Introduction
Knowledge on different kind of risk factors for children of parents with schizophrenia (SZ) and bipolar disorder (BP) is well established, e.g. having early mental health problems and disorders (Davidsen et al., Reference Davidsen, Munk-Laursen, Foli-Andersen, Ranning, Harder, Nordentoft and Thorup2021; Rasic, Hajek, Alda, & Uher, Reference Rasic, Hajek, Alda and Uher2014; Thorup et al., Reference Thorup, Laursen, Munk-Olsen, Ranning, Mortensen, Plessen and Nordentoft2018) and living with social disadvantages (Manning & Gregoire, Reference Manning and Gregoire2006). Early manifestations of vulnerability have been documented in children of parents with SZ and BP (Díaz-Caneja et al., Reference Díaz-Caneja, Morón-Nozaleda, Vicente-Moreno, Rodríguez-Toscano, Pina-Camacho, de la Serna, Sugranyes, Baeza, Romero and Sánchez-Gistau2018), where some seem to be more specific to children of parents with SZ (deficits in neurocognition (Agnew-Blais & Seidman, Reference Agnew-Blais and Seidman2013; Bora & Özerdem, Reference Bora and Özerdem2017; Hemager et al., Reference Hemager, Plessen, Thorup, Christiani, Ellersgaard, Spang, Burton, Gregersen, Søndergaard and Greve2018) and social cognition (Christiani et al., Reference Christiani, Jepsen, Thorup, Hemager, Ellersgaard, Spang, Burton, Gregersen, Søndergaard and Greve2019)) or are seen with greater severity (Maziade et al., Reference Maziade and Rouleau2009). Both offspring groups are also at an increased risk of experiencing non-optimal caregiving (Manning & Gregoire, Reference Manning and Gregoire2006). There has been limited research on the, often hidden, burden of the co-parent who together with a parent with SZ or BP, care for their children (Rose, Reference Rose1996). Given the risks and the challenges for both the children and the parents in families with parental SZ or BP, there is a strong need for increased knowledge about the specificity of any caregiving difficulties in these families in order to develop effective interventions and preventive strategies. The impact of being diagnosed with a severe mental illness (SMI) on the ability to provide good caregiving has been investigated using various methods, but knowledge is often restricted to certain age groups. Previous studies have had an almost unilateral focus on caregiving behavior (e.g. the parent’s affective responses to the child (Ainsworth, Blehar, Waters, & Wall, Reference Ainsworth, Blehar, Waters and Wall2015; Slade, Grienenberger, Bernbach, Levy, & Locker, Reference Slade, Grienenberger, Bernbach, Levy and Locker2005)) and adult attachment (Hesse, Reference Hesse2016). Moreover, only limited research is focusing on the important contributions of caregivers’ emotional experiences with their children as conceived from the theory about “the caregiving system” (George & Solomon, Reference George and Solomon2011). The caregiving system stems from attachment theory and requires that the caregiver makes a critical psychological shift away from seeking protection (the attachment system) to providing protection and care for the child (the caregiving system) (George & Solomon, Reference George and Solomon2011). Feelings of helplessness and fear in the caregiver can undermine the ability to make this important psychological shift. If feelings of helplessness or fear are triggered; e.g. when dealing with a mental illness while being responsible for a child (Huth-Bocks, Guyon-Harris, Calvert, Scott, & Ahlfs-Dunn, Reference Huth-Bocks, Guyon-Harris, Calvert, Scott and Ahlfs-Dunn2016; Oyserman, Mowbray, Meares, & Firminger, Reference Oyserman, Mowbray, Meares and Firminger2000; Røhder et al., Reference Røhder, MacBeth, Agnete Davidsen, Gumley, Brennan, George and Harder2020), the caregiver is at risk of lashing out, retreating or seeking comfort and protection from the child (role reversal) and thereby exposing the child to what has been termed ‘disorganized caregiving’(George & Solomon, Reference George and Solomon2011). It is theorized that disorganized caregiving can predict disorganized attachment in children (Solomon & George, Reference Solomon and George2011)—an attachment style associated with an elevated risk of negative developmental outcomes (Borelli, David, Crowley, & Mayes, Reference Borelli, David, Crowley and Mayes2010).
Research in caregiving among parents with SZ and BP is sparse and ambiguous. One study found that mothers diagnosed with BP, depression or psychosis antenatally showed higher levels of disorganized caregiving representation than controls, with mothers diagnosed with psychosis having the highest level (Røhder et al., Reference Røhder, MacBeth, Agnete Davidsen, Gumley, Brennan, George and Harder2020). However, when looking at perinatal maternal behavior, mothers with psychosis and BP resembled non-clinical mothers, and only mothers with depression expressed more overriding behavior compared to mothers without SMI. A systematic review concluded that mothers with SZ show reduced social contact, greater tension and more behavioral intrusiveness towards their infants compared to controls (Davidsen, Harder, MacBeth, Lundy, & Gumley, Reference Davidsen, Harder, MacBeth, Lundy and Gumley2015). However, the quality of the interaction between mother and infant seems to improve when maternal psychotic symptoms decline (Snellen, Mack, & Trauer, Reference Snellen, Mack and Trauer1999). Studies on caregiving in parents with BP are few with mother’s depression being associated with disruptions in caregiving (George & Solomon, Reference George and Solomon2011; Huth-Bocks et al., Reference Huth-Bocks, Guyon-Harris, Calvert, Scott and Ahlfs-Dunn2016; Trapolini, Ungerer, & McMahon, Reference Trapolini, Ungerer and McMahon2008). Compared to controls both mothers with BP and their infant show less positive affect when interacting and their interactions are characterized by more tension and less mutuality and reciprocity both at 3 and 12 months of age (Anke et al., Reference Anke, Slinning, Moe, Brunborg, Siqveland and Skjelstad2019, Reference Anke, Slinning, Moe, Brunborg, Siqveland and Skjelstad2020). To our knowledge, no research exists concerning the caregiver’s experiences of helplessness, fear and role reversal among parents with either SZ or BP and their co-caregivers having children in middle childhood. Individuals, who are diagnosed with SZ, are most at risk of developing chronicity and having the most severe symptoms (Gottesman, Reference Gottesman1989; Heslin et al., Reference Heslin, Lappin, Donoghue, Lomas, Reininghaus, Onyejiaka, Croudace, Jones, Murray and Fearon2016), and therefore it is conceivable that parents with SZ (and their co-parent) could be more burdened in the caregiver role, but there is a lack of knowledge about differences in caregiving experiences between parents diagnosed with SZ and BP. Furthermore, research regarding caregiving and SMI has mainly focused on caregivers with mental illness, while less attention has been paid to the quality of caregiving provided by the co-parent. However, mental illness can be associated with a high level of psychological distress and burden also on the co-parent (Greve et al., Reference Greve, Uher, Als, Jepsen, Mortensen, Gantriis, Ohland, Burton, Ellersgaard and Christiani2021; Saunders, Reference Saunders2003). The majority of adults in families with parental mental illness experience some kind of burden, such as self-sacrifice, feelings of being overloaded and volatility in the relationship (Azorin, Lefrere, & Belzeaux, Reference Azorin, Lefrere and Belzeaux2021; Rose, Reference Rose1996). However, a review concluded that the chronicity of some mental illnesses may lead to development of personal coping styles in some families, such as maintaining a balance in family life and developing a sense of self-enrichment (Rose, Reference Rose1996). It is important to remember that these families are very different in terms of both illness severity, adherence to treatment and level of functioning.
Measuring indicators of disorganized caregiving
George and Solomon (Reference George and Solomon2011) developed the Caregiving Helplessness Questionnaire (CHQ) as a screening tool for ‘disorganized caregiving’. The CHQ examines caregivers self-reported experiences of helplessness, fear in the caregiver–child relationship, and caregiver–child role reversal (child caregiving), which are indicators of disorganized caregiving (George & Solomon, Reference George and Solomon2011). The CHQ scales Helplessness and Frightened are associated with mother’s depression, caregiving stress (e.g. problems in becoming attached to the child) and child externalizing and internalizing problems (George & Solomon, Reference George and Solomon2011). Unexpected lack of associations with the Child Caregiving scale led to an exploratory analysis whereby four groups, based on scores from two of the scales, Frightened- and Child Caregiving, were created. It was suggested that the combination of high Frightened and high Child Caregiving (“high” defined as the upper quartile) may represent a more vulnerable group—the combinations were associated with the highest levels of helplessness, depression, mother and child stress, and child behavior problems (George & Solomon, Reference George and Solomon2011). It is important to investigate whether the combination of (1) the perception of fright in the relationship between caregiver and child (high Frightened) and (2) the perception of the child as capable of taking care of others (Child Caregiving) could be a significant environmental stressor for children at familial high risk of SZ (FHR-SZ) or familial high risk of BP (FHR-BP), as this may highlight a possible risk factor that contributes to the etiology of SMI.
Aims and hypothesis
This study aimed to explore if parents with SZ or BP and their co-parents are more likely to express experiences of helplessness, fear and role reversal in relation to the child they care for compared to population-based controls (PBCs). Further, we aimed to investigate whether these indicators of disorganized caregiving are associated with the caregivers’ and children’s level of function and the children’s internalizing and externalizing behavior problems. We hypothesized that caregivers diagnosed with either SZ or BP and their co-caregivers would report higher levels of helplessness, fear and role reversal compared to PBCs. Investigating diagnostic group differences in caregiving representations we hypothesized caregivers with SZ to report higher levels of disorganized caregiving compared to caregivers with BP. Finally, we hypothesized a negative correlation between indicators of disorganized caregiving and the caregivers’ and children’s level of functioning respectively. We expected to find positive associations between higher scores on indicators of disorganized caregiving and children’s internal and external behavior problems. Exploratively, we investigated whether it was possible to identify an at-risk group of children, whose caregivers express a high level of fear and role reversal in the caregiving relationship.
Method
Study design
This study is part of the Danish High Risk and Resilience Study—VIA 7, hereafter The VIA 7 study. The VIA 7 study is a nationwide population-based cohort study of 522 seven-year-old children at either FHR-SZ or FHR-BP and PBC. The study design has been thoroughly described elsewhere (Thorup et al., Reference Thorup, Jepsen, Ellersgaard, Burton, Christiani, Hemager, Skjærbæk, Ranning, Spang and Gantriis2015). Data were collected from January 2013 until January 2016.
Ethics and procedure
The study was approved by the Danish Data Protection Agency. The Danish Ministry of Health granted permission to retrieve data from the Danish registers. Approval from the Danish Committee on Health Research Ethics was not needed due to the non-interventional nature of the study. Written informed consent was obtained from all adult participants and from the legal guardians of the participating children. The study assessors were trained psychologists, medical doctors and nurses supervised by a specialist in child and adolescent mental health (AAET) and a certified specialist in clinical child neuropsychology (JRMJ). To ensure blinding to FHR status regarding the assessment of children’s daily functioning and psychopathology and the assessment of children’s general intelligence, different investigators assessed the caregiver and the child.
Participants
All 522 seven-year-old children were born and living in Denmark. The children had one or two biological parents diagnosed with SZ spectrum psychosis (ICD-10 codes F20, F22 and F25, or ICD-8 codes 295, 297, 298.29, 298.39, 298.89 and 298.99) or bipolar disorder (ICD-10 codes F30 and F31, or ICD-8 codes 296.19 and 296.39) or parents with neither of these disorders. Families were identified using the Danish Civil Registration System (Pedersen, Gøtzsche, Møller, & Mortensen, Reference Pedersen, Gøtzsche, Møller and Mortensen2006) and the Danish Psychiatric Central Research Register (Mors, Perto, & Mortensen, Reference Mors, Perto and Mortensen2011), including both inpatient and outpatient contacts. PBCs were matched to the families in which at least one parent had been diagnosed with SZ on sex, age and municipality of the child. Families in which at least one parent had been diagnosed with BP were a non-matched sample, but they were comparable to the other two groups in terms of age and sex of the children. PBCs could be registered with any other psychiatric diagnoses than SZ or BP. The caregivers with SZ or BP, the Index parents, were labeled SZ-I, BP-I. The co-caregivers (i.e. the caregivers without a diagnosis of SZ or BP in Danish registries), who were past or present partners to a person diagnosed with SZ or BP or foster parents/grandparents to a child having a parent(s) with either SZ or BP) were labeled SZ co-caregiver and BP co-caregiver, and the caregivers from the PBC group were labeled PBC. In each family, only one main informant was identified as the primary caregiver of the child. The primary caregiver was the adult who currently spent the most time with the child. Thus, a primary caregiver could either be a biological parent diagnosed with SZ or BP, or it could be the co-parent to a parent diagnosed with SZ or BP (i.e. ‘the other parent’) or a PBC. Only primary caregivers were asked to complete the CHQ (George & Solomon, Reference George and Solomon2011), which was done by 479 in this study.
Measures
Caregiving helplessness questionnaire
The CHQ (George & Solomon, Reference George and Solomon2011) was administered as a self-report measure to assess the primary caregivers’ feelings of helplessness, fear, and role reversal (child caregiving) in the relationship with the child. It is a 26-item self-report questionnaire assessing the core dimensions of disorganized caregiving representation (expressed in three subscales). The Helplessness subscale consists of seven items (e.g., “When I am with my child, I often feel out of control”), six items constitute the Frightened subscale (e.g., “I am frightened of my child” and “I feel that I punish my child more harshly than I should”), and six items constitute the Child Caregiving subscale (e.g., “My child is good at tending to and caring for others”). The remaining seven items are fillers to disguise the purpose of the questionnaire (e.g., “I enjoy doing things with my child that make him or her happy”). All items are rated on a scale ranging from 1 (not characteristic at all) to 5 (very characteristic). Subscale scores range from 7 to 35, 6 to 30, and 6 to 30, respectively, and higher scores reflect more of the given dimension, i.e. higher perceptions of helplessness, fear and role reversal. George and Solomon (Reference George and Solomon2011) reported an adequate internal reliability, with alpha coefficients of .85 for Helplessness, .66 for Frightened, and .64 for Child Caregiving among their middle class, ethnically diverse mothers (N=59) of 3- to 11-year-old children. The questionnaire was translated into Danish by a specialist in child and adolescent mental health (AAET) and back-translated by a native speaking translator, who did not know the original wording, and then approved by one of the developers (CG) of the questionnaire.
Other measures
Assessment of caregiver’s and children’s current level of functioning
The primary caregiver’s current level of functioning was assessed with the Personal and Social Performance Scale (PSP) (Morosini, Magliano, Brambilla, Ugolini, & Pioli, Reference Morosini, Magliano, Brambilla, Ugolini and Pioli2000). The PSP interview was rated based on the level of function during the previous month in four domains (socially useful activities, personal and social relationships, self-care, and disturbing and aggressive behavior), which is rated on four subdimensions; a total score on a 100-point scale is set, where lower scores reflect poorer function.
The children’s current level of functioning was assessed with the Children’s Global Assessment Scale (Shaffer et al., Reference Shaffer, Gould, Brasic, Ambrosini, Fisher, Bird and Aluwahlia1983) as part of the semi-structured interview K-SADS-PL. The child is rated on a scale from 0 to 100 with lower scores reflecting poorer levels of functioning based on the child’s daily functioning in the previous month.
For the assessment of caregivers’ and children’s current level of functioning, consensus meetings were held regularly to secure agreement among raters.
Assessment of children’s psychopathology
Any possible current diagnoses of the children were assessed with K-SADS-PL interview (the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version) (Kaufman et al., Reference Kaufman, Birmaher, Brent, Rao, Flynn, Moreci, Williamson and Ryan1997). All interviewers attended a formal K-SADS-PL course prior to data collection. The semi-structured interview was conducted first with the primary caregiver and then with the child. All possible diagnoses were confirmed at consensus meetings with a specialist in child and adolescent psychiatry (AAET). The interrater reliability for the assessment of psychopathology was estimated using Krippendorff’s alpha with 95% bootstrap confidence intervals (Zapf, Castell, Morawietz, & Karch, Reference Zapf, Castell, Morawietz and Karch2016). All interviewers were required to watch ten selected video-recorded K-SADS-PL interviews and determine whether a skip-out criterion was met. The combined observed agreement of KSADS-PL skip-out criteria across sections in the screening interview was 90.3%. Krippendorff’s alpha was .74 (95% CI: .63–.82).
The questionnaire Child Behavior Checklist (school-age version (CBCL) (Achenbach & Rescorla, Reference Achenbach and Rescorla2001)) was completed by the primary caregiver. It includes 118 problem behavior items rated on a Likert scale from 0 (not true) to 2 (very true or often true) and reports dimensional psychopathology. Higher scores reflect more problem behavior. We used the two broadband subscales (Internalizing and Externalizing) and the CBCL total score.
Assessment of caregiver’s and children’s general intelligence
An estimate of the caregivers and children’s general intelligence was assessed using the Reynold’s Intellectual Screening Test (RIST) (Reynolds & Kamphaus, Reference Reynolds and Kamphaus2003). The RIST consist of a verbal subtest (Guess What) and a nonverbal subtest (Odd-Item Out). The RIST index is based on norms stratified on age (Reynolds & Kamphaus, Reference Reynolds and Kamphaus2009).
The test performance on the RIST from at least 40 children were rescored by a specialist in child psychology (NH) or a trained psychology student who was blinded to the familial risk status and the original scoring. The initial scoring was accepted when the intraclass correlation was greater than .90. The Intraclass correlation coefficient was higher than .90 for both subtests.
Statistical analysis
The statistical analyses were performed with the statistical software SPSS Statistics 25 (IBMCorp Ibm, 2017) and Stata/SE version 15.1 (StataCorp, Reference StataCorp2017). Group characteristics on socioeconomic (i.e. parental status of employment and educational level), clinical and home status (e.g. whether children are living with both biological parents) variables were summarized using standard descriptive statistics and chi-square, including group comparisons with one-way analysis of variance (ANOVA) and pairwise comparison using Fisher’s Least Significant Difference. Internal reliability for each subscale in the CHQ (Caregiving Helplessness, Frightened Caregiving and Child Caregiving) was measured using Cronbach’s alpha (Tavakol & Dennick, Reference Tavakol and Dennick2011). Differences between caregivers diagnosed with SZ or BP, co-caregivers to a person diagnosed with SZ or BP and PBC regarding experiences of helplessness, fear and role reversal were examined using one-way ANOVA and pairwise comparison using Fisher’s Least Significant Difference. Differences that are significant after a Bonferroni correction are marked with *. Group differences were first examined in the three groups (SZ combined, BP combined and PBC) and afterwards the SZ combined and the BP combined group were further divided into four groups: (1) Caregivers diagnosed with SZ, (2) Co-caregivers to a child with a parent diagnosed with SZ (SZ co-caregiver), (3) Caregivers diagnosed with BP, (4) Co-caregivers to a child with a parent diagnosed with BP (BP-co-caregiver), and (5) PBC. One CHQ answer had two missing items where a mean score was given. A questionnaire is completed if two or less questions are missing. Pearson’s 2-tailed correlation analysis was used to evaluate correlations among caregiving representations and caregivers’ level of function, child level of function and child emotional and behavioral problems. A general linear model was performed with the groups (SZ combined, BP combined and PBC) as an interaction to investigate whether any correlations between the CHQ scales and function scores for children and caregivers respectively as well as children’s internalizing and externalizing behavior problems were significantly different across the three groups. The explorative analysis on the CHQ combined scales (High Frightened and High Child Caregiving) was examined by first dividing the caregivers into four groups based on the groups created by George and Solomon (Reference George and Solomon2011), using their defined upper quartile as a cut-off for a high score (Scores above 9 for the Frightened Caregiving subscale and scores above 22 for the Child Caregiving Subscale), and then using one-way ANOVA and pairwise comparison with Fisher’s Least Significant Difference to examine between-group differences. The explorative analysis on the four created groups were defined and labeled as followed: Frightened and Child Caregiving (F&CC; scores above cut-off for both Frightened Caregiving and Child Caregiving), Frightened Only (F Only, scores above cut-off for only Frightened Caregiving), Child Caregiving Only (CC Only, scores above cut-off for only Child Caregiving), and Neither Frightened nor Child Caregiving (Neither, no scores above cut-off).
Results
Sample characteristics
From our cohort of 522 children and their primary caregivers, 185 caregivers belonging to the SZ combined group (i.e. SZ-I + SZ co-caregiver), 110 caregivers to the BP combined group (i.e. BP-I + BP co-caregiver), and 184 caregivers to the PBC group provided data on CHQ. A minority of subjects from the full VIA 7 cohort did not provide data on the CHQ (N = 43; 17 (8.4%) from the SZ combined group, 10 (8.3%) from BP combined group and 16 (8.0%) from PBC) mainly due to discontinuation of participation in the study. The caregivers in the three groups did not differ significantly regarding sex distribution, but caregivers in the SZ combined group and BP combined group were more frequently unemployed and had significantly poorer levels of function measured on the PSP scale compared to PBCs (Table 1). Significantly more adults in the SZ combined group had a lower education than adults in the BP combined group and PBCs. Adults in the BP combined group had higher IQ than adults in the SZ combined group (Table 1). None of the caregivers, who provided data on the CHQ, had an IQ score below 70.
Table 1. Sample characteristics of caregivers and their children according to parental diagnostic group
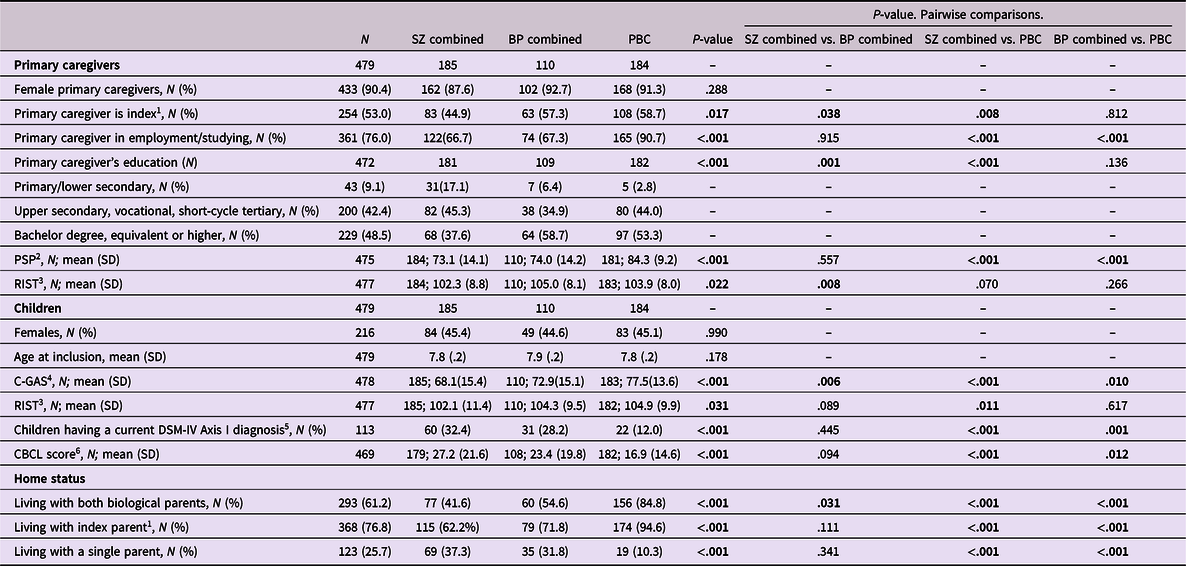
Table 1 statistical analyses: Standard descriptive statistics and chi-square, including group comparisons with one-way ANOVA and pairwise comparison using Fisher’s Least Significant Difference. SZ combined refer to caregivers with a SZ diagnosis, or past or present partners to a person diagnosed with SZ or foster parents/grandparents to a child having a parent(s) with SZ and their respective children; BP combined refer to caregivers with a BP diagnosis, or past or present partners to a person suffering from BP or foster parents/grandparents to a child having a parent(s) with BP and their respective children; PBC refer to population-based control group.
1 Index refer to the biological parents with a diagnosis of schizophrenia spectrum psychosis or bipolar disorder.
2 Primary caregiver’s level of function (Personal and Social Performance Scale), total score on a 100-point scale, a low score reflects a poor level of function.
3 Reynolds Intellectual Screening Test, a low score reflects a low IQ.
4 Children’s level of functioning (The Children’s Global Assessment Scale), total score on a 100-point scale, a low score reflects a poor level of function.
5 The diagnostic screening interview K-SADS-PL. Current refers to past two months. Transient tics, tics NOS and elimination disorders not included.
6 Child Behavior Checklist school-age version. A high score reflects more internalizing and/or externalizing behavior problems.
The children did not differ significantly regarding age and sex but children at FHR-SZ and FHR-BP had a significantly poorer level of function, were more likely to have a mental illness and to have more emotional and behavioral problems compared with controls (Table 1). PBC had significantly higher IQ than children at FHR-SZ.
A significantly larger proportion of the children at FHR-SZ and FHR-BP did not live with both biological parents compared to PBCs. There were significantly more single caregivers in the FHR-SZ and FHR-BP groups compared to PBC (Table 1).
Internal reliability for each subscale
Alpha coefficients were acceptable for Caregiving Helplessness, α = .79, but low for Frightened Caregiving, α = .51 and Child Caregiving, α = .58.
Indicators of disorganized caregiving in families with SZ or BP
We found significant differences between the three groups on Caregiving Helplessness (p < .001) and Frightened Caregiving (p = .001) (Table 2). The results of the pairwise comparison revealed that SZ combined group (N = 185, 38.6%) and BP combined group (N = 110, 23%) had significantly higher scores of Helplessness and Frightened Caregiving compared to the PBCs (N = 184, 38.4%), but there was no significant difference between the two combined groups. Child Caregiving did not differ across the three groups.
Table 2. Experiences of helplessness, fear and child caregiving reported by caregivers from the SZ combined group and the BP combined group and the PBC group

* P<.05 with Bonferroni correction. Table 2 statistical analyses: One-way ANOVA and pairwise comparison using Fisher’s Least Significant Difference. SZ combined refer to caregivers with a SZ diagnosis, or past or present partners to a person suffering from SZ or foster parents/grandparents to a child having a parent(s) with SZ; BP combined refer to caregivers with a BP diagnosis, or past or present partners to a person suffering from BP or foster parents/grandparents to a child having a parent(s) with either BP; PBC refer to Population-based control group.
1 Scale scores can range from 7 to 35. Higher scores reflect more Caregiving Helplessness.
2 Scale scores can range from 6 to 30. Higher scores reflect more Frightened Caregiving.
3 Scale scores can range from 6 to 30. Higher scores reflect more Child Caregiving (i.e. Role Reversal).
Impact of SZ and BP on experiences of helplessness, fear and role reversal: Differences between having a diagnosis and being the co-caregiver
The result showed a significant difference on Caregiving Helplessness (<.001) and Frightened Caregiving (p = .001) across the five groups (Table 3), with caregivers with SZ (N = 83, 17.3%) or BP (N = 63, 13.2%) and co-caregivers (SZ co. N = 102, 38.6%; BP co. N = 47, 9.8%) displaying significantly higher scores on Caregiving Helplessness compared to PBC. Furthermore, caregivers diagnosed with BP had significantly higher scores on Caregiving Helplessness compared to caregivers diagnosed with SZ and compared to BP co-caregivers. We found no difference between caregivers diagnosed with SZ and SZ co-caregivers on Caregiving Helplessness. The pairwise comparisons on the Frightened Caregiving subscale revealed that caregivers diagnosed with BP and SZ co-caregivers had significantly higher scores compared to PBCs (Table 3). Finally, there were no significant differences on the Child Caregiving subscale.
Table 3. Experiences of helplessness, fear and child caregiving reported by caregivers with SZ or BP, their co-caregivers and Population-Based Controls (PBC)
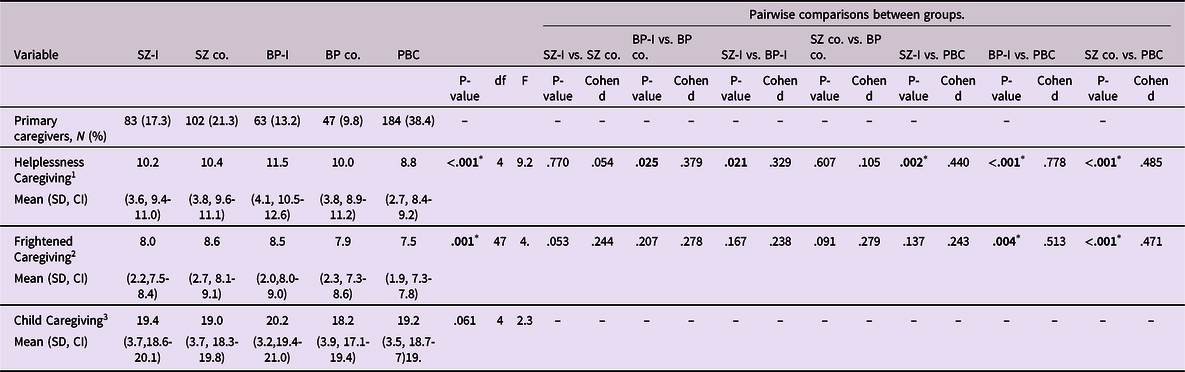
Table 3 statistical analyses: One-way ANOVA and pairwise comparison using Fisher’s Least Significant Difference.
* P < .05 with Bonferroni correction.
1 Scale scores can range from 7 to 35. Higher scores reflect more Caregiving Helplessness.
2 Scale scores can range from 6 to 30. Higher scores reflect more Frightened Caregiving.
3 Scale scores can range from 6 to 30. Higher scores reflect more Child Caregiving (i.e. Role Reversal).
Indicators of disorganized caregiving, level of function and emotional and behavioral problems
Pearson’s correlation analyses showed that higher scores on Helplessness Caregiving were significantly associated with caregivers’ lower level of functioning across all groups (Table 4). Frightened Caregiving were significantly associated with caregivers’ lower level of functioning in the BP combined group. Across all groups higher scores on Helplessness and on Frightened Caregiving were significantly associated with children having a lower level of functioning as well as more externalizing and internalizing behavior problems (measured with the CBCL questionnaire) (Table 4). The associations were not significantly different between the three groups (>.05; data not shown), except for the associations between Frightened Caregiving and children’s internalizing problems (p = .017).
Table 4. Correlations between experiences of helplessness, fear and child caregiving and caregivers’ global level of function (PSP), children’s global level of function (C-GAS) and children’s emotional and behavioral problems/symptoms (CBCL)

*** Correlation is significant at the <.001 level (2-tailed).
** Correlation is significant at the 0.01 level (2-tailed).
* Correlation is significant at the 0.05 level (2-tailed).
1 Scale scores can range from 7 to 35. Higher scores reflect more Caregiving Helplessness.
2 Scale scores can range from 6 to 30. Higher scores reflect more Frightened Caregiving.
3 Scale scores can range from 6 to 30. Higher scores reflect more Child Caregiving (i.e. Role Reversal).
4 Personal and Social Performance Scale (PSP), total score on a 100-point scale, a low score reflects a poor level of function.
5 The Children’s Global Assessment Scale (CGAS). Total score on a 100-point scale, a low score reflects a poor level of function.
6 Child Behavior Checklist school-age version (CBCL). A high score reflects more externalizing behavior problems.
7 Child Behavior Checklist school-age version (CBCL). A high score reflects more internalizing behavior problems.
8 Child Behavior Checklist school-age version (CBCL). A high score reflects more internalizing and/or externalizing behavior problems.
High frightened and high child caregiving—a possible high-risk group
Results showed significant differences between groups on child level of functioning and child behavior problems (p < .001) and caregivers’ level of functioning (p = .001) (Table 5). Pairwise comparisons revealed that caregivers in the combined group (F&CC) and caregivers in the F Only group reported significantly more child behavior problems (both externalizing and internalizing) and the children had lower level of functioning compared to the CC only and the Neither group. Differences between F&CC and F Only were non-significant, except from caregivers in the F Only reporting significantly more child externalizing behavior problems compared to the combined group. Significant between-groups differences in caregivers’ level of function were found between F Only and Neither and between F&CC and Neither.
Table 5. Pairwise comparisons of functional level and dimensional psychopathology in groups caregivers with a high level of both Frightened Caregiving and Child Caregiving
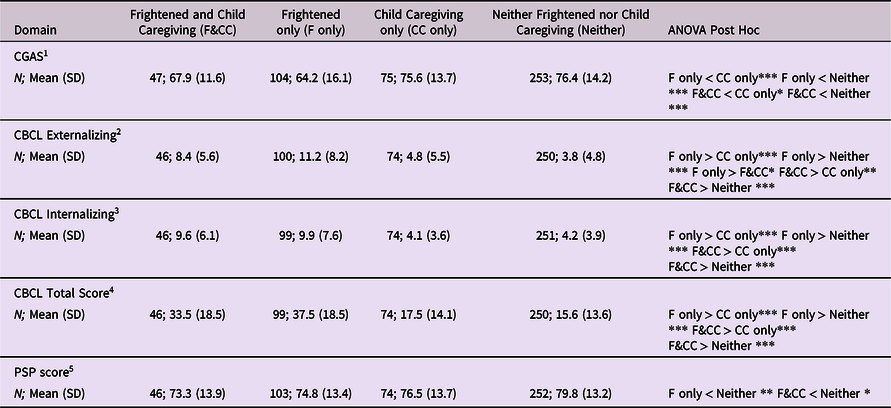
* p < .05.
** p < .01.
*** p < .001.
Table 5 statistical analyses: One-way ANOVA and pairwise comparison using Fisher’s Least Significant Difference. Caregivers belonging to “F&C” scores above the upper quartile on both Frightened Caregiving and Child Caregiving. Caregivers belonging to “F only” scores above upper quartile on Frightened Caregiving and below upper quartile on Child Caregiving. Caregivers belonging to “C only” scores above upper quartile on Child Caregiving and below upper quartile on Frightened Caregiving. Caregivers belonging to “Neither” scores below the upper quartile on both Frightened Caregiving and Child Caregiving.
1 The Children’s Global Assessment Scale (CGAS). Total score on a 100-point scale, a low score reflects a poor level of function.
2 Child Behavior Checklist school-age version (CBCL). A high score reflects more externalizing behavior problems.
3 Child Behavior Checklist school-age version (CBCL). A high score reflects more internalizing behavior problems.
4 Child Behavior Checklist school-age version (CBCL). A high score reflects more internalizing and/or externalizing behavior problems.
5 Personal and Social Performance Scale (PSP), total score on a 100-point scale, a low score reflects a poor level of function.
Discussion
This is the first familial high-risk cohort study using the CHQ to assess indicators of disorganized caregiving in caregivers of seven-year-old children, including both caregivers with SZ or BP and co-caregivers.
Experiences of helplessness and fear in families with parental SZ or BP
We found higher scores on experiences of helplessness and fear among caregivers with SZ or BP as well as their co-caregivers compared to PBC. The SZ combined group (SZ + SZ co-caregiver) and BP combined group (BP + BP co-caregiver) did not differ in their perception of helplessness and fear, which may indicate that it could be a common experience in families with SZ and BP.
Impact of SZ and BP on experiences of helplessness and fear
In the second analysis, a differentiation was made between caregivers directly and indirectly (i.e. co-caregiver) affected by SZ or BP. Caregivers both directly and indirectly affected by SZ or BP reported higher scores on Helplessness compared to PBC. The Helplessness scale is thought to capture a state of mind in which the caregiver perceives the child as out of control and where the caregiver is somehow overwhelmed by the caregiving task, thus leaving the caregiver unable to assume the caregiving role (George & Solomon, Reference George and Solomon2011). It seems understandable, that being diagnosed with a SMI may lead to elevated feelings of being overwhelmed in the caregiving role due to symptoms, medication side effects or lack of energy and executive problems (Nicholson, Sweeney, & Geller, Reference Nicholson, Sweeney and Geller1998; Oyserman et al., Reference Oyserman, Mowbray, Meares and Firminger2000). In a qualitative study, 22 mothers with either SZ, BP or severe depression with psychotic symptoms described the demands associated with caregiving in concert with the demands of coping with a SMI as considerable—for example that it can be difficult to look at the emotional needs of the child when being wrapped up in one’s own emotional need (Diaz-Caneja & Johnson, Reference Diaz-Caneja and Johnson2004). Our hypothesis considering caregivers diagnosed with SZ to report higher levels of disorganized caregiving representation compared to caregivers diagnosed with BP was not conformed as we found the reverse pattern. Further, caregivers diagnosed with BP reported significantly higher levels of Frightened Caregiving compared to PBC; this difference was not shown between caregivers diagnosed with SZ and PBC. Disorganized caregiving representations in caregivers with SZ may be stronger in periods with active psychotic symptoms than in periods with few or no psychotic symptoms, whereas caregiving improves when symptoms decline. This hypothesis can be supported by a study describing that quality of mother–infant interaction improved when maternal psychotic symptoms declined (Snellen et al., Reference Snellen, Mack and Trauer1999), where having a unipolar depression is associated with increased negative-intrusive and hostile behavior, and decreased engaged and positive-sensitive behavior even in the absence of clinical psychiatric symptoms of depression (Lovejoy, Graczyk, O’Hare, & Neuman, Reference Lovejoy, Graczyk, O’Hare and Neuman2000). Our cohort consists of caregivers that at some time point in life had been diagnosed with either SZ or BP and are thus in different phases of the illness. However, participation for the primary caregiver in the VIA 7 study generally required two days at the research unit and one home visit and therefore a certain amount of surplus energy and that the caregiver was not hospitalized. Further, our study is cross-sectional, which is an important limitation since our findings do not exclude that the caregiving situation may had been different for these groups of caregivers measured at a different time—e.g. during active illness symptoms.
To our knowledge this is the first study to investigate indicators of disorganized caregiving with an equal focus on caregivers diagnosed with SZ or BP and their co-caregivers. The additional focus on co-caregivers may further elucidate whether children at FHR-SZ or FHR-BP are at risk of experiencing disorganized caregiving not only from the caregiver diagnosed with a SMI but possibly also from the co-caregiver and therefore may be double exposed to disorganized caregiving. However, this cannot be inferred with certainty from this study as only one caregiver per child provided data on the CHQ. In our study, the SZ co-caregivers reported higher scores on Helplessness and Frightened caregiving compared to PBC, and BP co-caregivers reported higher scores on Helplessness compared to PBC. This may imply, that in a family with at parent diagnosed with SZ or BP, all family members can be influenced by the consequences of the mental disorder, taking time and surplus from other responsibilities and motivational systems (e.g. the caregiving motivational system). This is in line with previous research indicating that both patients and partners struggle with the tremendous impact of SMI on their lives and on their relationships (Granek, Danan, Bersudsky, & Osher, Reference Granek, Danan, Bersudsky and Osher2016; Rose, Reference Rose1996; Shiraishi & Reilly, Reference Shiraishi and Reilly2019). However, it should be noticed that the difference between BP co-caregivers and PBC on Helplessness is not significant after a Bonferroni correction, and should therefore be interpreted with caution. Another point to consider is assortative mating (i.e. the tendency for mated pairs to be more phenotypically similar for a given characteristic than would be expected if they were chosen at random (Merikangas & Spiker, Reference Merikangas and Spiker1982) in individuals with a mental illness. A study concludes that assortative mating is evident in psychiatric populations both within specific disorders and across the spectrum of psychiatric conditions (Nordsletten et al., Reference Nordsletten, Larsson, Crowley, Almqvist, Lichtenstein and Mataix-Cols2016). Such concordance may cause disruption in the caregiving system for both parents with adverse impact on child development.
Indicators of disorganized caregiving, level of function and emotional and behavioral problems
We report that across all three groups (SZ combined group, BP combined group and PBC), experiences of helplessness are correlated with the caregiver’s level of function and this correlation does not differ between the groups. This is in line with research suggesting that mothers’ current symptomatology and level of function play a much larger role in caregiving behavior than having a SMI in itself (Mowbray, Oyserman, & Bybee, Reference Mowbray, Oyserman and Bybee2000). However, the association between level of functioning and experiences of fear was only significant in the BP combined group.
From a theoretical standpoint, the associations found in this study between Helplessness and Frightened Caregiving and child behavior problems (externalizing and internalizing measured by the CBCL) and child level of function are not surprising. Children whose caregivers abdicate care and/or behave in frightened ways are left in a state of emotional and physiological dysregulation without any assistance (Solomon & George, Reference Solomon and George2011). However, cause and effect cannot be inferred, and child characteristics can also affect caregiving behavior (McBride, Schoppe, & Rane, Reference McBride, Schoppe and Rane2002).
We found no between-group differences on the Child Caregiving subscale nor any significant associations with the Child Caregiving subscale. It is possible that measurable differences on Child Caregiving may not surface until the children are older, for example during the self-transformations that are associated with adolescence (Allen, Reference Allen, Cassidy and Shaver2008; George & Solomon, Reference George and Solomon2011). However, our results support the researchers behind the subscale (George & Solomon, Reference George and Solomon2011) and their assertation that the subscale is not sensitive enough to capture this caregiving representation. They suggest that the subscale may be more useful in categorial analyses based on patterns of scores on both Frightened and Child Caregiving.
High scores on frightened caregiving and child caregiving
The exploratory results in the present study show that caregivers high on both Frightened and Child Caregiving were associated with elevated difficulties across all child measures compared to caregivers who were high only on Child Caregiving. Caregivers high on Frightened subscale only were also associated with elevated difficulties across all child measures compared to caregivers who were only high on Child Caregiving subscale. However, this group of caregivers also reported significantly higher externalizing behavior problems in the child compared to caregivers high on both Child Caregiving and Frightened subscale. Similar findings were reported in another study investigating disorganized caregiving representations in diverse, primarily economically disadvantaged women (Huth-Bocks et al., Reference Huth-Bocks, Guyon-Harris, Calvert, Scott and Ahlfs-Dunn2016). Thus, our study does not indicate that the combination of high scores on both Child Caregiving and Frightened constitutes a special risk group, but in this context it is important to take into account the low internal reliability found on these two subscales (F: α = .51 and CC: α = .58) (Tavakol & Dennick, Reference Tavakol and Dennick2011).
Clinical relevance
These results indicate a need for interventions addressing indicators of disorganized caregiving in families where a parent is diagnosed with SZ or BP. More concern for the caregivers’ well-being (e.g. feelings of being overwhelmed or feeling helpless) and functioning is warranted, considering the potential consequences for the children. This pertains to both the caregivers with SZ or BP and their co-caregivers. The indication that experiences of helplessness and fear not illness specific and are related to the caregiver’s level of functioning could make the CHQ and function score low risk and low cost screening tools in families with SZ and BP when identifying whom to support in more optimal caregiving for the potential benefit of both caregiver and child.
In a systematic review of interventions for parents with psychotic or bipolar disorder (Schrank, Moran, Borghi, & Priebe, Reference Schrank, Moran, Borghi and Priebe2015), the authors mention that there was no distinct type of intervention specifically aimed at parents with psychotic or bipolar disorder. They further raise the question if these parents need another type attention compared to any other persons with parenting challenges, and whether such interventions should be placed in the context of mental health services or in a community context. Our study provides important findings regarding this issue, as we find that experiences of helplessness and fear are far more pronounced in families with mental illness compared to PBC. Therefore, this could be targeted as a part of the treatment provided in the mental health services. Based on the results from Danish High Risk and Resilience Study—VIA 7 (Thorup et al., Reference Thorup, Jepsen, Ellersgaard, Burton, Christiani, Hemager, Skjærbæk, Ranning, Spang and Gantriis2015), a randomized controlled trial—the VIA Family (Müller et al., Reference Müller, Gjøde, Eigil, Busck, Bonne, Nordentoft and Thorup2019) —has been conducted. Families with SMI are offered an early, preventive, cross-sectoral and integrated intervention which (among many other areas), focuses on improving parenting competences by providing support from Triple P (Positive Parenting Program REF) (Sanders, Kirby, Tellegen, & Day, Reference Sanders, Kirby, Tellegen and Day2014). By supporting the parents in providing warm, responsive and sensitive caregiving and by increasing their mentalization skills, the risk of disorganized caregiving will most likely be reduced. Programs are also developed for younger children, for example in the VIPP program (Video Informed Positive Parenting) (Juffer, Bakermans-Kranenburg, & van IJzendoorn, Reference Juffer, Bakermans-Kranenburg and van IJzendoorn2017).
Strengths and limitations
The strengths of this prospective cohort study include a large sample size and the use of Danish national registers to recruit the families, which contributes to the representativity of the study. The narrow age range of the children is a strength of the study too. Data from this age range contributes to the current knowledge about indicators of disorganized caregiving when influences from having a SMI coincide with the requirements for caregiving of a seven-year-old child, including school start and other increased social demands. The use of CHQ has proven useful as a screening tool for disorganized caregiving for parents having children at different ages (George & Solomon, Reference George and Solomon2011; Huth-Bocks et al., Reference Huth-Bocks, Guyon-Harris, Calvert, Scott and Ahlfs-Dunn2016). The study had a high participation rate and it was not necessary to exclude any questionnaires due to inadequate completion. Another strength of the study is the inclusion of caregivers with SZ and caregivers with BP and co-caregivers in the same study, which allowed for exploration of possible illness-specific group differences.
This study also has some limitations. When the caregivers were split into four groups, group sizes became small, which can reduce statistical power and increase the likelihood of type 1 and 2 errors. Further, our inclusion criteria required that the index caregiver at some point in life had been diagnosed with either SZ or BP. Some of the index caregivers could be in full remission from their mental illness and have been so throughout the child’s upbringing, while others still experienced symptoms. Our analysis indicates that a lifetime history of SZ or BP affects experiences of helplessness and fear in the role as a caregiver, and it could be relevant to further differentiate between illness severity within the groups. It is a limitation that we only have data in current daily function of the parents, and not on psychopathology, and results should be considered with this in mind, that level of psychopathology at the time of testing varied between families. It is conceivable based on the literature that high scores on a given subscale primarily come from those who still experience symptoms. On the other hand, we know that mental illness also affects cognition and emotion regulation also in periods when symptoms are not pervasive (MacQueen, Young, & Joffe, Reference MacQueen, Young and Joffe2001; McCutcheon, Marques, & Howes, Reference McCutcheon, Marques and Howes2020) and even prior to illness onset (Reichenberg et al., Reference Reichenberg and Caspi2010).
CHQ as a self-report measure examines conscious perceptions and may therefore be prone to social desirability bias. Some of the constructs in CHQ may be partly unconscious and therefore better captured through interview-based measures.
Conclusion
The current study investigated indicators of disorganized caregiving among caregivers with a history of SZ or BP and their co-caregivers. Having a history of SZ or BP or being their co-caregiver were associated with higher scores on experiences of helplessness and fear in the child–caregiver relationship compared to a control group. Higher scores on helplessness were associated with lower level of functioning in both caregivers and children as well as more child externalizing and internalizing behavior problems. Higher scores on fear were associated with more child externalizing and internalizing behavior problems, lower level of functioning in children, and lower level of functioning in caregivers with BP. These findings support the need for an intervention addressing indicators of disorganized caregiving in families with SZ or BP.
Acknowledgements
We thank all the children and families who participated in VIA 7 study. We thank Carsten Bøcker Pedersen and Marianne Giørtz Pedersen for assistance with data extraction from the Danish Registers, Manon Chaine for assistance with data management, Preben Bo Mortensen, Thomas Werge, David Hougaard, and Anders Børglum for collaboration in iPSYCH, and Mette Skjærbæk, Anne Ranning, Heidi Jensen, Cecilie Gregersen, Kate Kold Zahle, Maria Toft Henriksen, Henriette Brockdorff Stadsgaard for assisting the data collection.
Funding statement
This work was supported by the Mental Health Services of the Capital Region of Denmark, Aarhus University (Grant No. J.NR 11531), and the Lundbeck Foundation Initiative for Integrative Psychiatric Research (Grant Nos. R102-A9118 and R155- 2014-1724).
Conflicts of interest
None








