Introduction
Attention-deficit/Hyperactivity Disorder (ADHD) is a neuropsychiatric condition that occurs in between 5.9% and 7.1% of children and adolescents (Willcutt, Reference Willcutt2012) and is the single most frequent reason for attendance at Child and Adolescent Mental Health Services (CAMHS) in Ireland (HSE, 2014). ADHD is characterised by difficulties in hyperactivity, inattention and impulsivity (APA, 2013). Typically, children present with additional school-related and behavioural difficulties (Loe & Feldman, Reference Loe and Feldman2007), and there is often associated family and parenting stress (Lifford et al. Reference Lifford, Harold and Thapar2008; Theule et al. Reference Theule, Wiener, Tannock and Jenkins2013). The most common treatment provided for child ADHD by psychiatrists in Ireland typically involves the use of psychostimulant medication, providing parenting advice, links with support groups, facilitating resources in the school and referral to a parenting programmes for parental management of the child’s behavioural difficulties (Seixas et al. Reference Seixas, Weiss and Müller2012). A specific focus on parents own mental health or stress level is often not explicitly part of the treatment offered, despite the salient role of parenting in determining outcomes (Modesto-Lowe et al. Reference Modesto-Lowe, Danforth and Brooks2008). Research suggests that parental stress and dysfunctional parenting may contribute to child behavioural difficulties (Neece et al. Reference Neece, Green and Baker2012). Conversely, early positive parenting interactions have been demonstrated to be a protective factor for the developmental course of conduct problems amongst children with ADHD (Chronis et al. Reference Chronis, Lahey, Pelham, Williams, Baumann, Kipp, Jones and Rathouz2007). This study identified praise, positive affect and warmth as specific aspects of positive parenting, which were observed to protect against future development of conduct problems. These early predictors of later conduct problems viewed as modifiable behaviours were presented as potential targets in the prevention and early intervention programmes.
Although Mindfulness has been practiced for over 2 millennia, it is only more recently that aspects of Buddhist mindfulness have been applied to elements of western psychotherapy (Van Gordon et al. Reference Van Gordon, Shonin, Griffiths and Singh2015). The Mindfulness-Based Stress Reduction (MBSR) programme was developed at the Stress Clinic in the University of Massachusetts Medical School in the late 1970s (Kabat-Zinn, Reference Kabat-Zinn2013), and the first to be formally introduced into clinical practice. In the 1990s, the Mindfulness-based Cognitive Therapy (MBCT) programme was developed in the UK encouraging the use of meditation as a secular practice to help individuals suffering from repeated bouts of depression and chronic unhappiness (Teasdale et al. Reference Teasdale, Segal and Williams2007). Since then, Mindfulness-based treatment programmes have been shown to have a positive impact on the psychological health of individuals, most notably: improvements in mood and quality of life (QOL) (Koszycki et al. Reference Koszycki, Benger, Shlik and Bradwejn2007); a reduction in perceived stress and burnout (Shapiro et al. Reference Shapiro, Astin, Bishop and Cordova2005); and a reduction in depressive relapse (Teasdale et al. Reference Teasdale, Segal, Williams, Ridgeway, Soulsby and Lau2000). Mindfulness techniques may also have an important role in increasing processing speed, memory and concentration (Murphy et al. Reference Murphy, Donovan and Taylor1997).
The strongest evidence for use of mindfulness-based interventions (MBIs) has been in depression and anxiety and within the adult population rather than child mental health services (Hofmann et al. Reference Hofmann, Sawyer, Witt and Oh2010). MBI has also found a welcome position alongside other interventions, such as dialectical behaviour therapy (DBT) (Linehan et al. Reference Linehan, Schmidt, Dimeff, Craft, Kanter and Comtois1999) and acceptance and commitment therapy (ACT) (Hayes et al. Reference Hayes, Strosahl and Wilson1999).
The mechanism of action of Mindfulness has occasionally been referred to as the ABC of Mindfulness. ‘A’ stands for ‘developing awareness’, often a bodily awareness, but also of intrusive and distracting thoughts, or habits. ‘B’ stands for ‘being with experience’ and turning towards difficult experiences with an attitude of acceptance. Finally, ‘C’ stands for making ‘wise choices’, having learnt to stay with difficult experiences (Groves, Reference Groves2016). To become aware of various stresses, and rather than avoid or cope maladaptively with them, the individual is encouraged to notice and accept them, pay attention to them in a curious and non-judgemental way, become aware that they are transient phenomena and respond or make decisions based on this experience. Home practice is considered essential and linked to better outcomes (Carmody & Baer, Reference Carmody and Baer2007).
Given the difficulties individuals with ADHD experience with inattention and distractibility, it is not surprising that the application of mindfulness has been studied in this population, albeit to a smaller extent. A meta-analysis of the effectiveness of mindfulness-based therapies (MBTs) for ADHD found MBTs to significantly reduce inattention and hyperactivity/impulsivity in individuals diagnosed with ADHD (Cairncross & Miller, Reference Cairncross and Miller2016). The effect size for reduction of inattention was larger for adults with ADHD, however, MBTs reduced symptoms of hyperactivity/impulsivity irrespective of age. A systematic review examining the use of meditation-based interventions in the treatment of children with ADHD found the majority of studies to report improvements in ADHD symptoms, however, the results were limited by the serious or critical risk of bias (Evans et al. Reference Evans, Ling, Hill, Rinehart, Austin and Sciberras2017). No study focused exclusively on parents of children with ADHD. Reported parent outcomes in interventions, which involved both parents and children suggested a reduction in parent ADHD symptoms, increased parental satisfaction and happiness, with mixed results for parental stress and over-reactivity. Evans et al. (Reference Evans, Ling, Hill, Rinehart, Austin and Sciberras2017) highlight the need for additional studies of mindfulness interventions for children with ADHD and their parents.
Although there is a growing literature on the effectiveness of MBI in youth with ADHD, existing studies are hampered by methodological issues, including small sample sizes (n = 10), ‘critical’ risk of bias and uncertainty regarding attendance ratings, it is difficult to differentiate lack of effectiveness from underpowered studies (Evans et al. Reference Evans, Ling, Hill, Rinehart, Austin and Sciberras2017). Based on the need for additional studies of MBIs for ADHD and local demand for non-pharmacological approaches for ADHD, an 8-week MBI was offered to parents of children attending any CAMHS for the treatment of ADHD. By adopting a non-restrictive recruitment strategy and having established evening time as the preferred time of delivery of parenting groups, this study sought to examine the feasibility and acceptability of such an intervention alongside routine CAMHS treatment in Ireland. Equally, it is plausible that parents of youth with ADHD, may also have ADHD themselves, and thus benefit from an MBSR course. However, ADHD-related difficulties with organisation, and attention may limit their ability to adhere to an 8-week course and engage in homework practice, limiting the feasibility of such an intervention.
We hypothesised that the adapted MBI offered in a clinical site in the evenings, would be feasible and acceptable to parents of children with ADHD, examining the rate of attendance and participation in home practice as the main outcome measures. The study also sought to examine if the intervention would result in improvements in parental stress levels, and parental QOL
Method
Participants
Information flyers regarding the adapted MBSR programme were forwarded to clinical staff working in South Dublin ADHD CAMHS clinics with the request to distribute to parents of children attending with a diagnosis of ADHD. These flyers were also made available in clinic waiting rooms and on the website of ADHD Ireland, an Irish charity providing support and information for families affected by ADHD (ADHD Ireland). Flyers included an email address through which parents could make contact for further information or to express interest in attending the programme. The inclusion criteria were parents of children under the age of 18 with a diagnosis of ADHD made by a CAMHS team. There were no specific exclusion criteria.
Forty parents responded to the flyer with 33 accepting places on the course and 29 ultimately attending. This included 23 mothers and 6 fathers, with both parents attending in 4 cases. Parents were considered participants if they completed the pre- and post-outcome measures and attended at least 2 sessions of the intervention.
MBI design
The MBSR programme was adapted for parents of children and adolescents with ADHD.
The course was delivered by a trained mindfulness teacher with experience in mindfulness for ADHD (CL). The course structure followed the standard MBSR model of eight, weekly, 2-hour sessions and one full day silent retreat (see Table 1). The group was run from 7 p.m. to 9 p.m. to facilitate the attendance of working parents. The sessions were held in a large room on the clinical site of the three CAMHS clinics from which the majority of participants were recruited. Participants were provided with a folder including weekly session content and record sheets. Weekly home practice was recorded by parents in this folder (see Table 1 for the content of home practice).
Table 1. Weekly sessions and homework
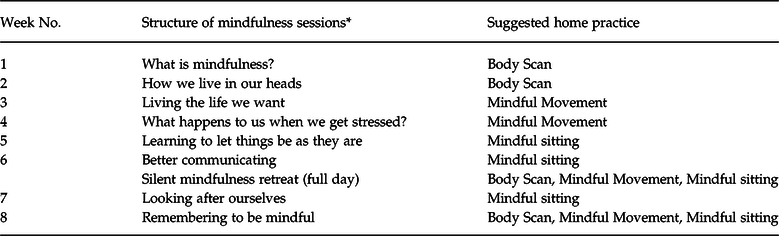
* General components of sessions are as follows: (1) Mindfulness Practice + Reflective Imagery; (2) Experimental Exercise + Group Discussion; (3) Didactic Teaching Topics; (4) Other Group Work.
Measures
Quantitative measures were administered at baseline and following intervention to assess for effectiveness.
Primary outcomes for parents
Our main outcome measure was to examine the attendance rate of parents, their engagement in home practice and any informal feedback they gave upon review at the end of treatment. This data were collected at each session by enquiry.
Secondary outcomes for parents
Parental stress scale (Berry & Jones, Reference Berry and Jones1995)
The Parental Stress Scale (PSS) measures the level of stress associated with raising children, focusing specifically on the stress generated by the parenting role (Berry & Jones, Reference Berry and Jones1995).
Respondents provide a response on a 5-point Likert scale, ranging from ‘strongly disagree’ to ‘strongly agree’, in terms of their typical relationship with their child. It is an 18-item scale giving a scale range of 0–90, with a higher score indicating higher levels of parental stress. The PSS has demonstrated adequate reliability (Cronbach’s alpha = 0.83) as well as adequate reliability over time (test–retest correlation = 0.81 over 6 weeks) (Berry & Jones, Reference Berry and Jones1995).
The parenting sense of competency scale (Gibaud-Wallston & Wandersman, Reference Gibaud-Wallston and Wandersman1978)
The Parenting Sense of Competency Scale (PSOC) is a 17-item scale. Each item is rated on a 6-point Likert scale anchored by 1 = ‘Strongly Disagree’ and 6 = ‘Strongly Agree’. Nine items are reverse coded, giving a range of 17–102. Higher scores indicate a higher parenting sense of competency, with no average scores or ‘cut-off’s’.
The World Health Organization quality of life – short form (WHOQOL-BREF) (WHOQOL Group, 1998)
The WHOQOL-BREF is a 26-item version of the WHOQOL-100 assessment, which measures QOL in four domains: physical, psychological, social and environmental. For each item, the participant responds to one of the four 5-point Likert interval scales, which reflect intensity, capacity, frequency and evaluation (Skevington et al. Reference Skevington, Lotfy and O’Connell2004). An overall score range is 24–120, with a higher score indicative of better QOL. The WHOQOL-BREF has been suggested to be a valid assessment of QOL (Skevington et al. Reference Skevington, Lotfy and O’Connell2004).
Mindful attention awareness scale (MAAS), trait version
The scale is a 15-item (1–6 Likert scale) questionnaire assessing dispositional (or trait) mindfulness, with higher scores reflecting increased mindfulness and self-regulation, and a range of 15–90. It has good psychometric properties (Brown & Ryan, Reference Brown and Ryan2003; Carlson & Brown, Reference Carlson and Brown2005). Internal consistency levels (Cronbach’s alphas) generally range from 0.80 to 0.90, population adult norms of 4.20 (s.d. 0.69) and it has high test–retest reliability.
Secondary outcomes for children
The strengths and difficulties questionnaire parent report
The Strengths and Difficulties Questionnaire (SDQ) is a 25-item child screening questionnaire made up of the following five subscales: Conduct Problems, Inattention–Hyperactivity, Emotional Symptoms, Peer Problems and Prosocial Behaviour (Goodman, Reference Goodman1997). Total scores range from 0 to 40, with scores above 17 being considered abnormal. The SDQ has been found to have satisfactory validity and reliability (Goodman, Reference Goodman2001).
Data analysis
Data were exported into SPSS 24. Frequency is provided for attendance rate and homework practice, and paired sample t-tests were used to determine if there was a significant difference in outcome measures (PSS, PSOC, MAAS and SDQ) mean score following intervention when compared to baseline.
Results
Twenty-nine parents enrolled in the study, with 26 attending at least 1 session. Not all parents completed baseline data, which is available on 25 parents. Twenty-three parents completed at least 1 of the MBSR sessions, and pre- and post-data were available for 8 parents (32%).
The mean age of participants was 48.9 and ranged from 37 to 61. The mean age of parents enrolled in the course (n = 29) was 48.88 years while the mean age of those who completed follow-up (n = 8) was 51.1 years, suggesting older parents were more likely to complete the course and to provide follow-up data.
The majority of participants were White Irish and the majority (n = 19, 76%) had completed third-level education. Twenty-two parents were married (88%), the others either single, widowed or divorced.
The average number of attendances was 6 (range 1–8) and, in general, parents engaged in home practice on average three times per week (range 0–7). A positive correlation was identified between how often a parent attended and both the number and duration of home practices (r(23) = 0.638, p = 0.001). Greater parental age positively correlated with the number (r(23) = 0.526, p = 0.007) and duration of home practices (r(23) = 0.458, p = 0.021) completed, but not with the number of sessions attended.
Of those who commenced the course, only a proportion completed and provided follow-up data. An independent sample t-test was used to compare baseline measures of those who completed the course and provided follow-up data (n = 8) and those who started but did not provide follow-up data (n = 17). Although those who completed follow-up had higher baseline PSS scores (mean 48.29, s.d. 8.015) than those not completing, (mean PSS 47.33, s.d. 9.462) this did not reach significance ((t (20) = −0.230, p = 0.821). Those completing follow-up also had lower baseline QOL scores (mean 99.13, s.d. 12.800) than those not completing, (mean 102.33, s.d. 17.775), also not reaching significance ((t (21) = 0.450, p = 0.657). Scores in the hyperactivity subscale of SDQ were non-statistically higher in those who completed follow-up (mean 8.43, s.d. 0.976) than those who did not (mean 7.63, s.d. 1.962) ((t (20.430) = 1.309, p = 0.205). Although none of these reached clinical significance, there was a trend for completers to show more impairment and distress
Parental stress levels showed a significant reduction (p = 0.03) post-intervention, from a pre-course mean of 48.29 to post-MBSR 41.00 (see Table 2).
Table 2. PSS, PSC, WHOQOL and SDQ outcomes

* p < 0.05.
Parental sense of competency also showed a small, but non-significant rise (p = 0.74) from a pre-course mean of 62.94 to a post-course mean of 63.54, indicating higher QOL post-intervention (see Table 2).
The total mean mindfulness score (MAAS) at baseline was 46.2, with an item mean of 3.08 and although this also increased post-intervention (total mean 51.6 and item mean 3.44,) it was not significant: t (12) = −1.09, p = 0.297.
A significant difference was documented between the mean parental pre-intervention score of the social relationships domain of the WHOQOL-BREF (M = 9.38) and post-intervention scores (M = 10.25), t(6) = −2.9, p = 0.021. Although improvements were also documented in the pre- and post-scores of the physical health domain and the pre- and post-scores of the psychological domain of the WHOQOL-BREF, these differences were not significant. The overall improvements in parental QOL are presented in Table 2.
Child ADHD symptoms
Pre-intervention mean SDQ hyperactivity scores fell into the ‘high’ category with a mean of 8.43 (using the four Band 4 Categorisation where scores >8 are considered ‘high’). Mean post-intervention scores were 7.0 (corresponding to the ‘slightly raised’ category). This reduction was significant; t(5) = 3,33, p = 0.016, suggesting some reduction in ADHD symptoms. Changes observed in other domains of the SDQ did not reach significance and are shown in Table 2.
Discussion
This pilot study offers preliminary evidence for an 8-week MBSR course for parents of children with ADHD.
Delivery of such an intervention was found to be acceptable to parents within the context of Irish CAMHS services. The 8 weeks MBSR programme was considered feasible in that it was offered as an adjunctive treatment alongside usual CAMHS treatment. Delivering the intervention required minimal support from clinical teams beyond the initial referral. High levels of initial interest in the course suggest a demand for such interventions. While outcome data were limited by low levels of completion of post-attendance outcome measures, attendance of sessions remained relatively consistent throughout the intervention period, with the average number of evening attendances at 6 (75%).
Quantitative results suggest that following the course, parents experienced a small but significant reduction in parental stress. With only seven parents completing pre- and post-measures of parental stress, further analysis of this group is limited. Another study reported a reduction in paternal but not maternal stress after mindfulness training, which was maintained at an 8-week follow-up (Van de Weijer-Bergsma et al. Reference van de Weijer-Bergsma, Formsma, de Bruin and Bögels2011) while a further study reported a worsening of parental stress following mindfulness intervention. Further larger scale studies are crucial to identify those parents most likely to respond favourably (Zhang et al. Reference Zhang, Chan, Lo, Chan, Chan, Ting, Gao, Lai, Bögels and Wong2016).
A significant improvement was observed in the parental QOL with specific improvements in social relationships. The social relationships domain of the WHOQOL-BREF asks participants about their satisfaction with personal relationships, sex life and support received from friends. The participant mean pre- and post-score reported was above the UK mean (Skevington et al. Reference Skevington, Lotfy and O’Connell2004) and the mean reported by parents of children with ADHD in a Hong Kong sample (Xiang et al. Reference Xiang, Luk and Lai2009). Possible explanations for the increase in this domain may be that participants developed relationships with, and felt supported by, other parents in the group, with whom they had a shared experience of parenting a child with ADHD and of participating in the group. Additionally, participants may have developed a greater awareness of their personal relationships and social support outside of the group, through cultivating mindfulness skills, such as awareness of the present moment, non-judgement, acceptance and reduced reactivity. A previous review has suggested higher levels of mindfulness, both dispositional and learned, to be correlated with greater relationship satisfaction (Kozlowski, Reference Kozlowski2013).
Although there was an increase in mindfulness scores and parental sense of competency post-intervention, these were not significant.
As per the SDQ’s Band 4 Categorisation, the pre-test mean of child hyperactivity symptoms fell into the ‘high’ category (scores greater than 8), while the post-test mean fell into the ‘slightly raised’ category (scores 6–7). Although a small reduction in reported ADHD symptoms is welcome, the lack of teacher-reported measures contributes some uncertainty to the interpretation. This could suggest either a true reduction in child ADHD symptoms or parental perception of improvement, perhaps mediated by a more tolerant or reflective response to their behaviour. SDQ scores, while recorded, were not considered a primary outcome measure given the short intervention time of 8 weeks and short follow-up period. Furthermore, we did not collect any other potentially confounding variables such as change in medication dose, school-related changes or other parent or child ADHD specific interventions. It would be useful to know if a blinded or independent report of SDQ, as given by a teacher unaware of intervention, would also endorse a reduction in symptoms. It is acknowledged in the literature that when an independent and more distant reporting procedure is used, for example, SDQ rated by teacher, blinded to the study intervention, that the efficacy of interventions is reduced (Sonuga-Barke et al. Reference Sonuga-Barke, Brandeis, Cortese, Daley, Ferrin, Holtmann, Stevenson, Danckaerts, Van der Oord, Döpfner and Dittmann2013). To some extent, a perceived rather than actual improvement in child functioning might in itself be welcome. Further studies should include parental and teacher ratings to disentangle this issue.
A similar reduction in child ADHD symptoms has been documented in studies in which children also received a mindfulness intervention, such as Lo et al. (Reference Lo, Wong, Wong, Yeung, Snel and Wong2017), who documented a significant reduction in child ADHD symptoms as per the SWAN rating scale. To the authors’ awareness, this is the first study that has documented a significant difference in child ADHD symptomology following an intervention offered to parents alone.
Previous literature has identified an improvement in the psychological domain of QOL following mindfulness programmes for parents of children with autism spectrum disorder (Rayan & Ahmad, Reference Rayan and Ahmad2016).
A recent overview of meta-analysis and systematic reviews conclude that mindfulness is effective in improving outcomes in a number of varied psychological and physical problems, and overall QOL (Gotink et al. Reference Gotink, Chu, Busschbach, Benson, Fricchione and Hunink2015). The benefits and potential applicability of Mindfulness are such that an all All-Party Parliamentary Group was setup in the UK (Mindful Nation UK) to review the scientific evidence and best practice and to develop policy recommendations for the government (Hyland, Reference Hyland2016). The authors concluded that Mindfulness intervention, and more specifically MBCT, should be made widely available, not only in medical settings but in school and the workplace, and research into its application should continue.
This pilot study is limited by the small number enrolled in the study, and low rates of return of time 2 data by those who completed the intervention. The demographics of participants, most of whom were White, Irish and had completed third-level education is unlikely to be an accurate representation of cases in the general population and is a further limitation in terms of the generalisability of this intervention. However, it does add to the literature of a potential positive effect of parentally focussed MBSR in a cohort of ADHD youth. To the authors’ knowledge, it is the first study that has measured the impact of a mindfulness programme for parents of children with ADHD on a range of measures.
Conclusion
MBSR programmes have found their way into routine clinical practice for a range of mental health disorders, and have been linked with an improvement in QOL more generally. This study suggests that it may be a useful adjunct as part of an ADHD treatment plan, in terms of acceptable attendance rates, positive perspectives of most of those who completed the intervention and an improvement in the parental QOL. Children’s hyperactivity scores were also significantly reduced. However before MBSR is rolled out into routine practice, further studies with larger numbers are required to attest to both efficacy and cost-effectiveness. The authors are currently undertaking a multisite RCT and hope that this might provide some additional data.
Acknowledgements
Our gratitude to the parents who participated in this study and to Dr Marc Bennett TCD for his help in an earlier pilot.
Conflicts of interest
RR, ANB, KK, CL and FM have no conflict of interest to disclose.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committee on human experimentation with the Helsinki Declaration of 1975, as reviewed in 2008. The authors assert that ethical approval was obtained from Saint John of God Hospital Ethics Committee in January 2018.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.




