985, the numbers of direct-access bed spaces had declined to 4,885 and, by 1990, to around 2,000.22 The 900 beds of the Camberwell Reception Centre, all direct-access, were replaced by only 62 direct-access bed spaces, the rest being in specialist, referral-only, units. Across the board, 75 per cent of direct-access hostel spaces were lost during the 1980s. There was much good practice in the resettlement schemes for the existing residents of these hostels; but the loss of direct access beds without much in the way of equivalent provision did make it harder for a street homeless person, without resources, to get accommodation for the night.
There was, however, some official and academic interest now developing. Helping Destitute Men was a book written by a psychiatrist and a nurse and published in 1980. It commented on the presence of mental disorders in St Mungo’s hostels but did not remark on them further, focusing instead on the sensible notion of rehabilitation for homeless hostel residents rather than simple containment.
Single and Homeless was a major report, commissioned by the Department of the Environment in 1982.23 It covered a wide range of data and listed mental illness as a single category with no further details. It reported levels of mental illness which, if they included depression and anxiety, would have been unremarkable in a primary care sample. However, the methodology used meant that it would probably have missed much of the psychosis present in hostels. Their profiles of ‘types of homeless people’ included a drinker but no one with a mental illness. So an opportunity was missed for increasing awareness of the connection between homelessness and mental illness. However, across the Atlantic, there was a burgeoning literature developing which drew a strong connection between their process of deinstitutionalisation and excess rates of mental illness among their homeless populations.24
In the middle of this decade, and while this process of closure was going on, another Salvation Army hostel was found to have a third of both its residents and new arrivals with a diagnosis of schizophrenia;25 however, some change was coming. In 1987, an outreach team to the large hostels in Lewisham and North Southwark in south London was established. The Psychiatric Team for Single Homeless People (PTSHP) consisted of two nurses, one psychologist, an occupational therapist and a trainee psychiatrist (me).26 It provided a service to several of the large hostels that would soon be closing, but the question was asked, would this extra effort – or outreach as it has come to be known – be worth it? To answer this question, referrals were randomised into a treatment group – to whom the team would provide a clinical service – and an advice group – whom the team would assess and then advise the hostel nurse as to appropriate referrals to make. At the end of both three months and the year, the numbers remaining in the treatment group were significantly higher – as one would have hoped.
1990s
By 1990, Jeremy Corbyn – at that time a rebellious backbencher – was challenging Mrs Thatcher in parliament over the increasing levels of London street homelessness.27 Although many felt that this was a consequence of the psychiatric deinstitutionalisation, the evidence suggested that it had more to do with the hostel closures of the 1980s.28 The homeless mentally ill were clearly vulnerable both to deficits in health care and to inadequacies in other systems, such as housing. Whatever the cause, the Conservative government then decided to fund the Central London Homeless Mentally Ill initiative.29 This consisted of several multidisciplinary mental health outreach teams in five locations across central and east London. Their scope was widened beyond hostels and incorporated the ideas of assertive outreach – but the work was directed at those who were not in touch with services at all.30 Nurses, social workers and psychiatrists found themselves working in homeless day centres, squats, parks and even on the streets. This proved successful and three of the original teams are still functioning.
One of these, the START team, in south London, established a close working relationship with Thames Reach, a local homelessness charity (see Figure 26.2). Independently of the NHS, they had set up three housing projects in the same area, specifically for people with severe mental health problems who were sleeping out. The stage was set for a rich collaboration between the two agencies. A person with schizophrenia who was sleeping out could now be offered a small flat to move into without going through the usual accommodation ‘ladder’ – an almost ‘housing first’ set-up.31
A Labour government came to power in 1997 with a rather different set of ideas about social problems. Essentially, they drew on the notion of ‘social exclusion’, derived from French social science ideas about the nature of poverty.32 This term might be assumed to be part of a set of left-wing or even socialist views of poverty. However, this version was, perhaps, a more a liberal-democratic idea. It viewed the marketplace as the weighted centre of society – and proposed, at least in part, to ‘improve’ the marginalised so that they can now play a full (or fuller) part in society. So, although society may be reshaped to include the individual, there was also an emphasis on reshaping the individual to conform to society. Homelessness was defined as an element of social exclusion and major policies were put in place to counteract it,33 including the formation of a Rough Sleepers Unit in 1999, with a target of reducing the number of rough sleepers by two-thirds by 2002. The target was met in 2001 and there were no increases in the number of people sleeping rough in England until 2010; but, of course, in the years since 2010 there has been marked deterioration.
2000s
There were few further important political or legislative changes during the first decade of the twenty-first century. Yet, professionally, those providing mental health services to homeless people began to look beyond psychosis and substance abuse. Psychologists came to the table and Nick McGuire in Southampton pioneered the use of cognitive behavioural therapy (CBT) in high-risk homeless populations.34 John Conolly set up an outreach psychotherapy and ‘pre-psychotherapy’ service in Westminster;35 and the notion of the psychologically informed environment began to be explored. Given the reluctance of many homeless and socially excluded people to engage with mental health services, it made more sense to provide psychological services in hostels and housing projects.36 Other major cities such as Sheffield, Birmingham and Liverpool also set up mental health outreach teams for their homeless populations.
Conclusion
Attitudes and practices did change significantly between 1960 and 2010. Both homelessness and mental illness became increasingly matters of concern – and the high levels of mental disorder among homeless people were recognised.
At the beginning of this period, there was probably less visible street homelessness but this was because homeless people and people with mental illnesses were both, to a large extent, hidden. From the mid-1980s, increased recognition of the problem produced a range of high-quality and effective projects. Although these were mainly focused on psychosis, in the latter part of this period the psychological needs of those homeless people without psychosis were at last recognised and addressed, often using the explanatory idea of complex trauma.
Those of us working in the field have, I think, developed novel, flexible and user-centred services. What we have not been able to do is to change the economic and social forces that force people with mental disorders onto the street; and, perhaps, we have not changed the practice of psychiatry to the degree we would have wished. Patients are still discharged from psychiatric wards to the street and there is evidence that the majority of referrals to specialist mental health teams have previously been in touch with psychiatric services.37 There is still much work to be done, especially as we have seen the subsequent years of austerity undo many of the achievements accomplished during the period described.
Key Summary Points
Homelessness and mental health problems have been historically associated, but before the 1980s this connection was not generally recognised.
For many people with mental health problems, the large hostels for the homeless formed a parallel system of institutionalisation to that of mental hospitals. Unlike mental hospitals, they were generally situated within working-class areas of housing.
Attitudes and practices changed significantly between 1960 and 2010. Both homelessness and mental illness became increasingly matters of concern – and the high levels of mental disorder among homeless people were recognised.
In 1990, homelessness and mental illness became a political issue because of the increasing numbers of people visibly sleeping out in London. Although it was linked to psychiatric deinstitutionalisation, the evidence suggested that it had more to do with the closures of the large hostels in the 1980s.
From the mid-1980s, increased recognition of the problem produced a range of high-quality and effective projects which provided better access to mental health care for homeless people. These were initially focused on psychosis. In the latter part of this period, the psychological needs of those homeless people without psychosis were at last recognised and addressed, and the explanatory framework of complex trauma was introduced.
The ‘driver’ factors that create homelessness have remained substantially unaddressed.
Introduction
Stigma, fear and pity are deeply intertwined with the history of psychiatry and mental health. This chapter reviews their continued impact during the years 1960–2010 and reasons and efforts to move beyond them towards respect, engaged relationships and social inclusion. It draws on the journey, individual and societal, of a social psychiatrist that began well before I started my first trainee psychiatrist job in Dublin in 1992, a seminal year for UK psychiatry as described in the section ‘1992: Jonathan Zito, Christopher Clunis and NHS Mental Health Services’. This journey includes thirteen years’ experience as Associate Registrar at the Royal College of Psychiatrists.
I had learned at an early age that people with ‘mental problems’ were different. Back in the 1970s, my grandfather returned one day, upset, from a job as a draughtsman-builder at the local psychiatric asylum in midlands Ireland. He had grown up nearby in the rural poverty of 1920s Ireland, burying four of his six siblings to tuberculosis before they reached the age of eighteen, but even he was shocked by the living conditions he saw then in what locals called the ‘looney bin’. His job was a short-term ‘fixer-upper’ for the wards, perhaps someone had written a bad report or an official was coming to visit. He said he had been told to do the bare minimum lest questions be asked about expenses, and he wanted to do more: ‘these people have nothing.’ I still have the photo of the outside of the building. We were not allowed in.
A year of two later, at my Dublin secondary school, a classmate reappeared following his first psychiatric admission for bipolar disorder. It should have been a low-key return. Instead, our chemistry teacher started to call him ‘mentler’. Jim also used the term looney bin when he talked about it. I said nothing. The abuse continued from that teacher and fellow pupils and Jim did not finish school.
It was the 1970s and Ireland had public service TV ads urging its citizens to stop driving while intoxicated: ‘if you give car keys to a drunk man, you might as well hand a loaded shotgun to a lunatic.’ I heard language like this, and much worse, within my new profession for the seven years I trained in psychiatry. My last trainee job there was in North County Dublin, another old asylum. There were several long corridors with fresh-ish paint until the turns where the long-stay wards began – with bare, crumbling walls. Did they run out of paint, I asked? No, that is for when health ministers visit: they do not need to go beyond these points. My twenty-one years’ experience as a full-time NHS consultant has been different but also similar. In north-east London, a senior manager declined a cup of tea on a visit to our day hospital because we offered her the same cup ‘the patients’ drink from.
What the Public Thinks It Knows about Mental Disorders
My interest developed into why having a mental illness was so less deserving of recognition/status/empathy than a physical one. I often asked people, well or unwell, what they thought about specific mental disorders, and talked to many psychiatrists and other health professionals, before I started to read the scientific literature. I met many Irish then UK-based colleagues who shared the same interest in public engagement with what we do and how our patients’ lives are impacted by stigma and discrimination. One of my east London colleagues, Mark Salter, taught me that ‘psychiatrists are the only branch of medicine that need to read the newspapers and go to the cinema’. There was much to review.1 I read ‘factual’ media pages (print and broadcast, online content) and was guided by fictional representations.2 Rabkin reflected on responses to the three key messages of an innovative 1960s Canadian educational programme to promote understanding of mental disorders, namely that:
the range of normal behaviours is wider than often believed
deviant behaviour is not random but has a cause and can be modified
normal and abnormal behaviour fall on a continuum and are not qualitatively distinct.3
She concluded that ‘the third proposition was so unpalatable that the community eventually rejected the entire (six month) educational program(me)’.4
Taking Corrigan’s definition that stigma is a prejudice based on stereotypes leading to discrimination,5 one avenue of study is to explore the stated opinions of the general public towards people with mental disorders. To find out what public attitudes are, work has often used agreement with stereotypical statements as a measure of prejudice. Broader research examines other aspects of public negative attitudes, but here I focus on two: violence perceptions and pity.6 Their consequence (discrimination) causes considerable distress to individuals. Even minor avoidance or subtle rejection of people with mental disorders is significant.
Reconceptualisations of psychosis allow for the possibility that stigma-mediated events play a role in relapses of psychosis through the ways these events are evaluated.7 Appraisal of events is influenced by reasoning and attributional biases; dysfunctional schemata of self and the world; and isolated or adverse environments.8 We can hypothesise similar end results in people with the common mental disorders: anxiety and depression (albeit through different mechanisms such as lowering self-esteem or increasing anticipatory anxiety).9
Courting Public Opinion
The Royal College of Psychiatrists (RCPsych) in the late 1990s funded an anti-stigma campaign led by the late Arthur Crisp, professor of psychiatry at St George’s Hospital Medical School. It looked at available research and completed a pre-campaign UK-wide opinion survey.10 Changing Minds (aka Every Family in the Land) was run from RCPsych from 1998 to 2003; other campaigns followed, the most enduring ones being See Me in Scotland and Time to Change across England and Wales. These latter two campaigns, or more accurately social movements, continue and do things differently and better: they are user-led (experts by experience) with training and support for people with mental health problems to do media work; they start within communities, not ‘top-down’, using social plus traditional media when necessary; and they achieve key alliances (celebrities, sporting organisations, barbers, taxi drivers, artists). What is required is that, as a society, we now talk about mental disorders, mostly with a new progressive language (see Table 27.1).
| 20th Century | 21st Century |
|---|---|
| Mental illness | Mental health |
| Psychiatric patient, patients | Service user, experts by experience |
| Family, husband/wife/partner | Carers |
| Schizophrenic | Person/people with schizophrenia |
| Psycho, lunatic, nut job, etc.11 | Known to services, care in community |
Others have placed tackling practical discrimination at the centre of their campaigns, most notably Graham Thornicroft and his international collaborators.12 After all, people learn how to conceal racist and other negative attitudes and what they might tell researchers can be at variance with what they believe and how they act. Some have argued that softer language is no practical gain – and some activities, for example challenging distasteful media items, are both stereotype suppression (implying an unwanted rebound) and a distraction from a rights-based approach to reducing stigma.13 All great points but, three decades ago, we faced an even greater distraction.
1992: Jonathan Zito, Christopher Clunis and NHS Mental Health Services
Everything changed in 1992. On 17 December, Jonathan Zito (age twenty-seven) was changing trains at Finsbury Park Station (London) when a complete stranger, Christopher Clunis (age twenty-nine), approached him to fatally injure him without any provocation. In the subsequent Clunis Report,14 multiple service failures were identified, principally that no service took responsibility to follow up Clunis to maximise his treatment engagement (see also Chapter 23).
I started my first consultant psychiatrist job in Kent, England, in 1999 and the only item left by my immediate predecessor on my office desk was that report.15 The UK government fed on this. When mental health services were allocated extra resources from 1999 onwards (as were hospital accident and emergency departments (A&E), cardiology and cancer), it was to protect public safety and much less to treat mental disorders. The Zito Trust became one of several public bodies to call for more coercion in mental health services, and when it wound down its last chief executive said it had become a ‘victim of its own success’.16
I acknowledge the sudden nature of the violent act that stole Jonathan Zito’s life as well as the years of grief of his widow, family and friends. The aftershocks of the homicide, inquiries, government statements and media coverage combined, however, to turn community psychiatry into ‘scare in the community’. Widespread assumptions about the violent unpredictability of all aspects of psychosis generalised to other mental disorders, and these stereotypes hardened public attitudes.17
Jonathan Zito’s homicide spoke to the public’s worst fears that severe mental illness (SMI) was hidden in ‘normal people’ (think Norman Bates in Psycho, 1960); that psychiatrists were ‘too soft’ to insist on confinement or coercion; and that our treatments don’t work anyway. At the time, Brian Cooper called this the Iron Triangle of public anxiety and distrust of people with mental illness; an alienated tabloid press; and government policies focused on populist measures.18 There was no public appetite for evidence of the declining rates of homicides by people with psychosis over forty years,19 and so when the murders (sic) of Lin and Megan Russell occurred in 1998, committed by a stranger who had no psychosis, ‘something had to be done’.20 It remains hard to fathom the depth of government feeling during these years, such that politicians instructed the civil service (not clinicians) to invent a diagnosis and then legislated to treat it. The Dangerous Severe Personality Disorder (DSPD) diagnosis was conjured up and imposed on psychiatry and mental health. A couple of ‘treatment’ centres sprang up but, not long after, like the credibility of this ‘diagnosis’, vanished into a sad chapter of UK psychiatry (see also Chapter 28).21
A review of fifteen years of population-based public attitudes research identified differences between disorders, with worse attitudes towards addictions and schizophrenia than towards depression and anxiety. The key difference was perceived to be not ‘deviant’ behaviour but risk of violence.22 The first challenge of public education/engagement was to facilitate empathy by shifting the focus away from violence. Every time there was a high-profile story, we at RCPsych have ‘put out’ a small group of media-trained clinicians to counter with arguments about actual incidence of these homicides,23 with clear messaging on what is needed (well-resourced general adult psychiatry and community mental health services). Even 9/11 brought psychosis back into the bear pit of public opinion, when then home secretary Jack Straw called bin Laden ‘psychotic’ in an interview, adding that he ‘was picking [his] words with care here because whenever you use the language of mental illness, you get letters from people’.24 The same Jack Straw drove the DSPD agenda.
‘Behaving Strangely’
This vague, informal two-word descriptor remains the referral headline from my A&E colleagues. Even within mental health services, clinical work is bedevilled by colleagues failing to differentiate, as evidence and professionalism demand, between functional psychoses (e.g. schizophrenia or bipolar disorder), acute confusional states caused by metabolic and similar abnormalities (delirium) and recreational substance-induced severe but transient mental disturbances; and sometimes also autism.
Successive government policies to outsource NHS addiction services to charities have undermined training in this area and compounded difficulties in both identification and treatment of related clinical problems. One of the clear empirical research messages about violence is that it is true that with stranger assaults the aggressor is far more likely to be intoxicated than be suffering from a functional psychosis. This actuarial statement is never an argument against people with addictions or addictions services. It is an argument in favour of evidence-based anti-alcohol policies such as minimum alcohol pricing.25 At the time of writing (2021), only England has neglected to pursue this enlightened public health policy in the UK. In fact, resourced addiction treatment services that engage people, including treatment of comorbid mental disorders, are part of the solution to reduce societal violence due to alcohol and drugs).26
The core argument to reduce homicides by people with functional psychosis remains: work for less stigma and discrimination and people will be more likely to present to mental health services, engage well and take agreed medications. More stigma (hysterical media headlines, government legislative zeal) and they will more likely present to police than psychiatrists; take medication only under coercion; and use cannabis/other substances that increase the risk of violence. People will then present to services not ‘because they are suffering but because they are insufferable’.
Existential Crisis within Psychiatry
As a clinician who works full-time as a general hospital psychiatrist, seeing patients referred from A&E and medical and surgical wards, my greatest frustrations relate to having responsibility without power. Often, I return patients home to unspeakable poverty with few or no supportive relationships in their lives. I document but cannot ‘fix’ their medium-term risks of suicide, coming to physical harm or, much less frequently, a future impulsive moment of violence to others. I am at once responsible but lack the power to make the right changes happen.
As the century began, NHS services in which I worked received ‘new money’ to assist us to set up five new early intervention in psychosis and general hospital liaison services but frustrations increased as that money dried up or was wasted on needless layers of management (see also Chapter 12). Professor Sir David Goldberg in his lecture on ‘NHS psychiatry 1980–2006’, referring to mental health services and the overemphasis on fear of psychiatric patients, concluded:
This deterioration occurred despite (Treasurer) Gordon Brown’s new money: £172 million a year between 2001 and 2005. Overall, the King’s Fund estimate that 17 per cent of the new money was spent on local service developments, 32 per cent on pay and price infrastructure, and 46 per cent on the NHS Plan and modernisation funds. Furthermore, the National Survey of Investment 2004/2005 revealed a focus on forensic services at the expense of basic provision. Spending on secure and high dependency, access and crisis services and home support rose by 81 per cent, 79 per cent and 75 per cent respectively. The NHS invested far less on new buildings (17.0 per cent increase), CMHT (13.0 per cent), continuing care (11.0 per cent) and clinical services (10.0 per cent). In other words, the new money has been spent on the wrong things. Funds for forensic patients have been given marked preference over improving basic services.27
Hitting the Target but Missing the Point
More than half a century ago, Phillips speculated about the relationship of knowledge to stigma: ‘the increased ability of the layman to identify certain behaviours as mental illness does not necessarily imply changes in the way he will act toward persons suffering from mental disease.’28 Clinical experience has taught me that the A&E doctor who correctly identified psychosis among the behaving strangely cohort was never more empathic towards this group. Aimed at the public, from the biomedical corner, public talk of ‘brain disorders … biochemical imbalances’ was followed by a decade or so of raising awareness about mental health and well-being (whatever that is). It is hard to prove this hypothesis, but the more universally mental health has been discussed, and despite sound general advice (exercise more, value your friendships), the greater the distancing and neglect of people with SMI. A review of the literature has shown that the ‘illness like any other’ approach to the stigma of schizophrenia increases perceptions of violence and the public’s desire for more social distance.29
‘Beware Pity: It’s About Parity’
More recently, and with fewer ‘scares in the community’ stories gaining media traction, we see new images, literally the stock photo images in print and online of what journalists/subeditors think mental disorders look like – principally, ‘headclutchers’.30 These are individuals with their heads bowed, hiding their distress and their secrets in both hands, with fingers splayed. With a sense of mystery as to what led them to here and a loss of personhood, they evoke pity and discourage interaction with others. Anti-stigma campaigners have mounted a spirited response, and a BBC News account called for ‘more sympathy (sic) for those affected’.31 Even complementary newspaper articles that covered the former UK prime minister David Cameron’s declared ‘mental health revolution’ in 2016 gave us another headclutcher.32 This time, as usual, the money did not follow the rhetoric: anti-stigma talk was cheap.
My experiences of this decade in briefing journalists, lobbying in Westminster, and working with some trustees of UK mental health charities were similar. What I encountered was not rights-based, social justice mindsets but pity-led motivations. Perhaps as a short-term strategy asking for funding because ‘these people have nothing’ seems the only way to achieve what is needed. The public mood had changed (perhaps Jack Straw’s ‘letters from people’ has evolved to censure in the social media) and ‘these people’ are now thought to deserve our sympathy and a better deal. However, listening to the warm words of journalists, politicians and charity grandees, there comes to mind Prince Lampedusa’s response to Garibaldi’s revolutionary campaign to unify Italy in the novel The Leopard: ‘things must change so that they can stay the same.’
There is no need to read the stigma literature to know that high public perceptions of danger generate avoidance and more distance from people with psychosis. Equally, we would not like to be in a relationship or get a new job merely because someone felt sorry for us. Stigma-based discrimination is about social relationships, but those where there is a power differential (between stigmatiser and stigmatised): pity from powerful others is internalised and makes people more hopeless over time, just as it lowers self-esteem and has the potential to provoke depression.33
The employment example makes a wider point. Less than 15 per cent of people with SMI are in paid employment, lower even than low European comparisons. These scandalous rates are not about ability or potential; they reflect an abundance of employer sympathy (‘this job might be too much for them’) and a lack of empathy (to enquire of ‘them’ what adjustments might be needed, if any, to support them in this employment). We asked our early intervention patients with a recovered psychosis what they wanted. They said jobs, relationships and housing. Within the two multidisciplinary early intervention psychosis teams where I have worked with nurses, support workers and vocational rehabilitation specialists, I have seen many young people with psychosis achieve employment, often their first job. We assumed only that they would recover. On reflection, the very fact that we supported them to stay out of hospital, or the ‘looney bin’, helped employers see their potential not their deficits.
Pity Can Seriously Damage Your Health
Recent collaborations with ASH (Action on Smoking and Health) as part of the mental health smoking partnership have revealed another aspect of pity over parity. The Stolen Years report identified cigarette smoking as the main preventable cause of the seventeen-year average reduction in life expectancy among people with SMI. Seventeen years of life lost and the final years of life are blighted with cardiovascular disorders, stroke, respiratory illnesses and smoking-related cancers: the stolen years.34 As mental health Trusts went smoke-free (banning smoking on their premises), some psychiatrists called for ‘exceptions’. They cited human rights, but no one has a right to smoke in a hospital building. Next came the arguments that psychiatric patients were different from general hospital patients and that:
‘I couldn’t expect my patient to quit smoking during a crisis’;
‘If we grab their cigarettes, they will become violent’; and
‘It’s all they have … let them smoke’.
For me, this is three decades in one exchange: violence, pity and low expectations. In case I sound too severe, we do not ask people to give up (highly addictive) nicotine but are insisting that they do not smoke cigarettes in our hospitals. This is also about the rights of other patients and staff to healthy smoke-free environments. We provide nicotine replacement and multiple resources, including electronic cigarettes, as well as access to quit programmes that include varenicline. The evidence is clear: people with SMI want to quit just as much as any smoker and achieve high quit rates with the right options; and violence on psychiatric wards has reduced since the smoking ban.35
Conclusion
I was too young to interrogate my grandfather’s response to the inhumane conditions cited in the Introduction to this chapter; was it pity or might it have been what Patrick Corrigan calls ‘righteous anger’? Fifteen years after school made life hell for Jim, I met him when I was resident on call to the psychiatric unit where he had been sectioned (against his wishes). It was a quiet night for both of us and I made some tea. I did not tell him how sorry I felt for his life course, but I got the chance to apologise for my silence when others harassed him. He laughed it off and then told me some tales ‘from the other end of the hypodermic needle’. The worst of his experiences were outside health services, and he set me on a path of learning about poverty and inequality.36
Effective community mental health services require an understanding of the communities we serve. This goes beyond cultural and subcultural beliefs. The community’s main concerns (their safety, young people who self-harm, seeing ‘homeless people’ who look mentally unwell) will change over time. When governments and others exploit these attitudes, we (psychiatrists and other mental health professionals) need to call this out. The public wants to know and engage with psychosocial explanations of distress and mental disorders, even self-harm and suicide. Social psychiatry, now public mental health, encompasses an understanding of the factors (poverty and inequality, adverse childhood experiences, structural inequalities, discrimination and daily stress, etc.) that cause and perpetuate mental disorders. We must use this evidence to pursue prevention, ensure treatment plans are properly resourced and address underlying social causes of mental disorders.
Key Summary Points
Historical fears of violence by people with mental disorders increased in the final years of the last century. Science demonstrated falling UK homicide rates by people with psychosis, but inaccurate perceptions drove UK government policy instead.
As the public perception of violence subsides, we see increasing societal narratives of pity for people who lose their mental health; these will mostly serve to extend their exclusion and deepen inequalities. Pity makes people ill.
Actions to highlight and reduce stigma and discrimination have softened some attitudes, but mental health awareness is no substitute for actual engagement with people who have mental disorders and sustainable funding for those that need state support (housing, income) or health services.
Clinicians and partners in mental health reform have a duty to engage with local communities (and sometimes beyond) to achieve sufficient degrees of public engagement to prevent mental disorders by reducing the causes, principally poverty and inequality. These actions are just as important as providing fully integrated community mental health services.
Parity of esteem is never having to say you are sorry (for someone) but to collaborate/advocate for their rights.
It is lack of appreciation and understanding of this factor (psychopathic personality) which has often led to a great deal of prolonged, useless, faulty and even dangerous treatment.
Introduction
The Dangerous and Severe Personality Disorder (usually abbreviated to DSPD) richly funded ‘treatment’ programme was introduced in the late 1990s by the then Labour government. It attempted to combine psychiatric diagnosis and treatment for severe personality disorder, but its main aim was public protection. Unsuccessful attempts were made to enshrine the ‘treatment’ programme in law. They met widespread resistance on human rights grounds by psychiatrists and other mental health professionals as well as service user–led organisations and all failed.
The exact origin of the concept of the DSPD programme remains an enigma. I will try to piece together the strands, focusing mainly on political actors, while appreciating that some will be left hanging in the air. What I hope to elucidate is that initiatives taken by government without the profession approving are rarely likely to succeed.
In this account, I am appreciative of all the contributions made by those listed in the Acknowledgements section of this chapter and also of the very detailed and scholarly account in Max Rutherford’s Blurring the Boundaries, published by the Sainsbury Centre in 2010. This is one of a few documents published about the programme that can be regarded as completely unbiased. Most of the other published papers, including many from government sources, are tendentious and misleading. Although I would like to exclude our own published papers on the subject,2 I feel even they, despite attempts to be neutral, have a tendency to overstate in their attempt to correct errors on the other side.
Early History
The story appears to start on 9 July 1996. Lin Russell, a mother aged forty-five, was walking home with her two daughters, Josie, aged nine, and Megan, aged six, and their dog down a quiet country lane near Canterbury in Kent after a school swimming competition.
Out of the blue, they were attacked. A man tied them up, blindfolded them and then beat them all indiscriminately. They all died apart from Josie, who after a rocky rehabilitation, has, gratifyingly, almost completely recovered.
The case was difficult to resolve, but in July 1997, Michael Stone, a heroin addict at that time on probation, was arrested and charged with murder. There is still great doubt that he was the murderer and Levi Bellfield, the man convicted of the murder of Milly Dowler in March 2002, has also been accused of the crimes.
The shocking case of Lin Russell and her family is said to be the stimulus behind the DSPD programme. Why was it that a man who was recognised to be unwell, with diagnosed antisocial or psychopathic disorder, was allowed to be at liberty and yet remain a big risk to the public. Psychiatrists regarded these people as untreatable, but were they right and what could be done to prevent it?
In all my enquiries, there has been one consistent feature in the timeline. It was the attack on the Russell family, followed by the widespread public reaction, that initiated the implementation of the DSPD programme.
Political Action between 1997 and 1999
In Chapter 9, I report on an interview with the former Conservative secretary for health and social services, Ken Clarke, who, while not involved in the Department of Health or the Home Office at this time, still knew a great deal about what was going on at the heart of government. He maintains that it was the Labour government who initiated the DSPD programme and that the earlier Conservative (John Major) government of 1992–7 had no part in this.
Yet it could be argued that this is not entirely true. Throughout the 1990s, in the context of psychiatric deinstitutionalisation, there had been concern in the UK about the number of homicides carried out by people with severe mental health problems. The frequency of such homicides was alleged to be increasing but analysis of official data showed the opposite; homicides had been reducing at the rate of 3 per cent per annum over many years.3 It is not the purpose of this chapter to examine why the misleading impression was created but a considerable amount of responsibility can be placed on the publishers of tabloid newspapers who reported almost every homicide on three separate occasions: the time of the offence, the time of detention and a full and garish report of the trial. Because of the gap between each of these reports, the average reader would think that homicides were three times more frequent than they actually were.
Yet there had long been concern over the provision of services for mentally disordered offenders, and even Taylor and Gunn conceded: ‘There appears to be some case for specially focused improvement of services for people with a personality disorder and/or substance misuse.’4
The Conservative government of 1992–7, in the last throes of its chequered existence, felt it had to do something to address the widely perceived notion that highly dangerous people were milling around the countryside looking for victims. They were in the same position as Mrs Ramsbottom, who, in the Stanley Holloway sketch,5 following the unexpected departure of her son Albert into the stomach of a lion, protested: ‘Someone’s got to be summoned! So that was decided upon.’ This is not meant to be flippant. If there were going to be high-profile cases, the government needed to be able to point to action being taken.
The first summons came in the form of the Crime (Sentences) Act of 1997, introduced by the Conservative government but enacted by the Labour one. This introduced a new power for the courts, allowing them to attach a ‘Hospital Direction’ to a prison sentence. A new section was added to the 1983 Mental Health Act (45A) that allowed a prisoner to be moved to hospital from prison provided
(a) The patient is suffering from psychopathic disorder,
(b) The mental disorder (i.e. psychopathy) is of a nature or degree which makes it appropriate for the offender to be detained in a hospital, and
(c) Such treatment is likely to alleviate or prevent deterioration of the offender’s condition.
The new Labour government passed this Act in 1997, but it is important to note there has always been a provision for prisoners to be transferred to hospital (currently sections 47–48). Section 45a was a hybrid order that authorised the court to send a sentenced prisoner directly to hospital and then on to prison if they became medically fit before the end of their sentence. The implication of a transfer to hospital was that treatment could be provided for the individual if the doctors agreed. This became ‘the treatability clause dispute’. Put simply, the government’s view was ‘if a mental disorder exists and is treatable, why should this decision be left to psychiatric whim?’
Why the Treatability Clause Led Everyone Astray
When the Mental Health Act was passed in 1959 ‘severe personality disorder’ was in nobody’s mind but ‘psychopathic personality’ was prominent, mainly because of the influence of the Scottish psychiatrist and sometime president of the Royal College of Physicians (Edinburgh), David Henderson, who had done so much to bring it to public attention in his book Psychopathic States, published in 1939.6 As it had such a powerful effect after twenty years, it influenced the wording of the Act, defining psychopathic personality as ‘a persistent disorder or disability of mind (whether or not including sub-normality of intelligence) which results in abnormally aggressive or seriously irresponsible conduct on the part of the patient, and requires or is susceptible to medical treatment’. (It is important to note that this only referred to one of the three types of psychopathic personality that Henderson described: predominately aggressive; predominantly inadequate or passive; and predominantly creative.)
The problem was that this definition was, in the wording of its last clause, unworkable. It left unanswered a host of questions:
Do all psychopathic personalities require medical treatment?
Is psychopathic personality per se treatable?
Do psychopathic personalities that are susceptible to treatment automatically require it (the ambiguous ‘or’ in the last clause suggests this is optional)?
What does the Act suggest for those with psychopathic personality who are not susceptible to medical treatment?
It is this last question that led to much animosity. The argument came down to the level of psychiatric responsibility required for people with this disorder when not susceptible to treatment.
In 1998, Jack Straw, then Home Secretary, said on the BBC:
Twenty years ago psychiatrists were adopting what I would say what was a common sense approach to serious and dangerous persistent offenders. These days they have gone for a much narrower interpretation of the law. Quite extraordinarily for the medical profession, they have said they will only take on those patients they may regard as treatable. If that philosophy applied anywhere else in medicine there will be no progress whatsoever. It’s time, frankly, that the psychiatric profession seriously examine their own practices and trying to organise them in a way that they have so far failed to do.7
Robert Kendell, then president of the Royal College of Psychiatrists, and well known for his plain speaking, responded robustly, if not entirely wisely under the circumstances:
‘We are not very pleased with him, but even more important we are appalled by his ignorance. The Home Secretary cannot expect psychiatrists to do his dirty work for him.8
Yet Robert Kendell had an important point to make. Are all diagnosed patients required to be treatable and under care? One does not say to a palliative care physician looking after incurable patients, ‘you are a physician, you have to treat these patients, you cannot just allow them to die, jump to it’. This broad generalisation also assumed that the responsibility for dealing with dangerous offenders lay mainly, if not entirely, with the medical profession.
The Joint Policy of the Department of Health and the Home Office
The focus on psychiatrists’ practice only was soon realised to be a mistake and a joint approach was then suggested:
It is not just a problem for The Home Office but a problem for the Department of Health, for the prison service, for mental health services, and somehow or other we have to find a solution to that problem. The truth is we can only do that together.9
It was far from clear, however, who would lead on this. Someone had to take the initiative. It was Jack Straw at the Home Office, who recalls:
During my first eighteen months as Home Secretary I had seen a number of cases where obviously dangerous individuals were having to be released back into the community, notwithstanding the patent risk they posed, and the near certainty that they would commit further serious violence, because they had reached the end of their prison sentences, and could not be detained under the Mental Health Acts because their condition was not diagnosed as ‘treatable’.10
Jack Straw also denied that the policy came from advisors as Ken Clarke has suggested (see Chapter 9):
I think you have to give the responsibility to the Labour government. The trouble is with policies like this is that you now have this semi-presidential system where everyone listens to advisers and so when public opinion gets sufficiently animated new policies are introduced without ever having been thought through.
Straw firmly contradicted this:
Ken is wrong in suggesting that this policy came from advisers, or from ‘President’ Blair. It came from me. I would have told Tony what I was doing, (probably in writing) but I don’t recall any second-guessing from No 10. I was rather resistant to that, and in any event there was no need, as I was getting on to develop the policy.
He also underplays the influence of the health ministers in the generation of the programme:
At this stage I cannot say for certain whether I talked to Frank Dobson, but it is highly probable, as with Alan Milburn who took over from Frank in early 1999. I might too have discussed the matter with the Shadow Home Secretary. There was no reason why not.
In this area, support from the Conservative opposition was likely to have been forthcoming.
Straw also makes it clear that public protection was most prominent in his mind in introducing the DSPD programme and it was the Michael Stone case that initiated it:
I thought (and still think) that it was irrational that whether someone really dangerous could be detained in hospital depended not on any objective analysis of the risk they posed to the public, but on the state of psychiatric understanding and diagnosis for the time being.
My recollection is that I initiated the review within government, probably prompted by concerns expressed in the Commons and in the press. I am pretty certain that the most prominent case was indeed the Michael Stone one.
Why Have a DSPD Programme When You Just Need to Change the Law?
The DSPD programme was bound to be coercive, although it is fair to add that, at its very beginning at HMP Whitemoor, the first prisoners volunteered for the programme. The normal process at this point is to change the law. I had a hint of this developing in March 1997. Ann Coffey, MP, then the Labour opposition spokesperson on health, was recommended to accompany me on my community visits in central London in March 1997. She said she wanted to see ‘psychiatry in the raw’. This turned out to be rather more accurate than was envisaged. One of the patients we were visiting in Paddington was highly suspicious, banned the community nurse from seeing her and only allowed me and Ann to come into her basement flat, where the patient proceeded to take off all her clothes and run round the kitchen table saying she was a werewolf.
Afterwards Coffey and I discussed a new Mental Health Act being introduced if Labour came to power. She expressed concern about people with personality disorders not being covered by existing legislation and asked what the profession would think about this. I said I thought it would be unwise, as we already had too much coercion, and the conversation rested there. It was, however, clear as early as 1997 that there was a move towards legislation for this group. It was never enacted. Attempts were made to enshrine the DSPD programme in law but all failed. Why?
This is even odder to explain as, only a little further north in Scotland, perhaps still following the advice of their fellow Scot, David Henderson, they solved the legal matter expeditiously. As there was already a Crime and Punishment Hospital Act passed in 1997 (see above), psychiatrists could exercise discretion in regard to a ‘hospital direction’ (i.e. the transfer of personality disordered offenders to hospital from prison); and this was extended further by the devolved Scottish government by simply passing legislation to allow the detention of dangerous prisoners.
Conflict between Psychiatrists and Government
The government in England was in one way trying to be encouraging to the psychiatric profession by introducing the option of treatment programmes that could allow new approaches and ideas to be tested. Yet, by introducing the programme without proper consultation – in the end it was simply bulldozed – it was received very badly. Dr Dilys Jones, at the time medical director at the Special Hospitals Services Authority and clinical strategy director to the High Security Psychiatric Services Commissioning Board, was the main proselytiser of the advantages of the programme for both public protection and therapeutic gain, but she was in a very small minority.
The minister who bore the main brunt of the criticism was Paul Boateng, who was appointed parliamentary under secretary of state at the Department of Health in 1997 and subsequently minister of state at the Home Office and a privy councillor in 1999. He therefore had a foot in both the Home Office and the Department of Health camps and was well placed to defend the new programme. Yet, although he could be quite charming, he had a short temper and did not take kindly to being challenged by psychiatrists.
In my discussions with John Gunn, Emeritus Professor of Psychiatry, Institute of Psychiatry, Psychology and Neuroscience at King’s College London, about these events, he fed back to me the essentials of a forensic faculty meeting in Cardiff where Boateng made it clear that the programme would be going ahead and if ‘you won’t play ball, we’ll get the psychologists to do it’. A similar response was forthcoming at a subsequent debate at the Maudsley Hospital, as by that time the prospects of retreat had disappeared. The DSPD programme would go ahead and if these ‘pesky psychiatrists’ would not see its advantages they could peek in from outside and later take part if they behaved more reasonably.
Straw finally announced the introduction of the DSPD programme in January 1999:
As to the future, my honourable friend the Secretary of State for Health has made it clear that alongside prison for those who are subject to serious personality disorder and to commit offences, and hospital for those who are categorisable under the Mental Health Act, we need a third approach, under which those who are suffering from severe personality disorders and pose a grave risk to the public can be kept in securer conditions as long as they continue to pose that risk.
The programme started at HMP Whitemoor and Broadmoor Hospital in 2001 and subsequently extended to HMP Frankland in County Durham. It was intended to include Rampton Hospital but this was abandoned. The initial cost was £128 million with operational costs amounting to £40 million per annum, and by 2010 it had cost £480 million. Jack Straw and Paul Boateng had their way and the treatment programme was developed and carried out almost entirely by psychologists using esoteric interventions that had no evidence base and whose outcome was not, and never will be, properly evaluated. The prison system still has a block when it comes to evaluation by randomised trials, even though we acknowledge they are difficult to carry out in secure settings. We carried out one but randomisation at times was deliberately overruled by prison staff because of ‘operational requirements’.11
Cost-Effectiveness
One of the key aims of the DSPD programme at its outset was to make the intervention ‘cost-effective’. This was a completely empty aim. The criminal justice system, at least at that time and almost certainly still at present, had no plans to carry out any form of economic evaluation worthy of the term, and the history of previous initiatives included only primitive measures of costs.12 (This should not be tolerated now, and any future experiments of this nature will have to include a proper economic component, preferably carried out completely independently. Criminal justice is far too expensive to ignore its economics.)
Did the DSPD Programme Identify the Really Dangerous?
The government policy of identifying and detaining the ‘really dangerous offenders’ was given a further blow by a systematic review published by Alec Buchanan and Morven Leese in the Lancet in 2001,13 which concluded that ‘six people would have to be detained to prevent one violent act’. So, to prevent such acts, five out of six people would be inappropriately detained. This was a serious matter for human rights.
What Went Wrong?
In the late 1990s, there were no good links between the Royal College of Psychiatrists and the governments of the day and this impaired understanding and inhibited cooperation. Nevertheless, there was a vigorous response by the College coordinated by Mike Shooter (then president) and Tony Zigmond (vice president lead on mental health law) linked to the Mental Health Alliance formed to examine implications of a new Mental Health Act. Louis Appleby, the first national director for mental health (‘mental health tsar’), appointed in 2000, was also involved; but although some in government may have listened, none were moved to intervene.
Vanessa Cameron, former chief executive of the College adds:
I do think the DSPD programme harmed the College’s relationship with governments. With a few exceptions the College was rather amateur in its dealings with ministers. Things got better when during Sheila Hollins’ presidency a Policy Unit, which included parliamentary monitoring, was created and professional staff employed.14
It is also fair to add that the later presidents of the College, Sheila Hollins and Dinesh Bhugra, were more mellifluous than Robert Kendell.
I personally think if there had been a minister of mental health at the time of the DSPD initiative matters might have turned out very differently. I think it very unlikely that such a programme could be introduced again without agreement with the key professionals who should have been intimately involved from the start. When one reflects on battles between governments and the doctors, there are virtually none in which the government has ultimately won. Ken Clarke managed to introduce the internal market to the NHS (see also Chapter 9) and did not give in to the British Medical Association (BMA) over pay, but he suffered greatly in his political standing in the process and probably scuppered his chances of becoming prime minister. The doctors then recovered their earning potential in 2004. In the DSPD programme debate, the doctors won in the end in that the programme was abandoned in favour of a much more modest offender pathway based in prisons. There is still room for compromise here, and how we combine public protection with psychiatric care effectively and humanely remains on the agenda. Until then, the statement by David Henderson at the beginning of this chapter remains just as true today as it was seventy years ago.
Conclusion
It would be wrong to say that the DSPD programme was a complete failure. It was a ridiculously premature experiment but it certainly improved engagement with prisoners, led to a serious review of the therapeutic environments of long-term offenders, which is described comprehensibly and well by Akerman and colleagues,15 and focused attention on a very neglected group, if not always for the best reasons. It also helped to stress the importance of severity in the study of personality disorder, to the degree that a single dimension of severity constitutes the new classification of personality disorder.16
Through dint of careful planning and subtle manoeuvring, in which Alison Hooper (an unsung heroine from the civil service) played a very important part behind the scenes, funding was made available for the development of personality disorder services across England, and these now cover most of the country.17 These developments still only provide a skeletal service in most areas, and many clamour for more, but I doubt whether they would have existed at all but for the DSPD programme. Perhaps if the acronym is regarded in the future as the Development of Services for Personality Disorder it will have achieved its best legacy.
Key Summary Points
Throughout the 1990s, there had been concern in the UK about the number of homicides carried out by people with severe mental health problems. The frequency of homicides was alleged to be increasing but analysis of official data showed the opposite; homicides had been reducing at the rate of 3 per cent per annum over many years.
The Dangerous and Severe Personality Disorder (DSPD) legislation and richly funded ‘treatment’ programme were introduced in the late 1990s by the then Labour government and aimed at the use of contrived psychiatric ‘diagnosis’ and ‘treatment’ to enhance public protection. The exact origin of the concept of DSPD programme remains an enigma but Jack Straw, secretary of state for the Home Office, and his Department played the leading role.
The programme started at HMP Whitemoor and Broadmoor Hospital in 2001 and subsequently extended to HMP Frankland in County Durham. The initial cost was £128 million with operational costs amounting to £40 million per annum, and by 2010 it had cost £480 million in total.
The legislation and ‘treatment’ programme were vigorously opposed by the Mental Health Alliance. The government policy of identifying and detaining the ‘really dangerous offenders’ was given a blow by a systematic review that concluded that, to prevent one significant violent act, five out of six people would have to be inappropriately detained.
Acknowledgements
The preparation of this chapter was a more complex assignment than first envisaged. I am particularly grateful to the politicians Jack Straw, Ken Clarke and Ann Coffey for their time and input and to Alastair Campbell for assisting in contacts. Max Rutherford’s publication Blurring the Boundaries is a very balanced account of the history and context of the DSPD development and I have quoted extensively from this work. John Gunn, Tony Zigmond and Vanessa Cameron contributed valuable additions and corrections to the original draft, and the editors of his book have done so also, with aplomb. I am also thankful to my many colleagues who were involved in our own evaluation of the DSPD programme and gave me additional insights, particularly Deborah Rutter, Conor Duggan, Rick Howard, Barbara Barrett, Eddie Kane and Helen Tyrer. I have also had additional comments from colleagues in the prison service, who wish to remain anonymous, who inform me that the DSPD therapeutic programme is still active; the programme has not gone away.
Introduction
In 1960, offenders with mental disorder were still sometimes treated by general psychiatrists but, more often, they were sent to prison, occasionally to special (high-security) hospitals where, in the 1960s, nursing staff dressed as prison officers. Consultant psychiatrists there were generally as isolated from mainstream psychiatry as their patients, neither specially trained nor recognised as trainers of future specialists. All that has changed.
In 1946, Aubrey Lewis became the first full-time professor of psychiatry at the Maudsley and took the Institute of Psychiatry into the University of London. He appointed first Norwood East, who gave lectures at the Maudsley before the war, and then Trevor Gibbens, returning from five years as a prisoner of war, as senior lecturers in ‘forensic psychiatry’. Why ‘forensic’? It is not what East wrote about – he was just treating criminals,1 but the term has stuck. The East and Hubert report had advocated the development of a specialist psychiatric prison in England (Grendon),2 although when it was finally opened in 1962 it did not, as he suggested, specialise in treating prisoners with psychosis but became a therapeutic community;3 but he had long recognised the need to treat ‘non-sane, non-insane’ prisoners. They abound in every prison system in the world.
In 1960, the Department of Health recognised only two consultants in Britain as forensic psychiatrists: Trevor Gibbens, who became the first UK professor of forensic psychiatry, and Peter Scott, who was allowed to ‘borrow’ two general psychiatry beds at the Maudsley Hospital before acquiring a joint appointment between the Maudsley and Brixton prison, but this gave little scope for effecting prisoner transfers to hospital. Their clinical work was the assessment of juveniles who were before the courts.
The abolition of the death penalty in Britain allowed the proper development of assessment and treatment of offenders. The last executions were in 1964 and the death penalty was abolished even for treason in 1998. Until abolition, it was hard for psychiatrists to remain completely objective in reports for the courts, feeling, almost inevitably, involved in the grisly process of trying to save the lives of condemned individuals. Professor Denis Hill, an expert on epilepsy, assessed Derek Bentley, a young man with epilepsy and intellectual disability, who was hanged in 1953; though involved with a homicide, he did not actually kill anyone. This experience left Professor Hill determined to improve society’s understanding of relationships between mental disorder and crime and to develop forensic psychiatry when he succeeded Sir Aubrey Lewis at the Institute of Psychiatry.
Professional Developments
In 1978, Trevor Gibbens’s chair was established and, in 1988, an independent Department of Forensic Psychiatry was created at the Maudsley. Between 1990 and 2002, seven forensic psychiatry chairs were created around England, almost invariably funded by the NHS; but British universities were becoming business-oriented and their core funding was decreasingly available for developing academic subjects, like forensic psychiatry, which did not attract large grants. The Department of Health set up a Special Hospitals Research Unit in 1970, initially funding a special hospitals’ case register but then, under the Special Hospitals Service Authority (SHSA), more wide-ranging projects and a new chair. As special hospital management was devolved, so the research monies passed into the National Programme on Forensic Mental Health. This both built knowledge and developed young academics across relevant disciplines, but success was rewarded with the removal of the protected streaming in 2007.4 Since then, British academic posts generally have come under increasing threat,5 thus hampering future research developments in psychiatry and, as a smaller specialty, forensic psychiatry is likely to suffer disproportionately.
The vision of specialist clinical development, however, began back in 1963, when the then two recognised forensic psychiatrists and thirteen others met, under the chairmanship of Dr Patrick McGrath, then medical superintendent of Broadmoor Hospital. They resolved to form a forensic subcommittee of the Royal Medico-Psychological Association. After the inauguration of the Royal College of Psychiatrists in 1971 this became a College section, holding its first two-day academic meeting in Birmingham, attended by tens of people. In 1997, it became a College faculty, now with an annual conference attendance of more than 400 people. Training continues, evolving alongside service development, with the three-year higher training curriculum under review at the time of writing.
Liberalising Legal and Institutional Systems
The Mental Health Act 1959, implemented in 1960, placed emphasis on voluntary psychiatric treatment. In 1961, the minister of health, Enoch Powell, launched the ‘care in the community’ policy – with one of his famous melodramatic speeches advocating the closure of hospitals and a drop in bed numbers of around 75,000 within 15 years.6
The care in the community ideal was that most psychiatric work would be done in the outpatient clinic or at home by visiting nurses, with rare need for short-term admissions to small general hospital units. This is probably the best approach if well-resourced and stable families can work with highly skilled staff, quickly available at any moment of crisis. It was hardly a novel idea. Towards the end of the eighteenth century, this is precisely how Mary Lamb was managed after killing her mother while psychotic.7 Few families of people with severe mental disorders, however, have the emotional or social resources to do this and good community clinical care is expensive. Governments have never provided adequate resources nor apparently have understood the extent, complexity and durability of need. Worse, as care gaps opened in England, the then three special hospitals – Broadmoor, Rampton and Moss Side – were increasingly asked to take more patients, ironically because of the liberalising effect of the Mental Health Act 1959.8 By the early 1970s, these hospitals were grossly overcrowded – with patients sleeping in corridors. A fourth was built – Park Lane (later combined with Moss Side, becoming Ashworth).
To some extent, such problems had been foreseen. In the same year as Enoch Powell’s speech, the Emery Report recommended that regional hospital boards should include secure units in the range of local hospital provision – nothing happened.9 In 1974, the Glancy Report recommended the building of a secure hospital unit in each NHS region of England and Wales, with approximately 20 secure beds per million population (about 1,000) – not implemented.10
Matters came to a head when Graham Young, admitted to Broadmoor hospital at the age of fourteen after poisoning several family members and perhaps suffering from autism, was released after nine years there.11 His intense preoccupation with heavy-metal poisons continued, he found employment in a photographic works, with access to thallium, and he poisoned several colleagues. At his second trial, he was found fully responsible for his actions and imprisoned. The home secretary, Reginald Maudling, established two inquiries on the same day – an inquiry into discharge arrangements from special hospitals, to be chaired by Sir Carl Aarvold,12 and a more wide-ranging inquiry into service provision, to be chaired by Lord Butler, a previous home secretary.
The Growth of Mental Health Services for Offenders
The Butler Report included recommendations for caring for and treating offenders with mental disorder.13 The committee, which included Denis Hill, from the Institute of Psychiatry, other psychiatrists, a lawyer and a criminologist, found the overcrowding in the high-secure hospitals so serious that they issued an interim report in 1974, recommending a medium-security hospital unit for every health region, just as Emery and Glancy had done, but with twice the Glancy number of beds. Unlike its predecessors, the Butler Report was not ignored. The secretary of state for health and social services, Barbara Castle, accepted the urgent need and allocated funds for 1,000 medium-security beds. By 1978, some interim units had opened and, by the early 1980s, there was steady growth, although some regions resisted on the advice of their general psychiatrists, even diverting the money to general medical and surgical services. One real problem was training clinicians of all disciplines, especially psychiatrists, quickly enough to staff the units. By 1990, almost all regions had provided purpose-designed units.
The Butler Report is perhaps principally remembered for launching these developments, but it ranged much more widely. Around thirty years before Corston and Bradley,14 it was advocating diversion from the criminal justice system for appropriate cases and calling for explicit care and treatment pathways. Frameworks for coercion and treatment contracts in the community were considered in depth; they expressed the need for research into the effectiveness of ‘psychiatric probation orders’, which applies also to their current counterparts – community sentences with treatment requirements. Indeed, Butler emphasised ‘the need to plan evaluative studies as soon as any new regime or form of treatment has been decided on’. The report also said that ‘the terms “psychopath” and “psychopathic disorder” are unsatisfactory’. These have been removed from disorder classification systems and UK legislation, but they are still used casually and pejoratively. One recommendation belatedly taken up in the Criminal Justice Act 2003 was an indeterminate sentence for public protection (IPP). This proved to be a serious mistake and was repealed in 2012. A Channel 4 documentary, Crime and Punishment, captures the awful legacy of this experiment.15
A key recommendation that has borne fruit was on co-operation between professions. Forensic psychiatry embraced that most systematically under the Multi-Agency Public Protection Arrangements (MAPPA), introduced in the Criminal Justice and Court Services Act 2000 and strengthened under the Criminal Justice Act 2003. The Forensic Psychiatry Faculty of the Royal College provided guidance for clinicians.16
A further wide-ranging review,17 chaired by Dr John Reed, included separate, supplementary reports on academic development, community treatment, finance, hospital provision, learning disability and autism, special service groups (e.g. women, under-eighteen-year-olds), prisons, research, people with special needs, staffing and training and services for people from black and ethnic minority groups. The enunciated principles still hold good:
patients should be cared for [according] to the needs of individuals, as far as possible in the community, rather than institutional settings, under … no greater security than is justified by the degree of danger they present to themselves or others, in such a way as to maximise … chances of … an independent life, as near as possible to their own homes or families if they have them.
Also:
there should be strong proactive equal opportunity policies relating to race and culture in all agencies involved. … ethnic minority communities should be involved in the planning, development and monitoring of services for mentally disordered offenders.
Elements of the review relating to people with mental illness and inpatient provision were generally followed through well. The Special Hospitals Service Authority assumed management of the high-security hospitals from direct Department of Health control between 1989 and 1996, before handover to local Health Trusts; the special hospital population was substantially reduced. The vision of better treatment of offenders with personality disorder was deferred to a new working group but that of reducing numbers of people with mental disorder in prison was not achieved. One recommendation has resonated forward:
services dealing with mentally disordered offenders [should] take account of the needs of victims.
Perhaps inevitably, funding for the development of the new services created resentment among some other psychiatrists. Perhaps uniquely in the history of medicine, one pair called for forensic psychiatry to be abolished:
forensic services, as they currently stand, primarily exist to fulfil political demands for a visible and coercive response to risk. … Meanwhile the poorly adherent, treatment resistant patients … come in and out of general acute wards, frequently abusing and hitting staff on their way … The reluctance of adult general psychiatry to accept low secure cases into this environment is often perceived as obstructive by forensic specialists. … General psychiatrists, in return, see forensic units as awash with resources and spoilt by the luxury of selectivity based on the specious definition of caseness.18
In fact, this outburst reflected old-fashioned attitudes towards mentally disordered offenders, implying that they should be treated in prisons,19 and the problem that general psychiatry is under-resourced.
Prisons
While truly innovative work has occurred in prisons since 1960, the situation for the average prisoner has worsened. Grendon prison was opened as a therapeutic community in 1962, its first governor a senior prison doctor – William Gray. Essential criteria were that men had to volunteer and be violence-free or leave. Grendon was evaluated by the Institute of Psychiatry;20 prisoners were assessed before, during and after treatment. On all the main measures – psychiatric state, symptoms, personality and attitudes to authority figures and to self – large changes were found between the first and final assessments. At baseline, two-thirds of the men had clinically significant psychiatric disorder but just one-third at final assessment; cases of moderate/marked severity dropped from 37 per cent of the total to 18 per cent. Although criminal attitudes also changed substantially, a ten-year follow-up of reoffending was equivocal, but, of course, relevant continuation work had rarely been available to the men.21 Subsequent studies confirmed positive effects.22 That Grendon continues and a second therapeutic community was opened at Dovegate prison in 2001 also indicate success.
Other prison developments were less positive. In 1960, 25,000 people were in UK prisons. By 1972, there were 40,000 in England and Wales, when an Institute of Psychiatry study of their mental health needs found that about one-third were ‘psychiatric cases’.23 A second epidemiological study in 1990 suggested that about 45 per cent of the prison population needed psychiatric treatment, about 1,000 of them as hospital inpatients.24 Later, an Office for National Statistics survey suggested that these figures were underestimates, reporting 7 per cent with psychosis, more than 60 per cent with ‘personality disorder’, 63 per cent with alcohol use problems and 66 per cent with other drug problems.25
By 2020, the prison population in England and Wales was about 83,000 but 40 per cent cuts to prison staff in 2013 in publicly run prisons in England and Wales undid some undoubted previous service improvements.26 Following these cuts, prisoner suicide, self-harm and violence rates rose to the highest levels since recording began in 1978, with 57,968 incidents of self-harm in 2018/19 alone.27 Her Majesty’s Chief Inspector of Prisons (HMCIP), in his annual report of 2016–17, observed:
By February this year we had reached the conclusion that there was not a single establishment that we inspected in England and Wales in which it was safe to hold children and young people.28
Qualitative evaluation of adult prisoner experience suggests that it is similar to the ‘institutionalism’ of the dying asylums.29
What was going well before this false cost-saving exercise? Prison officers had generally moved towards more truly safeguarding and respectful practices, perhaps a halo effect from the Grendon initiative. Indeed, HMCIP found this still true even when the environment was otherwise failing, citing 74 per cent of prisoners asserting they were being treated respectfully.30 Medical services in prisons had changed radically. When the NHS was established in 1948, the prison medical service had remained separate and answerable to the Home Office. Standards of care were poor,31 probably due to its isolation from the mainstream NHS.32 In 2002, it was announced that budgets for health care in public sector prisons would be transferred to the Department of Health, with full commissioning responsibility to be devolved to primary care trusts in stages; this process was completed in 2006. In 2007, HMCIP concerns had shifted:
When mental health in-reach teams rode to the rescue of embattled prison staff they found a scale of need which they had neither foreseen nor planned for.
Four out of five mental health in-reach teams felt that they were unable to respond adequately to the range of need.
… [in prison] need will always remain greater than the capacity, unless mental health and community services outside prison are improved and people appropriately directed to them: before, instead of and after custody.33
The importance of a long-term, comprehensive approach was underscored in guidance published as the Offender Mental Health Care Pathway.34 The Royal College of Psychiatrists set up a Quality Network for Prison Mental Health Services in 2015,35 which many prisons have joined, and set up an ‘enabling environments’ award.
From ‘Dangerousness’ to ‘Risk’
Until 1960, dangerousness was a popular concept in psychiatry. It was the preferred term for the Butler Committee in 1975, and the British Journal of Psychiatry carried Peter Scott’s guidance for psychiatrists on ‘assessing dangerousness in criminals’.36 In the 1970s, criminologists were very interested in dangerousness, and the Howard League sponsored a report on it,37 exposing flaws in attempts until then to measure dangerousness as an individual characteristic. The concept of ‘risk’ became more popular. Psychologists laboured to provide tools to help clinicians, but systematic reviews have pooled data to find their predictive value limited,38 the popular psychopathy checklist (PCL-R) producing the lowest of all as a geographer,39 working on the prevention of road accidents, observed:
Human behaviour will always be unpredictable; it will always be responsive to other human behaviour, including yours.40
Nevertheless, the psychologists’ tools do give prompts, structure and transparency in coming to decisions. Providing that a risk assessment is used ‘as an aid to clinical decision making and not a substitute for it’,41 in conjunction with appropriate risk management and regular re-evaluation, these tools are helpful, although we must remain mindful of advice from a US forensic psychiatrist:
A society sincerely concerned about reducing violence will seek broad measures that address both known risks for violence among persons both with and without mental health problems.42
Miscarriages of Justice
Forensic psychiatry and psychology in England became particularly concerned with false confessions after a 1972 incident in England when an eighteen-year-old with intellectual disability and two young teenagers were wrongly convicted of homicide or arson, largely on confession evidence.43 A subsequent case series of sixty estimated that less than half of suspects have a normal mental state at the time of police interview.44 A Royal Commission on Criminal Procedure followed, leading to the Police and Criminal Evidence Act 1984 (PACE).45 This provided rules for police interviews, with a requirement for the presence of a ‘responsible adult’ in the event of mental illness or disability. Further serious miscarriages of justice followed, however, with a common thread of police under pressure to solve a notorious crime providing flawed evidence. The release of six men wrongly convicted of the Birmingham IRA pub bombings led to the 1993 Royal Commission on Criminal Justice.46 James MacKeith and Gisli Gudjonsson provided clinical and research evidence for added safeguards.47 A new Criminal Cases Review Commission was established.48 Psychological damage to victims of miscarriage of justice adds to the social turmoil and is particularly difficult to treat in the face of constant re-traumatisation as inquiries follow.49 In personal experience of one case alone (PJT), hearings on compensation, inquiries into the miscarriage, criminal cases against lay witnesses and police and further inquiry into why the latter failed lasted nearly thirty years.
Victim-Centred Work
Recognition of the importance of work with victims of harmful behaviours has grown in terms of respect for their wishes and needs and also from the perspective of preventing further harms.
Countless studies have now linked adverse childhood experiences (ACEs) with later violence and/or mental disorder, but Cathy Spatz Widom pioneered prospective study relating to verified abuse.50 The mystery is that about half of such children do not become violent – why? Caspi and Moffitt identified a moderating effect of MAOA-LPR polymorphism;51 in the prospective Dunedin birth cohort study, 85 per cent of boys with a genotype conferring low MAOA levels who had suffered severe maltreatment became antisocial. In England, Walsh and colleagues showed the perhaps comparable vulnerability of people with severe mental illness to being violently attacked,52 not unique to the UK.53
In 1985 Shapland and colleagues highlighted the travesty of treating victims of crime merely as witnesses.54 Victim support services had been set up in the UK, probably the first in Bristol in 1971, but only tiny numbers of victims benefited.55 The Home Office published a Victim’s Charter in 1990, which established the centrality of victims’ rights, and probation services developed expertise in victim support.56 Eventually, the Domestic Violence, Crime and Victims Act 2004 put those rights into law and extended them to victims of offenders with mental disorder. Such victims have the right to know about tribunal hearing dates and to submit written or in-person evidence. For victims of offender-patients on Mental Health Act restriction orders, the system is adequate; but independent victim support is not guaranteed for unrestricted cases.
Over and above a duty of care to victims, we must learn from their experiences. The Crime Survey for England and Wales (formerly the British Crime Survey, now devolved) is a household survey giving a more accurate picture of criminal activity than criminal conviction statistics.57 In psychiatry, we have learned from individual inquiries after homicide. These followed Jayne Zito’s drive to have something of value emerge from her husband’s killing in 1992 by a man with inadequately treated schizophrenia(see also Chapters 23 and 27).58 The Zito Trust closed in 2009, considering its specific goals met; Hundred Families has taken up some of its roles,59 including being a repository for individual inquiries after homicide. Early collective evidence from these confirmed that, even with hindsight advantage, perhaps only 25 per cent of the homicides could have been predicted, but two-thirds might have been prevented with adequate treatment.60 This fits with a growing understanding that when psychosis confers added risk of violence it is when it is untreated.61 Adequate, timely treatment is evidenced on economic grounds too.62
International Exchange
Services for mentally disordered offenders are, in some respects, more culture- and country-bound than other medical specialties. Law and practice and court structures differ even between constituent UK countries. A powerful instrument supporting positive change in the UK, however, has been the European Convention on Human Rights.63 This has underpinned many legislative changes since 1970, including the right in mental health law to appeal against detention even after restrictions on discharge have been imposed by a criminal court.
Many countries have had to reappraise after some service lapses. In England, this has related mainly to high-security hospitals – Rampton and Ashworth both had inquiries after allegations of cruelty to patients and Ashworth again after finding children visiting a personality disorder unit.64 The latter simply excoriated anyone even marginally involved, from the secretary of state on down. Another report on security at all three English hospitals, led by a former director of the prison service, resulted in controversial and high expenditure on extra walls or fences at two of the hospitals.65
As other countries faced problems, British experience was occasionally called in, for example when New Zealand had to respond to over-restrictive and impoverished practices in its then high-security hospital.66 Service development followed on the Butler medium-security model – with relevant cultural modifications, from which we, in turn, now learn. In other areas, forensic psychiatrists themselves have identified service gaps and innovated. Paul Mullen left the UK for Australasia where, in addition to secure inpatient services, he set up specific problem-behaviour clinics for people who provoke avoidance behaviours in many clinicians – including vexatious litigants, the fixated, the morbidly jealous and stalkers.67 This model has recently been brought back to the UK and developed further, for example in a National Stalking Clinic and new gaps met as required and spread further internationally.68
International academic collaborations have been fostered through the International Association of Forensic Mental Health Services from 2000,69 showcasing interdisciplinary research worldwide, while in Europe the Ghent Group, established in 2004, provides support to psychiatrists assessing and treating mentally disordered offenders through an annual meeting discussing services, educational visits and a training programme.70
Conclusion
The period 1960–2010 has generally been one of growth for services for offenders with mental disorder. There have been errors and we are sensitive to ever present risks from both external threats and internal failings that could damage safety, trust and progress.
We have established the first charity dedicated to research in the field – Crime in Mind – .71 The charity finds it difficult to attract funding for the same reasons that forensic psychiatry does not attract funding in universities but it has managed to start a small programme of seminars relating to research issues and even to develop small-scale research projects.
Key Summary Points
By the 1960s, some psychiatrists had begun to specialise in work with mentally disordered offenders but the term ‘forensic psychiatry’ was not used anywhere except at the Maudsley Hospital. In the UK, such work has demonstrated a highly developed capacity for inter-agency working.
In 1978, the first UK professorial chair was established and in 1988 an independent Department of Forensic Psychiatry was created at the Maudsley Hospital. Between 1990 and 2002, seven forensic psychiatry chairs were created around England, almost invariably funded by the NHS; but British universities were becoming business-oriented and their core funding was decreasingly available for developing academic subjects, like forensic psychiatry, which did not attract large grants.
The Butler Report, in 1975,72 included recommendations for caring for and treating offenders with mental disorder. A further wide-ranging review, chaired by Dr John Reed in 1992,73 included separate, supplementary reports on academic development, community treatment, finance, hospital provision, learning disability and autism, special service groups (e.g. women, under-eighteen-year-olds), prisons, research, people with special needs, staffing and training and services for people from black and ethnic minority groups. One problem was training clinicians of all disciplines, especially psychiatrists, quickly enough to staff the units.
In 1960, 25,000 people were in UK prisons. By 1972, there were 40,000 in England and Wales, when a study found that about one-third were ‘psychiatric cases’. By 2020, the prison population in England and Wales was about 83,000 but 40 per cent cuts to prison staff in 2013 undid some undoubted service improvements. Following these cuts, prisoner suicide, self-harm and violence rates rose to the highest levels since recording began in 1978. Qualitative evaluation of adult prisoner experience in 2020 suggests that it is similar to the ‘institutionalism’ of the dying asylums.
Psychological damage to victims of miscarriage of justice adds to the social turmoil and is particularly difficult to treat in the face of constant re-traumatisation as inquiries follow. Forensic psychiatry and psychology in England became concerned with false confessions. In general, recognition of the importance of work with victims of harmful behaviours has grown in terms of respect for their wishes and needs and also from the perspective of preventing further harms.
Introduction
The closure and reprovision of the hospital asylums in the last century led the fundamental transformation of psychiatric services across Europe, North America and Australia. Italy undertook the most radical change, barring admissions to public mental hospitals and replacing inpatient beds with community residential care.1 The second fastest decant was in parts of North America where more attention went to closure than reprovision, with consequences of soaring numbers of mentally ill people in prison and of homeless on the streets of several major cities.2 The British experience fell somewhere between the two, following a more gradual trajectory, doing quite well with reproviding for the asylum population but in trouble from the outset with how to manage the steady accumulation of new cases with multiple and enduring disabilities stuck on acute wards when transfer to the asylum was no longer possible. This chapter recounts some of the journey, focusing on the experience in England and Wales from 1960 to 2010. The major landmarks of this journey are summarised in Box 30.1.
Box 30.1 Major Landmarks in the Evolution of Community Psychiatry, 1960–2010
Launch of asylum closure, 1960–5: Minister of Health Enoch Powell launches plans to replace hospital asylums with 60 beds per 100,000 population located in new district general hospitals (DGHs), with most mental illness managed in the community.3 Encouragement from psychiatrists.4
Reconfiguration and aspirations, 1966–75: Generic social work and ‘sectorisation’ aim at integrated care focused on the same population. Aspirational White Paper Better Services for the Mentally Ill published but stalls in context of NHS reorganisation and political upheaval.5
Expansion of community care but cracks appear, 1976–86: Increased collaborative mental health services in primary care;6 first Community Mental Health Centre (CMHC) opens.7 Concerns that these developments are at the expense of people with severe mental illness. Health and local authority staff in community and residential services reluctant/unable to manage challenging behaviour and ‘new long-stay’ patients accumulate.8 First asylum closes in 1986.
Fear and loathing, 1987–96: Asylum closures accelerate with mostly beneficial outcomes for the resettled patients,9 but increasing criticism by the public, media and politicians of mental health services’ failure to provide adequate supervision for new cases requiring long-term care.10 Introduction of care programme approach aimed at providing better management of risk.11 NHS reorganisation establishes NHS Trusts that are no longer coterminous with local authorities.
Specialisation of community care, 1997–2010: Fears continue. Mental health staff pulled back to secondary care; National Service Framework (NSF) reconfigures Community Mental Health Teams (CMHTs) to provide assertive outreach (AO), early intervention and crisis resolution home treatment teams,12 resulting in considerable service disruption and fragmentation; Mental Health Act revised to include Community Treatment Orders (CTOs). Introduction of IAPT (Improving Access to Psychological Therapies) services increases provision of psychological therapy for common mental disorders.13 World economic crisis in 2008 and the subsequent austerity programme fell heavily on social care.
Closing the Asylum
The impetus for closing the hospital asylum and providing treatment close to where people live came from a combination of optimism, disquiet and financial concerns: optimism among psychiatrists who found that the introduction of social and occupational therapies and the advent of chlorpromazine allowed them to unlock the hospital doors, do away with physical restraint and close long-stay beds, successfully discharging patients to outpatient clinics and day hospitals;14 moral outrage at the conditions in some asylums fuelled by empirical findings that many behavioural problems among incarcerated patients were consequences of institutional life;15 and, finally, the cost of maintaining the old asylums that became difficult to justify as the model of care was increasingly discredited.
In 1961, the minister of health, Enoch Powell, addressed the National Association of Mental Health at its annual conference, in which he included all these themes and called on psychiatrists and wider health and welfare bodies to provide the variety of community services for people whose needs were ‘little short’ of what only a hospital could provide (see also Chapter 1).16 Anticipating his speech, a report estimated that bed requirements could fall by as much as 70,000 by 1975.17 The old asylums would be replaced by a network of district general hospitals (DGHs), each serving a population of around 100,000 with up to 60 beds supported by group homes, day centres and mobile teams, models of which were already emerging around the country. At Warlingham Park, in Surrey, the first community nursing posts were established to support patients discharged from the asylum (see also Chapter 31).18 In Manchester, Maurice Silverman described a district service that prioritised outpatient clinics, domiciliary visiting and day care, relying on just 100 inpatient beds for a population of 254,000. Four out of eight psychiatrists in Manchester, each serving a population of approximately 250,000, said they no longer needed the large mental hospital.19 In 1968, a reorganisation of social services recommended bringing together all providers of personal social care into new social services departments in local authorities and principles of ‘sectorisation’ were introduced in which health and social care focused on the same local population.
Powell had estimated a closure and modernisation process lasting fifteen to twenty years but in fact it all took much longer. A great deal of the delay had to do with the worsening economic situation and industrial unrest through the 1970s and 1980s. Successive governments struggled to cope with strikes by coal miners, ambulance drivers, grave diggers and refuse collectors. Along the way, a reorganisation of the NHS (amusingly described as written in incomprehensible ‘mandarin managerial English’)20 contributed to the loss of senior managerial posts and amplified disquiet among nursing and medical staff (see also Chapter 12).21 Consultants complained that they were being made to do more work with less support; nurses marched in protest over low wages and against private health care; and senior medical staff took medical action, ‘working to rule’ for almost four months. Somewhat surprisingly, amidst this chaos, Barbara Castle, Labour minister of health, published a White Paper, Better Services for the Mentally Ill,22 setting out a vision for future community mental health care. Economic circumstances meant little of this could be realised. Pioneering studies such as those in Manchester proved difficult to replicate, not least because of the paucity of residential and day care capable of managing challenging behaviours (see also Chapter 26). Local authorities struggled with competing priorities, including improving children’s services, while some of the funding allocated to mental health ended up bailing out financial crises in general hospitals. Asylum discharges to that point had largely been of the more able patient, with surveys reporting that several hundred patients identified for discharge remained in hospital.23 Furthermore, as the impetus to close the asylums gathered pace, the option to transfer patients from the acute ward to long-term asylum care was cut off. While it was possible to shorten the length of hospitalisation for acute illness and manage some patients in acute day hospitals,24 no new treatment had prevented the accumulation of people with persistent illness that now comprised up to a third of people in the new DGH psychiatric facilities, stuck there for a year or longer.25
By 1980, asylum reprovision had become the government’s top health priority and pressure was put on regions to close and sell off the old hospital sites as the only way to free up resources to fund new community facilities. The first asylum to close was Banstead Hospital in 1986 and thereafter the quickening pace soon became an end in itself. Most closures followed the same ‘train and place’ approach in which patients practised various aspects of managing life in the community followed by placement in small groups into ordinary houses, accompanied by staff from the asylum who provided supervision at least daily and in some instances up to twenty-four hours. The homes were intended ‘for life’ – then considered a very important reassurance and safeguard. This resettlement process was evaluated in a longitudinal study of the closure of Friern Barnet and Claybury hospitals in north London.26 Although patients showed little change in symptoms or behaviour, most preferred being out of hospital and had significant gains in terms of social and domestic skills, social networks and living conditions. Fears that the move might be associated with higher mortality and homelessness were not realised, although 38 per cent had subsequent readmissions with a third of these having very lengthy hospitalisations. Even the small number of patients with challenging behaviours who were initially transferred to secure accommodation on the edge of the old hospital site did well, many moving on to community group homes.27
Despite these positive results, there were concerns that employing ex-institutional staff to support patients simply perpetuated institutional practices that could only be solved by bringing in a new workforce not contaminated by history, while the notion of providing a ‘home for life’ was soon abandoned. On the other hand, there were ‘not in my backyard’ protests and opposition to resettlement by people anxious about the impact on the values of their properties and of risks to their children. These fears were fuelled by the practice (on grounds of confidentiality but also an attempt to avoid confrontation) of not giving neighbours prior notice before patients were moved to their new homes. An experimental programme showed that openness and preparation of neighbours resulted in greater acceptance and integration but came too late to have much effect on policy.28 Finally, with hospital closures, many of the occupational and sheltered employment schemes provided by the old asylums also ended and were not replaced, leaving many patients idle and lonely.29
By 1993, just over a quarter of the 130 large asylums in England had closed and beds for mental illness had fallen by two-thirds to 50,278.30 Yet pressures on acute inpatient beds continued unabated. Occupancy levels were frequently well above 100 per cent and patients were admitted to private hospitals that had seen the business opportunity and stepped in to plug the gap.
Community Care Takes Off
As outpatient services developed, some psychiatrists started running clinics in primary care or provided a consultation-liaison service to general practitioners. Some mental health professionals, particularly community psychiatric nurses, were seconded or directly employed in primary care.31 Brief psychological therapies for common mental disorders, including counselling and behavioural and cognitive therapies, were increasingly available across professional groups.32 Extending support to primary care was popular with general practice and some models had good empirical support, including reductions in hospital admission.33 The approach also chimed with views that lay behind asylum closure, notably that mental health care would best progress when delivered in non-institutional, non-stigmatising settings by staff not tainted by the institution.
Later controlled trials confirmed the benefit of these approaches in primary care and, in many respects, were the success story of community mental health. In practice, however, they were overtaken by a different model that was shaped by concerns about failures in the management of severe mental illness. Borrowing a model from the United States, the first Community Mental Health Centre was established in south London with a generous grant from the Gatsby Charitable Foundation. Opened in 1978, the Mental Health Advice Centre (MHAC) comprised a multidisciplinary team based in a deliberately non-descript community location. It provided referral and walk-in access for anyone with mental health problems living in the local catchment area.34 The service model was soon replicated elsewhere, with similar centres doubling in number in England every two years and with eighty-one centres open by 1987.35 Yet the approach was not without problems. The walk-in service was swamped by people seeking help for problems of daily life, arguably at the expense of severe mental disorders.36 A survey of the fate of people with severe mental illness, including those in the catchment area of the MHAC, found half continuing to experience severe symptoms and behavioural problems with, paradoxically, the least well-functioning receiving the lowest level of support.37
Concerns from politicians, the press and the public about psychiatry’s apparent inability to manage risk accelerated through the 1990s as people with severe mental illness became much more visible in the community. Managing severe mental illness in the asylum had been relatively easy. Patients were in one geographical location, moved between the ward and on-site or nearby supervised occupational facilities, and institutionalisation was reflected in compliance with treatment and the asylum regime. It proved much more difficult to keep track of vulnerable patients in the community. There was a conspicuous rise in the number of homeless mentally ill people, attributed by some to the asylum closure programme but actually reflecting the revolving door ‘new long-stay’ population, changes to housing benefit regulations introduced by the Thatcher government and a less widely acknowledged closure of several large direct-access hostels in which many people with chronic mental disorders had long-term shelter.38 In 1992, Christopher Clunis, suffering from paranoid schizophrenia and with a long history of repeated admissions, interspersed with poor engagement with outpatient services, stabbed a stranger in the eye, killing him – just one of 39 homicides and 240 suicides by severely mentally ill people in the subsequent 3 years (see also Chapters 23 and 27). A report of a confidential inquiry into these tragedies concluded that many might have been prevented if patients had been adequately supervised. Communication failures, confusion about responsibilities and inadequate use of care plans were all cited as contributory factors.39 The Department of Health issued guidance establishing the ‘care programme approach for people with a mental illness’ in which patients in the community had detailed health and social care plans overseen by a named member of a Community Mental Health Team (CMHT).40
To cope with the demand, CMHTs revised their offer for common mental disorders, limiting access to people already known to the teams or by formal referral from general practice and pulling back staff working in primary care. Some CMHTs split into two sub-teams, one focused on assessment and treatment of common mental disorders and the other taking on the care co-ordination role for severe mental illness. Studies confirmed that patients preferred the less stigmatising CMHT over more traditional outpatient clinics, co-ordination across health and social care was improved and there were reductions in hospitalisation, resulting in lower costs.41 In time, the CMHT model expanded to provide specialist services such as in-reach to hostels for the homeless, with this early work leading ultimately to the DH-funded Homeless Mentally Ill Initiative, which established specialist multidisciplinary teams for homeless people, some of which survive to this day (see also Chapter 26).42
Yet, despite evidence for the benefit of CMHTs, they still seemed unable to do anything to prevent continuing tragedies among a few patients. The DH guidance on care co-ordination was strengthened in 1995 to give the supervising clinician the right to convey people to hospital if necessary. In the meantime, in the United States, one model of co-ordinated care became hugely influential. This ‘Assertive Community Treatment’ (ACT), provided 24-hour support, 7 days per week, ensuring that patients were maintained on medication and received appropriate support for daily living. Community members (family but also police and landlords) were given advice and direction on how to support the individual and, where necessary, an individual was helped to leave unhelpful relationships. A clinical trial comparing this approach to usual care proved ACT to be cost-effective, with patients in the experimental arm spending less time in hospital and with better overall clinical and social functioning.43 Around the same time, in Australia, another controlled study diverting acute patients from hospital to 24-hour crisis and aftercare support by a community team also showed significant reductions in hospitalisation.44 In England, a research team at the Maudsley Hospital attempted to replicate these findings. Patients at the point of an acute admission were randomised to either hospitalisation and routine care or to experimental home-based care with assertive community support. Outcomes over eighteen months were superior in the experimental service, considerably reducing hospital admissions and length of stay, but the positive results were overshadowed by a tragic homicide in the experimental arm and, perhaps for this reason, the study did not achieve the influence it deserved.45 Instead, other studies focused on aspects of the ACT model (the size of team caseload or recruitment of patients outside of acute crisis) and failed to show comparable benefit.46
Alongside these studies, prompted by concerns about whether new community staff had the skills they required for the job, attention was given to training the multidisciplinary team. Most CMHTs included psychologists and other professionals with skills in the delivery of cognitive behavioural therapy (CBT) and other psychological therapies but few of these were developed for the care of severe mental illness. New interventions seemed to offer some hope. These included ‘compliance therapy’, based on motivational interviewing techniques that in studies had achieved improvements in insight and medication adherence; family interventions that reduced relapse; and CBT for psychosis. Drawing on these, a postgraduate training course, the Thorn nurse training initiative, was established in London and Manchester to equip community psychiatric nurses with specific skills in risk assessment, medication management, family intervention and how to support aspects of daily living.47 The principles of the course were taken up in several centres around the UK but, despite some early success, services struggled to maintain these interventions once the supervision and support provided by the training courses were stopped (see also Chapter 19).
The Specialisation of Community Care
In 1998, Frank Dobson, the then health secretary, responded to continuing public concern about dangerous mentally ill people in the community by saying he would introduce new regulations to increase places in secure units and change the law to give mental health professionals new Community Treatment Orders (CTOs) to enforce treatment and ‘sweep the mentally ill off the street’.48 At the same time, and at odds with the idea that mental health teams were not being sufficiently proactive, it was increasingly apparent that there were discrepancies in both the incidence and the treatment response for psychotic disorders between black minority ethnic groups and the indigenous white British population. Not only was incidence considerably higher but people from these backgrounds were more likely to be compulsory hospitalised and to access services through the criminal justice system.49 There were challenges of bias in the diagnostic judgement of psychiatrists and allegations that the high rates of incarceration and coercion reflected institutional or even frank racism (see also Chapter 35).50
In 1999, the DH produced a National Service Framework (NSF) that recommended training psychiatrists in cultural awareness and introduced new specialist teams to better manage risk while reducing reliance on hospitalisation (see also Chapters 10, 23 and 27).51 These new teams included assertive outreach (AO) based on ACT principles, 24-hour crisis resolution and home treatment as an alternative to acute hospital admission and dedicated early intervention services (EIS) for first-episode psychosis. At the time of publication of the NSF, there was scant evidence from UK research for any of these services. The NSF arrived with some force behind it. National groups of experts and champions formed to steer implementation and, at a local level, services went through a protracted and disruptive period of reconfiguration. Not only was there the challenge of identifying staff for the new service but it was also blindingly obvious that some kind of generic CMHT provision would have to persist, perhaps comprising those clinicians who, for whatever reason, had not made the cut for a position in one of the new specialist services.
The new services introduced structural discontinuities in care that were most likely bad for patients. Those with a first episode of psychosis would receive care from the new specialist early intervention team to a maximum of three years before transfer to the CMHT; people who engaged poorly with the CMHT were to be taken over by a specialist AO team but transferred back to the generic CMHT once adherent with treatment; and those in crisis saw different clinicians from those usually involved in their care – all as though the personal relationship developed with a staff member was inconsequential. These services also fuelled an existing trend for psychiatrists to be dedicated to inpatient or community services, radically changing the traditional approach in which patients were under the care of a consultant psychiatrist across both hospital and community. With the greater resource going to managing severe mental illness, CMHTs increasingly offered only time-limited courses of treatment for people with non-psychotic disorders and tried to maintain links with primary care through ‘link workers’ but, in practice, also focused on the most disabled and troubling patients.
Earlier scepticism about the value of ACT in the UK was reinforced by a controlled trial that failed to show AO had any advantage in terms of hospitalisation over that achieved by CMHT care,52 and a systematic review concluded that well-resourced CMHTs persistently matched AO outcomes in the UK.53 Many of the patients that ended up in AO teams had problems with substance abuse in addition to mental ill health. It was hoped that integrating treatments for both disorders within an AO model would be more effective than treatment by separate services but neither this integrated approach nor a much more intensive intervention of combined psychological therapies made any substantial impact on outcomes.54 In contrast, EIS did reduce rehospitalisation and improve clinical and social functioning.55 Ultimately, AO services disappeared from many parts of the country while EIS expanded albeit with concern that resources were being diverted from long-term care. Establishing the Crisis Resolution teams took longer, often starting with the rather easier task of facilitating discharge rather than the intended but much more challenging task of diverting the acute admission itself. Eventually, however, the model did get going and amassed some evidence in the UK.56
By the end of our epoch, the general public were far more accepting of the idea that mental health problems were common, could be spoken about and could be effectively treated. New models for delivering psychosocial help for common mental disorders emerged, notably Improving Access to Psychological Therapies (IAPT),57 and for severe mental illness, new models of occupational support (particularly for paid work; see also Chapter 33)58 as well as more proactive housing support encouraged progress towards independence, albeit with no evidence by way of controlled clinical trials.59
Dobson’s proposals for CTOs eventually found their way into law, though in a less draconian form than originally envisaged. Even before their introduction, international research suggested these approaches had little benefit in terms of reduced rates of rehospitalisation or treatment adherence,60 a view supported by a later UK study.61 The policy also did little to halt a continuing growth in incarceration in forensic and other long-stay secure accommodation.62 Involuntary hospitalisation, originally expected to shrink, instead increased with more rather than less use of locked doors and seclusion.63 Important efforts to counterbalance coercion by greater involvement of patients in their care, including, for example, early experiments with the use of joint crisis care plans to reduce compulsion, peer support and ‘personal recovery’,64 emerged to be further developed in the subsequent decade. In 2008, an international financial crisis originating in the United States put paid to much further development, particularly in social care.
Conclusion
There is little doubt that community care increased the ‘reach’ of psychiatry to bring effective treatments to much larger numbers of people in the wider population, sometimes at the risk of accusations that it has encouraged inappropriate medicalisation of the woes of everyday life. If that is one concern, the opposite is the accusation that psychiatry still relies too much on hospital care. Closing the asylum did not guarantee the elimination of institutional care, which remained in the longer-stay rehabilitation units and group homes that replaced the asylum. If added to residential forensic care and mentally ill people in prison, it has been argued that there are now as many people in some form of incarceration as there were in the old hospitals. Changes are also seen in the use of acute inpatient care where the rates of involuntary admissions have steadily risen since the mid-1980s, possibly due to reductions in acute beds or to changes in tolerance of risk among community teams.65
As noted by some of the earliest commentators, there is very little appetite in health or social care providers to develop to-scale community residential alternatives to hospitals to the extent done in Italy. There have been a few implementations of crisis houses,66 but, typically, these have been for special patient groups not considered at particularly high risk or requiring involuntary care, some of whom would not be hospitalised in any event. Challenging behaviour is still viewed as too risky to be managed in community units, not least because of fears of getting hold of a sufficiently rapid and robust response in an emergency, with the result that, to this day, the model has never caught on as a serious alternative to acute hospitalisation. Similarly, while there are some rehabilitation units that can provide secure care, there is a reluctance to expand provision, as they are viewed as perpetuating institutionalisation. If mental health services should proceed, like in Italy, to radically reduce hospital care, it would need to do this ‘at scale’ with the full backing of authority and increased tolerance of risk. Such a development is yet to emerge.
Key Summary Points
The closure of the old hospital asylums in Britain was driven by psychiatric optimism; moral outrage at overcrowding and poor quality of care; and concerns about the cost of maintaining the old buildings. Initial results were promising, and patients discharged from the asylum experienced a better quality of life with few adverse outcomes. At the same time, mental health care became more multidisciplinary and reached out to people with less disabling conditions.
Problems emerged when the asylums could no longer accept new referrals of people with enduring disability whose needs for care were publicly visible and who were stuck on acute wards. Community residential facilities were unwilling to accept people with challenging behaviours.
The prevailing social model was one of a progressive movement towards independence that spoke against the provision of long-stay accommodation. This left ambulatory mental health teams to provide intensive support that nevertheless failed to prevent tragedies, including suicide and homicide.
The media and politicians claimed community care had failed and demanded more powers to enforce treatment. By the end of the epoch, calls for such draconian measures had ameliorated somewhat but the core dilemma of balancing personal independence with the need for care remained unresolved.
Introduction
The year 2021 marks the sixtieth anniversary of Enoch Powell’s Water Tower speech – a famous or infamous occasion depending upon one’s assessment of deinstitutionalisation and the advent of community care. Powell, the minister of health in Harold Macmillan’s Tory government, was a superb orator and a man not known to mince his words. In 1968, his ‘Rivers of Blood’ speech on immigration would cost him his position on the Opposition front bench and essentially end his political career (see also Chapters 1 and 2). In 1961, however, he was seen as a formidable figure in the Conservative Party and a possible future prime minister. Delivered at the annual conference of the National Association for Mental Health, the Water Tower speech announced a radical shift in mental health policy. Since the passage of the Asylums Act in 1845, which made construction of county lunatic asylums at taxpayer expense compulsory, Britain, like the rest of the Western world, had placed primary emphasis on institutionalisation as the preferred solution to the problems posed by serious mental illness. That era, Powell announced, was coming to a close.1
Neoliberal Dawn
The shift in policy was couched in the apocalyptic tones that Powell preferred. ‘There they stand,’ he intoned, ‘isolated, majestic, imperious, brooded over by the gigantic water-tower and chimney combined, rising unmistakable and daunting out of the countryside – the asylums our forefathers built with such immense solidity to express the notions of their day. Do not for a moment underestimate their powers of resistance to our assault.’ Yet assault them he would. The government’s plans ‘imply nothing less than the elimination of by far the greatest part of this country’s mental hospitals’. It was, he acknowledged, ‘a colossal undertaking’. Within fifteen years, however, half of the existing beds, 75,000, should be gone: ‘if we are to have the courage of our ambitions, we ought to pitch the estimate lower still, as low as we dare, perhaps lower.’ Mistakes might be made, but ‘if we err, it is our duty to err on the side of ruthlessness. For the great majority of these establishments there is no, repeat no, appropriate future use.’
Powell granted that vast sums had been spent on these edifices, and in the past decade much treasure had been expended to make them ‘less inadequate’. Those sunk costs were proffered as one argument against radical change. Other objections could be expected from the ‘hundreds of men and women who have given years, even lifetimes, to the service of a mental hospital or group of hospitals … have laboured devotedly, through years of scarcity and neglect, to render conditions in them more tolerable’. Too bad. The mental hospitals were ‘doomed’; and Powell volunteered to be ‘the first to set the torch to the funeral pyre’. In the following year, the NHS Hospital Plan began the process of enacting these proposals.
Powell spoke like an Old Testament prophet, and a prophet he proved to be. Though the asylums did not begin to vanish from the scene until the 1980s under Margaret Thatcher, their population did shrink significantly throughout the 1960s and 1970s. On an average day in 1960, the population of England’s mental hospitals was just over 140,000. By 1970, the census had fallen to 106,000 and, a decade later, to just over 79,000. Under administrations of all political stripes, Conservative, Labour and Coalition, the remorseless run down of institutional populations has continued apace. When David Cameron took power in 2010, the inpatient population had fallen to less than 23,000; and, while most mental hospitals remained open into the 1980s, notwithstanding the shrinking inpatient population, during the second half of Thatcher’s term in office they were largely abandoned. Some, like the massive Friern Hospital in north London, were converted to upscale flats for the nouveau riche (the building’s past coyly hidden as it became the Princess Park Manor); while others, like the old Devon County Asylum at Exeter, contaminated with asbestos and heavy metals, proved too costly to repurpose and were left to rot. ‘For dust thou art, and into dust shalt return’, as one of Powell’s favourite books would have it.
As Powell’s speech should make clear, deinstitutionalisation was no accident. It was a consciously chosen policy, pursued relentlessly over many decades, even as evidence materialised that the alternative to the hospital – ‘community care’ – was largely a figment of politicians’ imaginations, a phrase that sought to obscure the fact that there was little in the way of community to which most mental patients could return and still less in the way of care. Community care is, as I have suggested elsewhere, a shell game in which there is no pea.2 Those suffering from serious forms of mental illness have been cast into the wilderness – a wilderness that has little time for those with few resources of their own; for people who lack the capacity to function in a neoliberal environment whose architects regard them as little more than a drain on the public purse; and for ‘unfortunate creatures’ chronically dependent on the not-so-tender mercies of a shrinking welfare state, doubly stigmatised for their illness and because they show no signs of reform or recovery.
Psychiatrists have embraced the myth that the mass discharges of patients reflected advances in therapeutics, most especially the psychopharmacological revolution that began in 1954, with the marketing of Largactil (chlorpromazine). That, coincidentally, is the year in which the mental hospital census in England and Wales reached its zenith. The reality, however, is that the number of patients resident in many hospitals had begun to decline several years before antipsychotics arrived on the scene. Leading British psychiatrists such as Sir Aubrey Lewis and Michael Shepherd were rightly sceptical about the relationship between pharmacology and hospital discharges, and a host of later scholarship has confirmed their suspicions (see also Chapter 2).3 Drugs may have soothed professional anxieties when psychiatrists were asked to discharge long-stay patients, and the effects of Thorazine (chlorpromazine) and its copycat drugs on florid symptomatology may have made a difference at the margin, notwithstanding the tendency of disturbed patients to be non-compliant about taking their medications. Most awkwardly, though, for the advocates of the notion of a technological fix as the source of deinstitutionalisation, they have no way of accounting for the pattern of accelerated discharge that manifested itself from the 1970s onwards, a period where no breakthroughs in psychopharmacology materialised.
The record demonstrates that it was policy choices, not drugs, that fundamentally underpinned deinstitutionalisation, whose impetus did not come from the ranks of psychiatry. Indeed, the shift from the hospital to the community occurred largely behind the backs of the profession and independent of its predilections and actions. Political preferences ruled and, by and large, the profession followed along.
Deinstitutionalisation was not a uniquely British phenomenon, of course. Strikingly similar patterns can be observed in the United States and, later, in most advanced industrial societies. The mental hospital, once touted as ‘the most blessed manifestation of true civilization the world can present’,4 was now dismissed as a ‘total Institution’ on a par with such places as prisons and concentration camps, an anti-therapeutic engine of degradation that fomented chronicity rather than cured its inmates.5 That focus on the defects of the institution and its malign effects on those it purported to treat accounted for much of the support the new policy drew from civil libertarians and those concerned with patients’ rights (see also Chapters 3, 4, 13 and 20). Yet it substituted for careful assessment of what alternatives were being prepared, if any, for those discharged back into society at large.
Long before the principle that medical care would be provided free and as a right for all British citizens had been established, the special problems associated with serious mental illness had prompted the state to pay for the confinement and treatment of the overwhelming majority of mental patients. Such care, well into the twentieth century, had come at the price of being labelled a ‘pauper lunatic’, but the costs of housing and providing for the tens of thousands of patients who crowded the wards had long constituted a major draw on the public purse. Nor did that change much with the advent of the NHS in 1948. Mental hospitals continued to exist as a separate system, independent of the health service that dealt with physical ill health. The end of that separation was forecast in the 1962 Hospital Plan but only became a reality during the 1970s. No longer were the mental health services a separate administrative and financial system, and in the fight for resources, the generally low priority placed on mental illness has left the advocates for resources in a parlous position. Worse still, the incurable tendency of the political classes to reorganise and ‘reform’ the health services has repeatedly added to the chaos. Particularly pernicious in this regard was the 1990 National Health and Community Care Act, which passed responsibility for community care on to local authorities. Uneven and inadequate provision has been the inevitable result. No resources were allocated to the local authorities to provide for these new responsibilities, and the dislocations associated with establishment of NHS Trusts then compounded the problem (see also Chapters 10 and 30).
Neoliberal Supremacy
The 1970s saw the breakdown of the post-war consensus in British politics, which had seen both parties embrace a strong role for the government in the economy, an expanded welfare state and a major role for trade unions.6 Though they would be exacerbated by the external shock of the sharp rise in oil prices in 1973, the structural problems that already plagued the economy were exacerbated even further by the increasingly fractious state of labour relations. Unions flexed their power. Massive strikes, both official and unofficial, appeared to render Britain almost ungovernable. The country’s difficulties were made worse by the weakness and fecklessness of the politicians of both parties who ruled Britain during this decade.7 The miners’ strikes of 1972 and 1974, and the resultant blackouts and forced move to a three-day work week, brought the collapse of the Heath government, but Labour under Callaghan proved equally inept and incompetent in the face of industrial turmoil and political unrest. The ‘Winter of Discontent’ of 1978/9 saw more massive strikes, particularly by public sector trade unions, as Callaghan vainly sought to rein in rampant inflation. Bodies went unburied, rubbish uncollected and flying pickets restricted hospitals to taking emergency patients only. Public services appeared to be on the brink of collapse, as did the economy itself.
The sick man of Europe responded by electing a Conservative Party led by Margaret Thatcher in May 1979. Blessed with a thumping majority, her pro-market and neoliberal instincts, and visceral hostility to both unions and the public sector, would dominate British politics for decades. Within two years, she had ejected most of the one-nation Tories from her government and embarked on a radical reconstruction of the British economy and the British state. By the time Tony Blair brought ‘New Labour’ out of the political wilderness and back into power, following more than a decade and a half of Conservative rule, trade unions had been neutered as a political force, economic inequality had widened sharply and the parameters of political discourse and public policy had been altered, if not permanently, then certainly for the foreseeable future. Blair’s ‘Brave New Britain’ in many ways continued to embrace key plans of Thatcherite orthodoxy, albeit while putting a softer, more emollient face on its policies.8
Someone who could announce with a straight face (and meaning it) that ‘there is no such thing as society’, and who proceeded to amplify her meaning by insisting that ‘It is our duty to look after ourselves’, was not inclined to show much support for those who depended upon public provision of services for their very survival. Scornfully, in the same interview Thatcher noted that ‘we have gone through a period when too many children and people have been given to understand “I have a problem, it is the Government’s job to cope with it!” … they are casting their problems on society.’9 It was a view for which she evinced no sympathy. At best, she saw a role for Victorian charity, de haut en bas: ‘There is a living tapestry of men and women and people [sic] and the beauty of that tapestry and the quality of our lives will depend upon how much each of us is prepared to take responsibility for ourselves and each of us prepared to turn round and help by our own efforts those who are unfortunate.’ Victims of misfortune who sought collective, public responses to the difficulties they confronted were out of luck. Hers was not an administration who viewed such supplicants with favour. Handouts were to be in short supply.
In Thatcher’s view, British citizens had become far too dependent on the state, losing their sense of responsibility for their own lives. For her, the key to reviving Britain was to restore economic incentives and the discipline of the marketplace, rolling back the frontiers of the state and reducing expenditure on welfare, confining it to those in ‘real need’. Social security payments steadily eroded in value, and sickness and unemployment benefits were cut. The upshot was a doubling of the relative poverty level by the time she resigned in 1990, when 28 per cent of British children were found to be living below the poverty line (3.3 million, up from 1.7 million when she took office) – statistics that grew even worse under her successor, John Major. Levels of inequality showed no signs of declining under New Labour and have worsened still further since. 10 Neoliberalism, in other words privatisation, the deification of individualism, the destruction of union power, economic liberalisation and increased ideological hostility to the collective provision of public goods became the hallmarks of her tenure in office and have perceptibly changed the terms of political debate ever since. Welfare ‘reform’, in Britain as in the United States, has become a term of art disguising repeated assaults on the social safety net and the demonisation of those dependent upon it.
Neoliberal NHS and Mental Health Services
The sole and singular exception to this sustained ideological attack on the welfare state in the UK has been the NHS. Thatcher ostentatiously chose private health care, but this is one area where her ideology encountered stiff resistance (see also Chapter 9). At least at the level of rhetoric, governments of all stripes since she was forced from office have genuflected to the NHS and promised to protect it, a reflection of its overwhelming popularity among the public at large. Under Labour, the rhetoric was matched for a time with an attempt to boost resources for the health services, though little of this new money found its way into the mental health sector. The promised ‘parity of esteem’ for physical and mental health remained a slogan without substance. The great bulk of the additional money provided to the NHS was directed at physical illness, though administrative obfuscation and the fragmentation of service provision have made quantifying where the money went extraordinarily difficult.11 Moreover, though serious violence among those living with schizophrenia and psychosis is quite rare,12 media-inspired moral panics surrounding this issue have exercised a lopsided influence over public policy and have meant that such increases in resources for mental health provision as did occur under Labour were disproportionately spent on mitigating these risks – a distortion of policy that found legislative recognition in the new category of ‘Dangerously Severe Personality Disorder’ (DSPD) in the 2007 Mental Health Act (see also Chapters 23, 27 and 28). Labour’s decision to have the NHS Trusts mimic the marketplace, a standard feature of neoliberal policy, added additional layers of administration and increased the strain on the system, to no good effect.
Whatever slight progress towards improving the lot of the seriously mentally ill that had accompanied Labour’s thirteen years in power has since been reversed. David Cameron had given notice prior to wining the general election and entering a coalition with the Liberal Democrats in 2010 that ‘the age of irresponsibility was going to be giving way to the age of austerity’. With the enthusiastic support of his chancellor, George Osborne, he was as good as his word. The transfer of welfare to the private and voluntary sectors – a key part of the Thatcherite agenda – was soon under way. Over the ensuing decade, local authorities had their funding from Whitehall cut by 60 per cent. At the same time, caps were introduced on increases in council tax, placing local government under increasing fiscal strain. Under the 1990 legislation, local authorities bore primary responsibility for the community care of the mentally ill. What meagre provision they had previously made for their needs was increasingly threatened. Simultaneously, sharp cuts of the social care budget and the essential abandonment of any pretence to provide social housing worsened the situation further. Nor were these to be temporary measures to cope with the economic shock of the Great Recession. That provided the initial excuse for the cuts, but by 2013 (by which time public spending had already been cut by 14.3 billion pounds compared to 2009–10), Cameron announced that he had no intention of reversing the changes when and if the economy improved. The reduced commitment of the state was to be a permanent feature of Britain’s future.
The NHS was supposedly to be protected from austerity; its funding ‘ring-fenced’. Though this was true in nominal terms particularly as demands increased with the ageing of the population, the health service has suffered drastic cuts in real terms. Cash increases that averaged 1.4 per cent per year adjusted for inflation were entirely inadequate to meet demand. Forced to prioritise day-to-day expenditures, capital budgets were neglected, which led to rapid deterioration of both buildings and equipment. Over 32,000 overnight beds were lost in a decade. Waiting times for services of all sorts lengthened, despite promises to reduce them. And, as usual, in the face of this deteriorating fiscal environment, mental health care suffered disproportionately. The gap between needs and services available took another turn for the worse, and deeper cuts in social services added to the problems faced by those with serious mental illness.
The idea that we bear a collective moral responsibility to provide for the unfortunate – indeed, that one of the marks of a civilised society is its determination to provide as of right certain minimum standards of living for all its citizens – has been steadily eroding since Thatcher came to power. In its place, we have seen the resurgence of an ideology far more congenial and comforting to the privileged: the myth of the benevolent ‘Invisible Hand’ of the marketplace, and its corollary, an unabashed moral individualism. There is little place (and less sympathy) within such a worldview for those who are excluded from the race for material well-being by chronic disabilities and handicaps – whether physical or mental disease, or the more diffuse but cumulatively devastating penalties accruing to those belonging to racial minorities or living in dire poverty.
The punitive sentiments directed against those who must feed from the public trough extend only too easily to embrace those who suffer from the most severe forms of psychiatric misery. Those who seek to protect the long-term mental patient from the opprobrium visited upon the welfare recipient may do so by arguing that the patient is both dependent and sick. But I fear this approach has only a limited chance of success (see also Chapter 27). After all, despite two centuries of propaganda, the public still resists the straightforward equation of mental and physical illness. Moreover, the long-term mental patient in many instances will not get better, and often fails to collaborate with his or her therapist to seek recovery. Such blatant violations of the norms governing access to the sick role in our societies make it unlikely that people with severe and enduring mental ill-health will be extended the courtesies and exemptions accorded to the conventionally sick (see also Chapter 3).13 Instead, even those incapacitated by psychiatric disability all too often find themselves the targets of those who would abolish social programmes because they consider any social dependency immoral.
Conclusion
Seen in this larger context, the neglect that has been the hallmark of the shift from the asylum to community care should come as no surprise. Among those with more noticeable continuing impairment, ex-patients placed with their families seem overall to have fared best. It would be a serious mistake, though, to suppose that even here deinstitutionalisation has proceeded smoothly and has proved unambiguously beneficial. Quite early in the process, John Wing expressed ‘surprise’ that, in view of the greatly increased likelihood of someone with schizophrenia living at home instead of in a hospital, so little research was being done on the problems experienced by their relatives.14 His own work, and that of his associates demonstrated that ‘the burden on relatives and the community was rarely negligible, and in some cases, it was intolerable’ (see also Chapter 2).15 A good deal of the distress and misery continues to remain hidden because of families’ reticence about complaining, a natural tendency, but one which has helped to sustain a false optimism about the effects of the shifts to community treatment. As George Brown pointed out, ‘relatives are not in a strong position to complain – they are not experts, they may be ashamed to talk about their problems and they have come to the conclusion that no help can be offered which will substantially reduce their difficulties’.16 Such conclusions may have a strong factual basis, in view of the widespread inadequacies or even absence of after-care facilities, and the reluctance, often refusal, of the authorities to countenance rehospitalisation. Long delays in receiving appointments, the absence of any provision for respite care, and the lack of co-ordination among service providers compound the problems families face, and eventually many give up the struggle.
Many psychotic patients are thus left to shuffle between flop-houses, homelessness, and short periods in jail, when their illness and dependency cause them to commit what are usually minor offences. Misery and poverty remain their lot, till most of them succumb to an early death. Given the thrust of public policy for the past sixty years, it should come as no surprise to learn that those afflicted with serious mental illness have a life expectancy of between fifteen and twenty-five years less than the rest of us.17 It is, nonetheless, a disgrace.
Key Summary Points
The number of patients resident in many hospitals had begun to decline several years before antipsychotics arrived on the scene.
The population of asylums did shrink significantly throughout the 1960s and 1970s, though mental hospitals did not begin to vanish from the scene until the 1980s under Margaret Thatcher.
Deinstitutionalisation was no accident. It was a consciously chosen neoliberal policy, pursued relentlessly over many decades.
Welfare ‘reform,’ in Britain as in the United States, has become a term of art disguising repeated assaults on the social safety net and the demonisation of those dependent upon it.
‘Community care’ in the era of neoliberal politics has turned out to be an Orwellian euphemism, masking a nightmare existence for all too many of those afflicted with serious psychoses and for their families.

















