Introduction
As institutions, nursing homes have been particularly vulnerable to COVID-19. Although the official reporting has been very problematic, it is estimated that nursing home residents account for a large percentage of all COVID-19-related deaths. In Europe, both Italy and Spain have been badly affected by the pandemic (Comas-Herrera et al., Reference Comas-Herrera, Zalakain, Litwin, Hsu Amy, Lemmon, Henderson and Fernández2020). In these two countries, hundreds of nursing homes are currently under investigation for indirectly causing an alarming number of deaths on their premises. Multiple complaints against the slow reaction of public authorities in providing support to these institutions are now in the hands of the judiciary. What was the policy response to this emergency in these two countries, and how timely and effective was it? How much of what happened can be explained by the existing conditions of long-term care policies (LTC) in such countries, i.e. the policy legacy? In this article we investigate the policy responses to COVID-19 in nursing homes within the overall strategies put in place to tackle the health crisis, focusing in particular on the first wave of the pandemic (from March to June 2020). We analyse the adequacy of the policy measures adopted in nursing homes and the delay in the implementation process. The point of reference for our analysis is the course of action taken in hospitals. In the second half of the article we provide a tentative explanation of such facts based on the policy legacy in this field.
Our empirical analysis focuses on Lombardy and Madrid, the wealthiest regions in Italy and Spain. These two regions were the most severely affected by the pandemic during the first wave, both country-wise and at the European level. We have chosen these two cases in order to reconstruct the emergency dynamics in given policy contexts. Rather than performing a cross-case comparative study for identifying causal effects of high mortality, our goal is to empirically trace complex policy processes within cases in order to depict causal mechanisms, i.e. to understand how the process developed in each actual case (Beach and Pedersen, Reference Beach and Pedersen2019: 16). A detailed analysis of the chronology of events allows us to study the evolution of the policies implemented and the limitations faced in the nursing homes sector in each region and to inductively build a valid, but not necessarily generalisable, theoretical explanation.
Our findings suggest that nursing homes in Italy and Spain were trapped in a blind spot, being only marginally considered in the emergency action plans. During the first wave of the COVID-19 pandemic, policy response was late and weak, especially when compared against actions in the National Health Systems. We argue that this is associated to policy legacy factors: in particular, the marginal role of nursing homes in the two countries and regions studied.
The article is structured as follows. Section two presents the main theoretical concepts used in the article and the methodological strategy adopted. Section three briefly describes the evolution of the pandemic in our two countries and regions. Section four offers a rich account of the public policy response to COVID-19 in nursing homes, looking specifically at the main policy mechanisms that were used to deal with the crisis. Section five tentatively proposes the principal explanatory factors for the type of policy response in nursing homes identified in the preceding section. Section six concludes.
Concepts and methods
Conceptual framework
The COVID-19 emergency was an acute exogenous shock for health and social policies across the whole of Europe. Public authorities had to manage the emergency in a situation of severe uncertainty and total lack of knowledge about the disease, its diffusion and its impact. The causes were unclear, while the problems and responses, from a policy standpoint, were only vaguely understood. The high number of deaths in care homes during the first wave of the pandemic shows that such policy responses were ineffective, due to a complex range of multiple factors.
To analyse the (weak) capacity of policies to manage the emergency in care homes, we adopt a relatively simple policy analysis scheme (see Figure 1). Since the onset of the outbreak, policies have had to deal with a new risk, and authorities have had to activate a range of policy tools to protect people and prevent the spread of the virus. In the first wave, three main policy tools were crucial in protecting care homes: lockdown measures; testing and tracing plans; and provision of Personal Protective Equipment (PPE) to protect residents and staff. A further fourth policy element was to control the flow of patients from/to hospitals. These policy tools were activated by introducing new public regulations, mobilising actors and financial resources, and providing coordination among institutions. In short, by implementing a complex policy mechanism. We reconstructed these mechanisms and observed the policy outputs through chronological sequence analysis and process tracing.

Figure 1. Cause, mechanisms and outcomes of the COVID-19 crisis in nursing homes
Source. Own elaboration
As an explanatory framework, and to advance potential causal mechanisms linking cause and outcome, we tentatively look at structural and cognitive factors that reveal policy legacy effects (Pierson, Reference Pierson1993; Kingdon, Reference Kingdon1995). Building on historical institutionalism, we understand policy legacy as a historically constructed set of institutional constraints and cognitive frames that structure the policy-making process (Steinmo et al., Reference Steinmo, Thelen and Longstreth1992; Immergut, Reference Immergut1998). In cases of unpreparedness and lack of previous experience, it is expected that policy responses will be strongly influenced by the most relevant characteristics of the existing governmental system (Capano et al., Reference Capano, Howlett, Jarvis, Ramesh and Goyal2020). Moreover, problems and solutions are defined on the basis of the dominant cognitive frames that designate the main priorities and policy goals. Institutional settings as well as policy ideas therefore play a crucial role in framing new policy actions, especially in situations where decisions need to be taken very quickly with no past experience.
In the case of nursing homes, policy legacy is seen as hindering an appropriate response to the crisis. Although we are well aware that the outputs we describe are conditioned by a vast array of factors, many of which are context and time-specific, we are interested in unveiling the possible significance of institutional features and the interaction of actors in a given model of policymaking in explaining the specific management of the COVID-19 crisis in nursing homes. Thus, following Howlett (Reference Howlett2009: 243), we mainly focus on the meso-level of policy regime logics, situated between overall structural issues and the more micro-level of policy actor behaviour.
Exploring the role of policy legacy in shaping emergency strategy for nursing homes, we consider three main aspects (see Section 5): i) the public relevance of nursing homes within the LTC system in the two countries; ii) the degree of public provision and funding of residential services; iii) the main characteristics of the governance system of nursing homes, considering the regulation and the coordination capacity of central government in this policy field. The first aspect captures the cognitive relevance attributed to nursing homes within national welfare systems and the status recognised in LTC policy reforms and public discussion (Béland, Reference Béland2010, Reference Béland2016). The second and third aspects reflect the idea that historically-constructed institutions and governance settings create major constraints and opportunities that affect the policy-making process (Skocpol, Reference Skocpol1992; Hall and Taylor, Reference Hall and Taylor1996; Immergut, Reference Immergut1998).
Methodology
Our empirical analysis is based on a combination of chronological sequence analysis and of process tracing. The chronological sequence analysis does not merely have a descriptive function (how and when events happened and decisions were taken), but is also an important analytical tool, since a sequence of a cause and its effect cannot be temporally inverted (Yin, Reference Yin2018: 184-185). We compare the chronology of policy decisions that affect nursing homes against broader policy responses related to the health crisis. By using this comparison, we are able to evaluate delays in actions and issues regarding levels of resources and coordination. Our results are drawn from extensive documentary research of material coming from media outlets and official reports (see Appendix 1).
In order to establish the chronological sequence of the main events that characterised the nursing home strategy during the first wave of the pandemic, we have organised the data by weeks. We begin in week zero with the first reported local transmission of a COVID-19 case in each country: 22 February 2020 for Italy and 25 February 2020 for Spain, according to the European Centre for Disease and Control tracker (ECDC, 2021). The end point for our analysis is situated around week eight, when both countries started their slow descent from a peak of cases at 221,124 for Spain and 207,428 for Italy.
In parallel to the chronology, we have also used process tracing in an exploratory way to detect what policy mechanisms link the emergence of the pandemic in its different stages (the cause) with public policy responses at different levels of government (the output) (see Figure 1). Building on our previous discussion, we group these policy mechanisms into lockdown, testing, sourcing equipment and discharging/hospitalisation. Through a rich description of events, our study proposes a framework for potential causal relationships. Following Beach and Pedersen (Reference Beach and Pedersen2019: 33) we depict our methods as an empirical narrative, where the actual causal mechanisms between policy legacies and the outcomes of different policy tools remain to be explored in further research.
Evolution of the pandemic in Lombardy (Italy) and Madrid (Spain)
In Figure 2 we present the evolution of new daily cases and deaths, in a five-day moving average. In both countries, the number of cases began to increase sharply around the end of February, with the evolution in Spain occurring approximately a week after the evolution in Italy. On 22 February, Italy reported its first local transmission of a COVID-19 case, while in Spain this happened on 25 February. When the World Health Organization (WHO) declared COVID-19 a ‘high global risk’ on 28 February, Italy already officially had 888 infected people, 345 hospitalised COVID-19 patients, sixty-four patients in intensive care and twenty-one deaths. Likewise, when the WHO declared COVID-19 a ‘global pandemic’ on 11 March, there were already over 2,000 cases and forty-seven deaths in Spain. From then on, cases (and deaths) increased sharply in an exponential progression until they reached their peaks (both in cases and deaths) in late March/early April. Only from 3 April was a slow, gradual decrease in cases and deaths observed, going down to around 300 daily cases at the beginning of June.
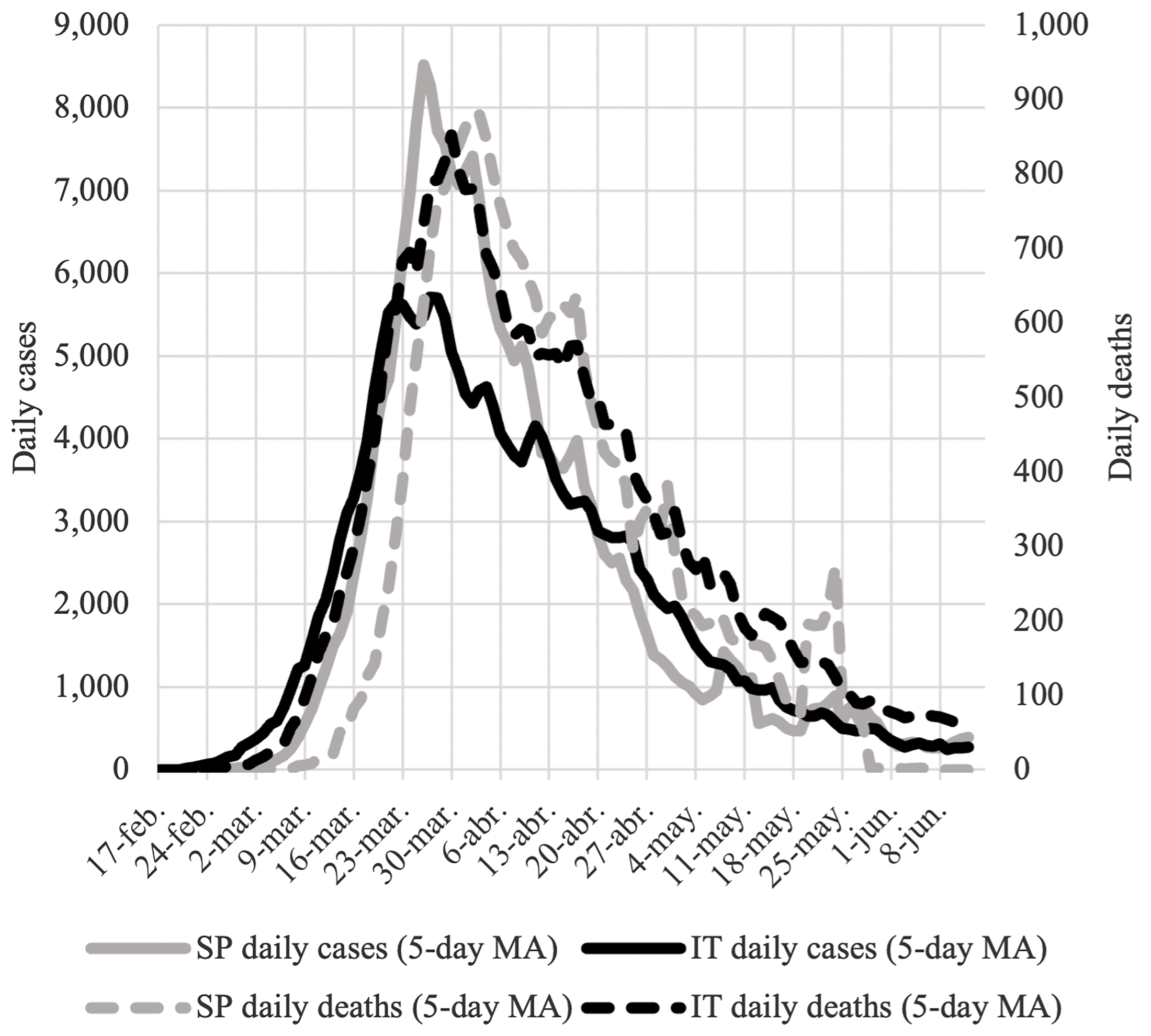
Figure 2. Daily reported cases and deaths in Italy and Spain
Source. Own elaboration using ECDC (2021) data. Note: daily reported cases with negative values have not been included.
Given the differences in counting methodologies, using excess deaths – measured as the deviation of the number of deaths during the period of the pandemic compared to deaths for the same period in previous years – can give an accurate idea of how both the regions studied in this article were more severely affected than other EU regions (ONS, 2020). From 21 February to 12 June, the highest Covid-19 related deaths in Europe was in Northern Italy and in Central Spain, with the province of Bergamo, in the Lombardy region, reaching an 848 per cent age-standardised mortality rate around 23 March and the Madrid region reaching 433 per cent the following week. No other regions in Europe reached this degree of mortality. The next most affected regions in Europe were in the UK and France (mainly near London and Paris), but they never reached peaks above 300 per cent.
How much is the mortality rate due to COVID-19 in nursing homes in Lombardy and Madrid? The answer to this question is not at all straightforward. In both countries, lack of testing and problems with reporting mean that the figures are either incomplete or not comparable across countries − or even within regions in one country. For Italy, the only data available is provided by the Italian National Institute of Health (Istituto Superiore di Sanità) survey. This covers 1,356 nursing homes for elderly people with dementia (i.e. representing only a subsample of a total of 4,629 residential institutions in the country). As for Spain, to date, we do not have official figures on the number of confirmed deaths in nursing homes. This is despite the fact that on 3 April, the Spanish Health Ministry requested regional governments to provide this information in a standardised way. Taking these limitations into account, Comas-Herrera et al. (Reference Comas-Herrera, Zalakain, Litwin, Hsu Amy, Lemmon, Henderson and Fernández2020) have estimated that deaths attributed to COVID-19 as a percentage of all nursing home residents are 6.10 per cent in Spain and 3.10 per cent for Italy. This ranks our two countries alongside other countries with high rates such as the UK (5.3 per cent), Belgium (4.9 per cent) and Ireland (3.2 per cent).
Policy response to COVID-19 outbreaks in nursing homes
Here we present the chronological description of the nursing home policy strategy implemented to manage the COVID-19 crisis in both regions. In order to provide a better understanding of the response capacity in nursing homes, the two country graphs in Appendix 2 provide a visual representation of the sequence of events, also comparing the nursing home sector with the hospital system regarding the timing of their main actions. The lack of timeliness (expressed in days of delay) of the response in nursing home clearly identifies a particular critical configuration in this policy field regarding the capacity to respond to the COVID-19 emergency. In this section we will reconstruct the policy strategy adopted and its main failures more in depth, focusing in particular on the three main policy tools identified in Section 2 (see also Figure 1).
Lockdown: nursing homes in a blind spot
During week zero the Italian Health Ministry promptly activated prevention protocols in hospitals. Visits to patients were discontinued. Anyone with symptoms or that had come into contact with a COVID-19 patient was tested and then monitored for fourteen days. All confirmed COVID-19 cases were hospitalised in isolation rooms. Healthcare staff working in hospitals and in contact with COVID-19 patients were required to wear appropriate PPE. In parallel, all public and private events were suspended in Lombardy. The region quickly moved into lockdown, including the closure of schools and strict mobility restrictions. However, such emergency protocols were not immediately adopted in nursing homes. Restrictive rules about external visitors in nursing homes were only partially implemented during week one and at the discretion of managers. In week two, when a general lockdown of the country began, nursing homes were still allowed to admit a limited number of visits.
In Spain, the first political actions to combat the health crisis were concentrated at the regional level in Madrid, the epicentre of the pandemic. But it was not until week one that specific action was taken regarding nursing homes. The central government issued a protocol regarding hygienic and protection measures for workers, while the regional government delivered a protocol on how to isolate infected users and ordered the closure of recreational centres for retired people if a cluster of COVID-19 cases was detected, but not of nursing homes. However, over the same week the regional government changed its approach and restricted family visits to nursing homes.
The pandemic crisis then began to accelerate frenetically. Consequently the regional government introduced specific lockdown measures for health care services: all non-essential health appointments were suspended. Community health care centres also closed and moved online. The only specific mention of nursing homes was about health measures and the need to start using telemedicine. Complete isolation of nursing homes was not mandated until the end of week two, when the country had already 2,000 confirmed cases and forty-seven deaths, with around 50 per cent of these cases in the Madrid region.
Testing and reporting of cases
At the onset of the pandemic in Italy, testing was required for all people with symptoms, i.e. including nursing home patients. But in reality, testing was to a large extent concentrated only in hospitals. In Lombardy, only hospitalised patients and people with respiratory symptoms and in urgent need of hospitalisation could be tested. As a consequence, there was no way to test nursing home patients and workers. In this way, COVID-19 became a hidden phenomenon in nursing homes, although it was actually spreading inside them very quickly.
Data on Lombardy show that in week four, only 2 per cent of the official COVID-19 infections were in nursing homes. But according to a national retrospective survey carried out by the Italian National Institute for Public Health (ISS), the majority of COVID-19 deaths in nursing homes (including deaths of people with similar symptoms but who had not officially been tested) actually occurred during week three and four.
According to the first reports that expose the reality in nursing homes, only during week four did the Italian government add healthcare staff working in nursing homes to those who should have priority testing. A week later (week five), the shockingly high number of deaths in nursing homes entered the public debate. Pressed by these events, the Italian Minister of Health then enforced the testing of nursing home patients and asymptomatic workers: the result was a vast increase in the recorded numbers of cases. Official statistics in Lombardy registered that in one week, the share of tested COVID-19 infections in nursing homes scaled up to 40 per cent of the total.
Likewise, at the beginning of the outbreak, testing in Spain was only available for suspected patients with respiratory symptoms and previous links with Wuhan (China). Although this theoretically also included nursing homes, in week three health officials from both the regional and central governments claimed that they had logistical problems in providing the required testing. As the press started to report on the situation in nursing home, their residents were made a priority for testing (although again, only those with symptoms).
In an attempt to resolve the ‘diagnosis blindness’ problem, in week four the Spanish central government distributed quick tests to regions for health workers and residents of nursing homes. However, the Madrid regional government prioritised distributing these tests to hospitals. It was only when for the first time (during week six) the regional government carried out a first comprehensive report regarding COVID-19 deaths in nursing homes (according to which more than 70 per cent of death recorded between week one and six had been suspected cases), that quick tests finally arrived in nursing homes. The figures kept increasing until week eight, when they stabilised at around 5,900 deaths in nursing homes, of which 1,200 were confirmed cases and 4,700 suspected cases. This figure represented 12.5 per cent of nursing home beds and around 65 per cent of all COVID-19 deaths in the region.
Human and material resources to combat COVID-19
In order to fight the COVID-19 emergency, in week one the Italian government immediately adopted an extraordinary plan to support the hospital sector. This aimed to hire more health care workers, finance the purchase of equipment, increase the number of intensive care beds and involve private hospitals in the provision of health care services. But again, there was no specific mention of nursing homes.
Indeed, it was only some weeks after the onset of the outbreak that nursing homes became the target of specific policies. In week four, guidelines provided by the Ministry of Health indicated the importance of ‘intensifying’ the staff in these facilities, also through the implementation of the extraordinary recruitment plan already in place for hospitals. However, there is no evidence that this plan was ever executed. At the regional level, the Lombardy government issued a resolution to provide nursing homes with a specific COVID-19 plan, but only in week five. The same structural delay plagued the national strategy: indeed, it was only during week eight that the Italian Health Ministry published its first specific guidelines for prevention and control strategies in nursing homes.
In Spain, protocols for nursing homes were implemented earlier than in Italy, and we find more specific measures aimed at nursing homes; however, the contrast with measures carried out in hospitals is vast. The first emergency funding to support the health-care system was approved by the Health Ministry in week two. As in Italy, efforts were placed on rapidly increasing the number of hospital beds. In Madrid, in week two the regional government announced the creation of a 5,000-bed COVID-19 hospital that was ready within a week. That same week, the Spanish government authorised the urgent recruitment of 1,700 health professionals in Madrid. Special funding from the central government to the regions was also approved in week three to support socio-sanitary services, but only about 20 per cent of this funding went to nursing homes. The recruitment of health professionals was also difficult due to the better pay conditions in hospitals. To compensate for the scarcity of staff in nursing homes, the Madrid social services department called for volunteers.
In both countries, the lack of protective equipment (PPE) for staff was a key difficulty in fighting infections in nursing homes. During the critical weeks of the outbreak, the scarcity of PPE meant that priority was given to professionals working in hospitals, at the expense of nursing homes.
In Lombardy, while already in week zero a general regional protocol established the use of PPE for all healthcare service providers, there was much confusion about whose responsibility it was to provide it. Only in week four did a Health Ministry circular establish rules to guarantee a minimum supply to protect nursing home workers. However, during the whole of April a lack of PPE continued to be persistently reported by nursing home managers. According to the aforementioned ISS survey, by mid-April (week seven), over 86 per cent of nursing homes declared that the lack of PPE was a major difficulty.
In Madrid, the lack of PPE was so dramatic in nursing homes that Civil Protection teams, together with the special emergency unit of the Army, were given the special mission of disinfecting nursing homes and providing sufficient equipment. Nevertheless, during week three nursing homes were still complaining about the public authorities’ poor response regarding the provision of material. The care sector trade union CSIT even reported managers to labour inspection for not providing protective equipment to staff, but just as in Lombardy, the chain of responsibilities was a puzzle that was too complex to solve quickly.
Discharged patients and limits on hospitalisations: trapped in nursing homes
The critical condition that nursing homes found themselves in during the COVID-19 crisis was further exacerbated by decisions regarding the discharge of hospitalised patients to nursing homes, coupled with the introduction of specific limits as far as the hospitalisation of sick nursing home residents is concerned. In the two regions studied here, pressure on hospitals became very severe during the peak of the pandemic. As already described, the health authorities focused on increasing the capacity of emergency units in hospitals, and this also meant making decisions about where to find additional intensive care beds.
In this attempt to locate beds outside hospitals, in week two the regional government in Lombardy introduced the possibility of discharging hospital patients (including those affected by COVID-19 but not in a critical condition) to nursing homes, while guaranteeing specific standards in terms of protocols and isolation. Nursing homes were not obliged to accept these patients, but several of them – in particular, nursing homes with higher health care standards – agreed to do so. This was also because the regional government was only allowing 50 per cent of new admissions for nursing homes. A generous budget (150 Euros/day) was also provided by the region as reimbursement for each patient accepted from hospitals.
Furthermore, a second critical aspect was the severe limitation imposed on hospitalising nursing homes patients. Our two regions followed different criteria. In Lombardy, according to a regional resolution established in week five, the hospitalisation of older patients (those over seventy-five) who suffered conditions of frailty or comorbidity was not allowed, leaving them in the hands of care homes. Only patients who were over seventy-five, in ‘fair health’ but with abnormal oxygen saturation values could be sent to hospitals. While the public authorities claimed that this decision was to avoid further risks of extremely vulnerable patients deteriorating, in reality this measure denied proper medical care to many residents in nursing homes.
The criteria used to avoid transferring nursing home residents to hospitals in Madrid became a highly contentious political issue. The final version of the protocol established in weeks three-four by the regional government for regulating hospital admissions called for a specific assessment based on the Rockwood fragility index used in gerontology. Although this protocol was challenged by the regional social services department and the largest Spanish disability organisation (CERMI), which claimed that the assessment was denying hospitalisation to people with physical and mental disabilities, the index continued to be applied during the critical weeks when there was a risk of hospital overcrowding. This enforced a strict selective admission of nursing home residents to hospitals.
The rising death toll in nursing homes and no possibility of transferring residents to hospitals made it crucial to medicalise nursing homes in Madrid. The regional government published guidelines in week four that included a transfer of competencies for nursing homes from social services to health. In this new arrangement, interventions to medicalise care homes were to be carried out by the department of health upon the request of social services. However, increasing nursing home capacity and creating new centres, a costly and complicated task, was left to social services, quite clearly indicating the reluctance of the department of health to deal with nursing homes. Transfers between nursing homes continued to generate further risks. It became increasingly clear that neither health services in hospitals nor in primary health centres were being assigned adequate resources to deal with the medicalisation of nursing homes.
Long-term care in Italy and Spain: the role of policy legacies
In the previous section we showed how nursing homes were not the target of any specific measures in either country during the first critical weeks of the outbreak. This delay was compounded by the inadequate implementation of preventive and protective measures, far inferior to those implemented in hospitals. We argue in this section that the inadequacy of the policy response to help nursing homes during the COVID-19 crisis can, at least partially, be explained by structural and cognitive factors that reveal policy legacy effects. Policy legacies in this context are seen as hindering appropriate responses during the different phases in the evolution of the pandemic (Capano et al., Reference Capano, Howlett, Jarvis, Ramesh and Goyal2020).
In this section, we group these policy legacy factors into three main categories as already explained in Section 2 (see also Table 1). Such analysis is necessarily carried out at national level, as comparative data and information are available only at this scale. Particular deviations from the national pattern will be properly indicated. Firstly, we look at the relevance of nursing homes within the two national LTC systems, as shown by the reforms and policy innovations recently introduced or proposed in the field. Secondly, we consider coverage rates and public funding in nursing homes compared to that of other EU countries. Finally, we consider governance aspects, including both regulatory and coordination capacities.
Table 1 Policy legacy dimensions considered in the paper

Source. Own elaboration.
Public relevance of nursing homes within the LTC system
Historically the LTC system has been poorly embedded within both the Italian and Spanish welfare states. Strong familialism led to a very residual supply of publicly funded (both home-based and residential) care services for frail elderly people. Since the early 2000s, in both countries, demographic ageing, the mass incorporation of women in the labour market and international migration flows have led to the growth of a private, little-regulated care market fuelled by in-house care provided by migrant workers (Bettio et al., Reference Bettio, Simonazzi and Villa2006). The financial convenience of this ‘migrant-in-the-family regime’ has sustained a strong preference for ‘ageing in place’ strategies in the population as well as among policy makers.
From this starting point, our two countries have recently taken divergent policy trajectories. Spain made significant policy innovations and financial investments in this field in 2006 through the LTC Act (Ley de Dependencia), which formally universalised access to care provision by recognising it as a right for accredited dependants. However, research has shown that the implementation of such reform has been severely hampered by a range of factors including the financial crisis in 2008, a critical devolution of responsibility to regional governments, and insufficient public funding (León and Pavolini, Reference León and Pavolini2014). Furthermore, the LTC Act did not address the structural deficiencies of nursing homes nor their modernisation and, despite the increasing health needs of residents, it kept regional social service departments as the main competent bodies.
Conversely, Italy has been characterised by prolonged institutional inertia, with very limited policy reform over recent decades (Costa, Reference Costa, Ranci and Pavolini2013; León and Pavolini, Reference León and Pavolini2014; Estévez-Abe and Naldini, Reference Estévez-Abe and Naldini2016; Saraceno, Reference Saraceno2016). In the last two decades, LTC funding has been strongly directed towards cash benefits, while proposals for general reform (Pavolini et al., Reference Pavolini, Ranci, Lamura and Greve2017) or policy innovation (Ranci and Arlotti, Reference Ranci and Arlotti2019) have never considered residential services as a priority. More recently, a document of a National Commission in charge for a general LTC reform (Commissione per la Riforma della Assistenza Sanitaria e Sociosanitaria della Popolazione Anziana, 2021: 7) has not only affirmed precedence for home-based care arrangements, but it has also considered residential institutions as ‘only temporary solutions aimed to stabilise the health conditions of patients’, to be replaced by home care arrangements as soon as possible. No nation-wide regulatory proposals concerning LTC have either prioritised or even named residential care as a policy priority, in spite of the very poor institutionalisation of such field.
In spite of different trajectories in LTC policy, in both the countries nursing homes have not been recognised as important assets of the national LTC system, and have not been targeted for increased national funding or stronger regulatory settings. On the contrary, in both countries institutional innovation has always prioritised home care services or cash-for-care measures, leaving residential services in a permanently marginal position.
Public provision and funding of residential services
Public expenditures in residential services have recently taken different trajectories in Italy and Spain. Building on the 2006 reform, Spain has focused on expanding its nursing home structures and has built more facilities, especially up until 2010, slightly increasing overall coverage and the percentage of publicly-owned beds. The coverage rate (number of beds/population over sixty-five) has increased from 1.9 per cent in 2004 to 4.7 per cent in 2011, and has been consolidated to 4.4 per cent in 2018 (OECD, 2021). Italy has maintained coverage at a pretty stable level in the last decades: it was 1.5 per cent in 2004 and it is 1.9 per cent in 2018 (OECD, 2021). As shown in Table 2, in 2018 both countries scored in lower position in respect of other European countries.
Table 2 Coverage rates and public financing of nursing homes in a selected group of European countries, 2018

Source. OECD (2021).
These figures are also in line with spending patterns: in 2018, public financing in inpatients LTC facilities was 172 PPS dollars per capita in Spain and 143 PPS dollar in Italy, with an increase in the last eight years of 17 per cent for Italy and 30 per cent for Spain (OECD, 2021). In spite of these recent developments, our two countries lag behind most other European countries. In 2018, PPS per capita expenditure in residential facilities was 60 per cent higher in Austria and UK, almost double in Germany and even higher in France, Belgium, the Netherlands and Nordic countries, than in our two countries (see Table 2). Only in Greece was spending lower than in Italy and Spain, confirming a pattern (with the exception of Finland) which Southern European countries seem to share (see Table 2).
Notwithstanding recent divergent institutional trajectories in LTC policies, therefore, Italy and Spain share a weak level of investment on nursing homes. Public financial investment in these services and coverage rates are still at the lowest levels in Europe, and this lack of commitment on the side of the State badly impacts on the funding, extension and quality of such services. In both countries limited public funding does not cover the full costs, and this implies that older people in need for residential care have to pay huge amounts of money to use these services. In both countries, therefore, residential care is still a residual welfare provision, hardly affordable for most of the severely impaired older population.
Governance
The governance structure of the sector plays a crucial role in emergency policy making, as it frames the capacity of government to enforce rules and implement its guidelines. Moreover, governance is crucial for guaranteeing equal entitlements and provision in highly pluralised, decentralised systems such as the nursing homes sector.
In both countries, the regulation of nursing homes has been decentralised to regions and has long suffered serious fragmentation of subjects and actors. The Spanish Act of 2006 establishes some minimal requirements, but leaves implementation and monitoring to sub-national administrations. While other decentralised realms of the welfare state (namely, health and education) possess robust territorial coordination mechanisms, the marginality of the LTC sector translates this decentralised element into an almost chronic institutional fragmentation with insufficient channels of communication between the different levels of the administration. In Italy, nursing homes are mainly governed at regional levels with no national coordination or standards.
A particularly important element is the lack of integration between social care and health. In both countries, residential institutions are formally considered integrated socio-sanitary services. However, in practice, the health element is clearly downplayed, leaving these institutions in a sort of institutional vacuum (Arlotti and Aguilar-Hendrickson, Reference Arlotti and Aguilar-Hendrickson2018; Marbán Gallego, Reference Marbán Gallego2019). In Italy, the National Health Service does not clearly recognise the specific health services provided by residential institutions, limiting itself to paying an all-inclusive daily fee for each resident (officially amounting to 50 per cent of the total costs for each patient). The result is that health services in nursing homes are not provided on the basis of a general, recognised social right. The consequence is that not only do the vast majority of residents have to pay these expenses themselves, but also that nursing homes have had to raise their fees to match their costs, or cut their costs by reducing numbers of qualified staff and lowering quality standards. The COVID-19 emergency found many of these institutions in an already critical situation.
One good example of the coordination challenges that have been explained in the previous section is the decision of the Madrid regional government to transfer responsibility for nursing homes from social services to health. Whereas the health care system became centralised under the State of Alarm and the Ministry of Health gained all decision-making capacity, actions in nursing homes were by default delegated to regional governments and were outside the remit of the health authorities. This clearly hindered their capacity to intervene in the COVID-19 emergency.
Finally, nursing home provision in Italy and Spain is operated by a mix of charitable and religious bodies, public institutions and, increasingly, for-profit organisations. Of these last ones, differentiation between local or national companies and large international corporations adds further complexity to the picture. In Italy, the proportion of public residential beds has decreased from 45 per cent in 2002 to 21 per cent in 2016 as a consequence of the privatisation of many residential institutions (Arlotti et al. Reference Arlotti, Parma, Sabatinelli and Ranci2020). In Spain, the percentage of public nursing home beds is around one quarter of total supply and has not varied greatly over the last two decades. In both countries, the public-private mix has resulted in weak public regulation and control. Furthermore in the case of Spain, professional qualifications and quality standards for care are in general weakly established and monitored.
Conclusions
The management of the pandemic in nursing homes was structurally undermined by the delay in implementing preventive actions aimed at reducing the risk of infection. In this article, we have looked at how this delay in response and action played out in two European regions that were severely affected by the onset of the COVID-19 crisis. In Lombardy and Madrid, the delays in closure and the weak restrictions for access to nursing homes paved the way for the virus to spread in these institutions. In this context, the special regulations and controls necessary for adequate crisis management came late, especially when compared to actions carried out in health care systems. Key interventions such as buying PPE, expanding bed capacity and distributing quick tests, which in turn affected the reporting of cases, were delayed for weeks compared with the same measures implemented in hospitals. Furthermore, nursing homes were not only left to deal with a dramatic crisis alone, but were even wrongly considered a resource to be used to reduce the pressure of COVID-19 patients in hospitals (in Lombardy); in addition, they were denied support with residents failing to be hospitalised due to the implementation of a highly controversial triage system (in Madrid).
We have argued in this article that the untimely and inadequate response is at least partially explained by policy legacy effects. In particular, we have discussed the weak institutional embedding of residential care within the Italian and Spanish LTC systems in terms of public relevance, degree of public coverage and funding and regulation capacity. The general level of public commitment to residential LTC is still very low. The governance structure is also characterised by high institutional fragmentation in both countries.
One problematic aspect is the lack of coordination between social and health care services; this is a critical point for services, such as nursing homes, that need to provide both these services to their residents. Finally, the private sector clearly dominates service delivery, with an increasing role of profit-making agencies and extremely weak forms of public control and regulation. Overall, the policy legacies we have described cement a structural residualism of residential care in both countries that has severely hindered a swift response to a crisis of unprecedented magnitude.
Acknowledgments
Margarita León acknowledges the support form the ICREA foundation through the ICREA Academia programme. David Palomera acknowledges financial support from his PhD scholarship of the Catalan Administration [Grant number: 2020FI_B1 00049].
Appendix 1
Spain: References from Media outlets and official press releases
Media
El País 25/02/2020 http://bit.ly/ElPais_250220_CoronavirusNeumonia
El País 08/03/2020 http://bit.ly/ElPais_080320_VisitasResidencias
El País 06/03/2020 http://bit.ly/ElPais_060320_TengoCoronavirus
El País 18/03/2020 http://bit.ly/ElPais_180320_ResidenciasMorgues
El País 06/03/2020 http://bit.ly/ElPais_060320_CentrosdeJubilados
El País 12/03/2020 http://bit.ly/ElPais_120320_CaosHospitales
El País 12/03/2020 http://bit.ly/ElPais_120320_SanidadIncapacidadPruebas
El País 17/03/2020 http://bit.ly/ElPais_170320_19muertos
El País 19/03/2020 http://bit.ly/ElPais_190320_EjercitoResidencias
El País 22/03/2020 http://bit.ly/ElPais_220320_TestsRapidos
El País 26/03/2020 http://bit.ly/ElPais_260320_MuertesResidencias
El País 27/03/2020 http://bit.ly/ElPais_270320_AyusoCiudadanos
El País 8/04/2020 http://bit.ly/ElPais_080420_4750AncianosMueren
El País 11/04/2020 http://bit.ly/ElPais_110420_ConvenioEmpleados
El País 18/04/2020 http://bit.ly/ElPais_180420_ResidenciasTrampa
El País 19/05/2020 http://bit.ly/ElPais_190520_TrasladoNavas
El Diario.es 11/03/2020 http://bit.ly/ElDiario_110320_FernandoSimon
El Diario.es 23/03/2020 http://bit.ly/ElDiario_230320_EjercitoCadaveres
El Diario.es 26/03/2020 http://bit.ly/ElDiario_260320_ProtocoloDiscapacidad
El Diario.es 08/04/2020 http://bit.ly/ElDiario_080420_FallecidosResidencias
ABC 11/04/2020 http://bit.ly/ABC_110420_HotelesRescate
Press Notes Comunidad de Madrid
03/03/2020 http://bit.ly/NdP_030320_VideoRedes
09/03/2020 http://bit.ly/NdP_090320_MedidasExtraordinarias
13/03/2020 http://bit.ly/NdP_130320_ActivacionPlanProteccion
18/03/2020 http://bit.ly/NdP_180320_ControlResidencias
22/03/2020 http://bit.ly/NdP_220320_CompraMaterialUrgente
14/04/2020 http://bit.ly/NdP_140420_PruebasRapidasResidencias
15/04/2020 http://bit.ly/NdP_150420_MaterialesProteccion
Spain: Bills (Royal Decrees) concerning health and regulation in nursing homes
RDL 6/2020 of March 10
RDL 7/2020 of March 12
RDL 463/2020 of March 14
RDL 8/2020 of March 17
RDL 9/2020 of March 27
RDL 11/2020 of March 31
RDL 15/2020 of April 21
RDL 19/2020 of June 9
RDL 22/2020 of June 16
Order SND/265/2020 of March 19
Order SND/275/2020 of March 23
Order SND/344/2020 of April 13
Order SND/354/2020 of April 19
Order SND/387/2020 of April 21
Order SND/387/2020 of May 2
Order SND/299/2020 of May 9
Order SND/404/2020 of May 11
Order SND/422/2020 of May 19
Italy: References from Media
la Repubblica 05/04/2020
la Repubblica 05/04/2020
la Repubblica 06/04/2020
la Repubblica 16/04/2020
la Repubblica 25/04/2020
Corriere della Sera 04/04/2020
Corriere della Sera 08/04/2020
Corriere della Sera 10/04/2020
Corriere della Sera 18/04/2020
Corriere della Sera 23/04/2020
Il Fatto quotidiano 23/04/2020
Il Fatto Quotidiano 24/04/2020
https://www.ilfattoquotidiano.it/prima-pagina/la-lombardia-mente-sui-malati-nelle-rsa/
Italy: Decrees, circulars, ordinances concerning health and regulation in nursing homes
Council of Minister 31/01/2020
https://www.gazzettaufficiale.it/eli/id/2020/02/01/20A00737/sg
Council of Ministers 04/03/2020
https://www.gazzettaufficiale.it/eli/id/2020/03/04/20A01475/sg
Council of Ministers 08/03/2020
https://www.gazzettaufficiale.it/eli/id/2020/03/08/20A01522/sg
Council of Ministers 09/03/2020
https://www.gazzettaufficiale.it/eli/id/2020/03/09/20G00030/sg
Council of Ministers 17/03/2020
https://www.gazzettaufficiale.it/eli/id/2020/03/17/20G00034/sg
Ministry of Health 22/2/2020
Ministry of Health 23/02/2020
https://www.gazzettaufficiale.it/eli/id/2020/02/25/20A01273/sg
Ministry of Health 27/02/2020
Ministry of Health 17/03/2020
Ministry of Health 25/03/2020
Ministry of Health 03/04/2020
Ministry of Health 18/04/2020
Lombardy Region 25/02/2020
Lombardy Region 08/03/2020
Lombardy Region 30/03/2020
Lombardy Region 30/03/2020
Appendix 2
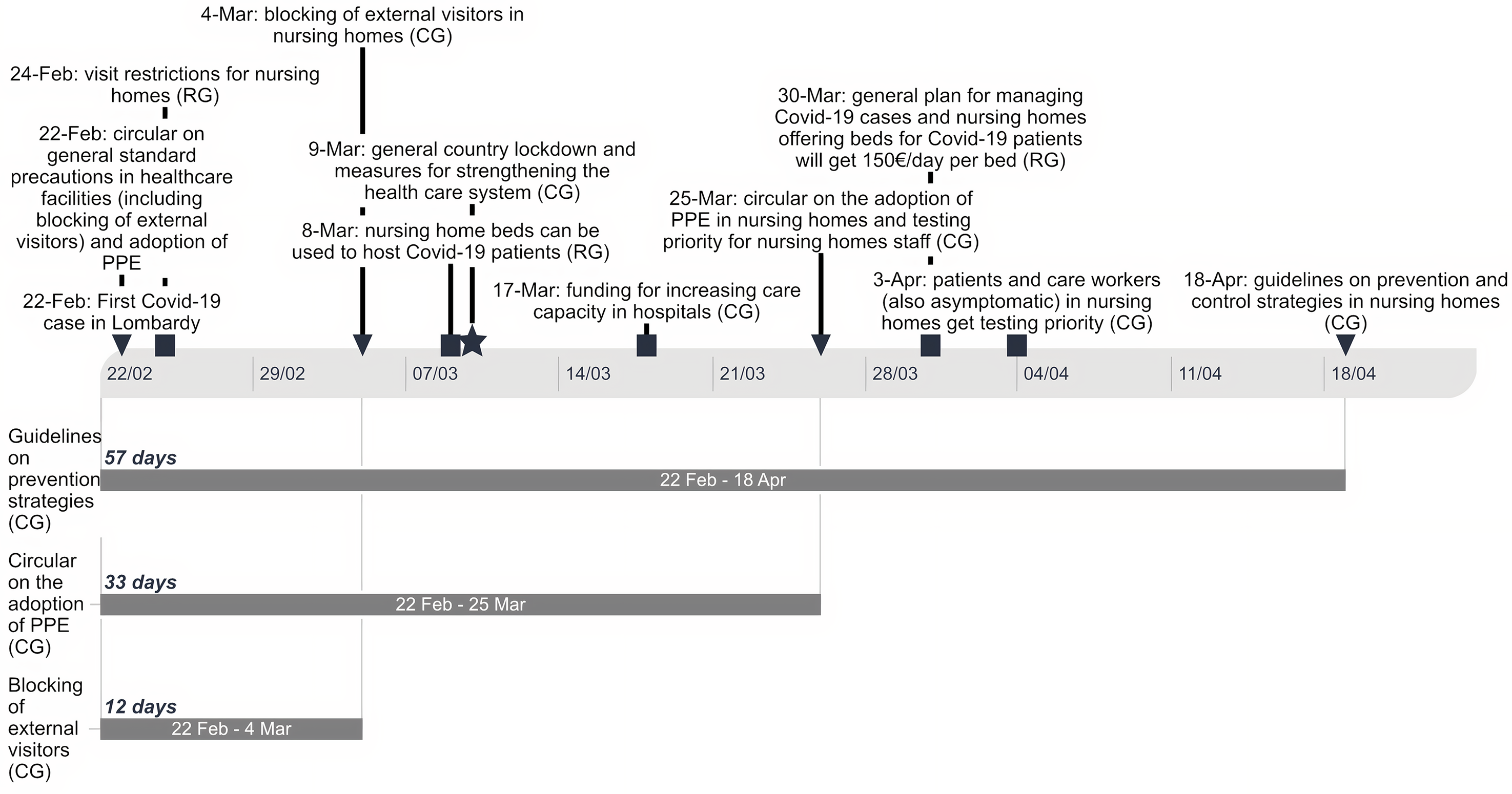
Figure A1. Timeline and policy delay: Italy
Source. Own elaboration
Note. RG: Regional Government; CG: Central Government
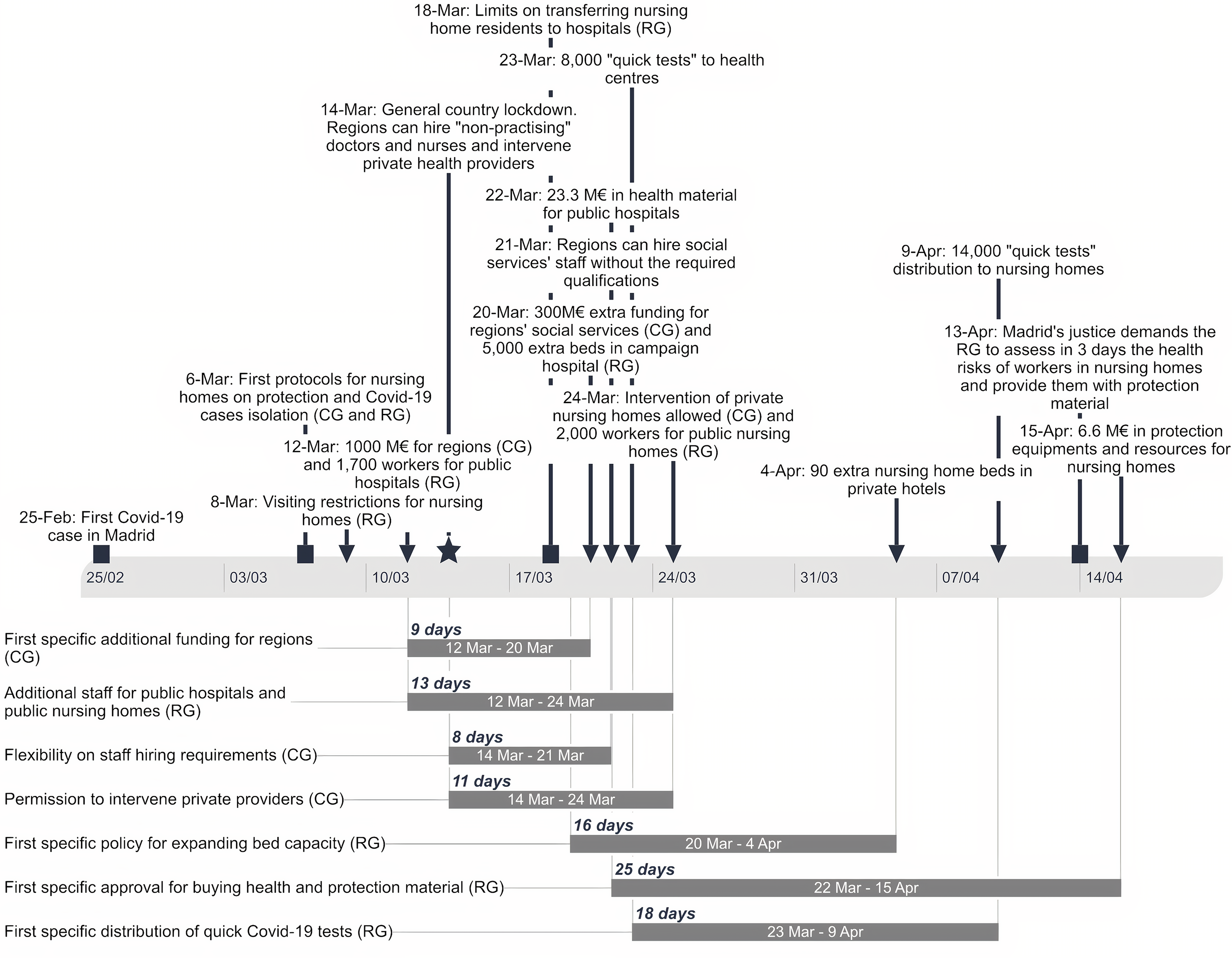
Figure A2. Timeline and policy delay: Spain
Source. Own elaboration
Note. RG: Regional Government; CG: Central Government








