Introduction: “If Living Were a Thing That Money Could Buy”
Imagine for a moment a series of disasters that kills more than 800 women every day for a year: the equivalent of two or three daily crashes of crowded long-distance airliners or the equivalent of the direct death toll from the attack on the World Trade Center and the Pentagon every four days. There is little question that such a situation would quickly be regarded as a humanitarian emergency, as the stuff of headlines, especially if ways of preventing the events were well known and widely practiced (as is the case with avoiding crashes in civil aviation). However, remarkably little attention is paid outside the global health and human rights domains to complications of pregnancy and childbirth that kill more than 300,000 women every year – a cause of death now almost unheard of in high-income countries (HICs), although this would not have been the case a century ago. A Canadian woman’s lifetime risk of dying from complications of pregnancy or childbirth is 1 in 8,800 for a woman in Sub-Saharan Africa, the world’s poorest region, it is 1 in 37 (World Health Organization et al., 2019).
This is one example among many of the health contrasts between rich and poor worlds. Average life expectancy at birth (LEB) worldwide has been estimated at 28.5 years in 1800, much of the short average lifespan caused by high rates of death in the early years of life. By the end of the twentieth century, worldwide average LEB had increased to roughly 67 years (Reference RileyRiley, 2005), due in large measure to reductions in infant and child mortality. However, global progress conceals large variations between countries. For example, Canadians born today can expect to live to the age of 82, a figure that is among the world’s highest. In the world’s least-developed countries, as classified by the United Nations, where nearly a billion of the world’s people live, estimated LEB averages 64 years (World Bank, 2017).Footnote 1
Differences in the prevalence of specific diseases are even more dramatic. Although the acquired immune deficiency syndrome (AIDS) was first identified in HICs, more than 95% of new HIV infections now occur outside those countries, with the highest prevalence rates in Sub-Saharan Africa, accounting for more than two-thirds of the world’s infected population and an estimated 660,000 of the estimated 940,000 annual deaths from AIDS (UNAIDS, 2018a). Importantly, the number of AIDS-related deaths has declined sharply from a high of approximately 2 million in 2005 because of the rapid increase in access to antiretroviral therapy (discussed later in this chapter), but a slow decline in the number of new infections means that the number of people living with human immunodeficiency virus (HIV) worldwide continues to rise. Malaria and tuberculosis have been almost entirely vanquished in HICs. Elsewhere in the world, malaria kills an estimated 435,000 people per year and tuberculosis 1.6 million (World Health Organization [WHO], 2018, 2019), despite the demonstrated effectiveness of relatively low-cost solutions.Footnote 2 Health disparities between rich and poor countries involve not only differences in the kinds of illnesses that affect their populations but also the ages at which illness and death occur. Of the estimated 5.4 million deaths of children age five years or under that occurred worldwide in 2017, just 60,000 occurred in HICs, but 2.75 million occurred in Sub-Saharan Africa (GBD 2017 Mortality Collaborators, 2018). And although the worldwide risk of child death declined steadily through the last decades of the twentieth century, far more substantial gains could have been achieved because it has long been recognized that most child deaths outside the high-income world result from causes that are either extremely uncommon in those countries or rarely result in death there (Reference Hug, Sharrow and YouHug, Sharrow, & You, 2017)
Deprivation and Economic Gradients
The intuitive and largely accurate explanation for many of these differences involves poverty and material deprivation. An estimated 897 million people worldwide in 2012 were living on US$1.90 a day or lessFootnote 3 on the World Bank’s contentious definition of extreme poverty (World Bank & International Monetary Fund [IMF], 2016: 29–35). More than 800 million people worldwide were undernourished in 2016, reversing a long-standing if gradual decline according to the United Nations Food and Agriculture Organization (FAO et al., 2017). These are risibly inadequate indicators of the prevalence of material deprivation with consequences for health. “In Zambia, for example, a person on the poverty line can afford a daily diet of two–three plates of nshima (a maize staple known as mealie meal), a sweet potato, a few spoonfuls of oil, a couple of teaspoons of sugar, a handful of peanuts and twice a week, a banana or mango and a small serving of meat. Such a person would have just 28% of his budget left over for other things,” including of course such basics as housing (The Economist, 2016). The FAO undernourishment figures capture only continuous insufficiency of caloric intake over a period of at least a year. Thus, on more realistic indicators, material deprivation is far more widespread than the World Bank and other international agencies acknowledge in their optimistic self-reports (Reference HickelHickel, 2016; Reference Reddy and LahotiReddy & Lahoti, 2016).
Economic deprivation creates situations in which the daily routines of living are themselves hazardous. Charcoal, crop residue, and dung smoke from cooking fires are major contributors to respiratory disease among the world’s poor, mainly in rural areas (Reference Perez-Padilla, Schilmann and Riojas-RodriguezPerez-Padilla, Schilmann, & Riojas-Rodriguez, 2010). In the fast-growing cities of the developing world, almost 900 million people were estimated to live in slums, as defined by UN Habitat, in 2014 – a number that was projected to rise to 2 billion by 2030, with associated exposure to multiple hazardous living and working conditions (Reference Ezeh, Oyebode and SatterthwaiteEzeh et al., 2017). Lack of access to clean water, for example, is a major contributor to infectious diarrhea and a variety of parasitic diseases (Reference Prüss-Ustün, Bartram and ClasenPrüss-Ustün et al., 2014), yet an estimated 660 million people lack access to clean water, and 2.4 billion people have no access to basic sanitation (UNICEF & World Health Organization [WHO], 2015); it is, of course, primarily the poorest people and regions in the countries in question that continue to lack access (WHO & UNICEF, 2017). A further dimension of the role of material deprivation involves the lack of resources to access healthcare. At the individual level, the need to pay for healthcare and the loss of livelihoods associated with illness push an estimated 150 million people into poverty every year (WHO, 2010) – a problem that historically was often worsened by health sector “reforms” actively promoted by HICs through such agencies as the World Bank (Reference Lister, Labonté and LabontéLister & Labonté, 2009; Reference Stubbs, Kentikelenis, Stuckler, McKee and KingStubbs et al., 2017; Reference YatesYates, 2009).Footnote 4
In many respects, then, the words of the folk song “All My Trials” (made famous by Joan Baez) ring true: living is a thing that money can buy; the rich do live, and the poor do die, much earlier and from different causes. In addition to differences among countries, socioeconomic gradients in health status – inverse correlations between health status and various indicators of socioeconomic status – are almost universal within national and subnational boundaries, in countries rich and poor alike. Figure 1.1 shows such gradients in mortality among children under age five (U5MR): children in the poorest fifth of the population in six largely dissimilar low- and middle-income countries (LMICs) are at least twice as likely to die before their fifth birthday, and sometimes three times as likely, as children in the richest fifth. In India alone, a WHO commission estimated in 2008 that 1.4 million child deaths would be prevented each year if the U5MR for the entire Indian population were reduced to the level characteristic of its richest quintile (Commission on Social Determinants of Health, 2008: 29).
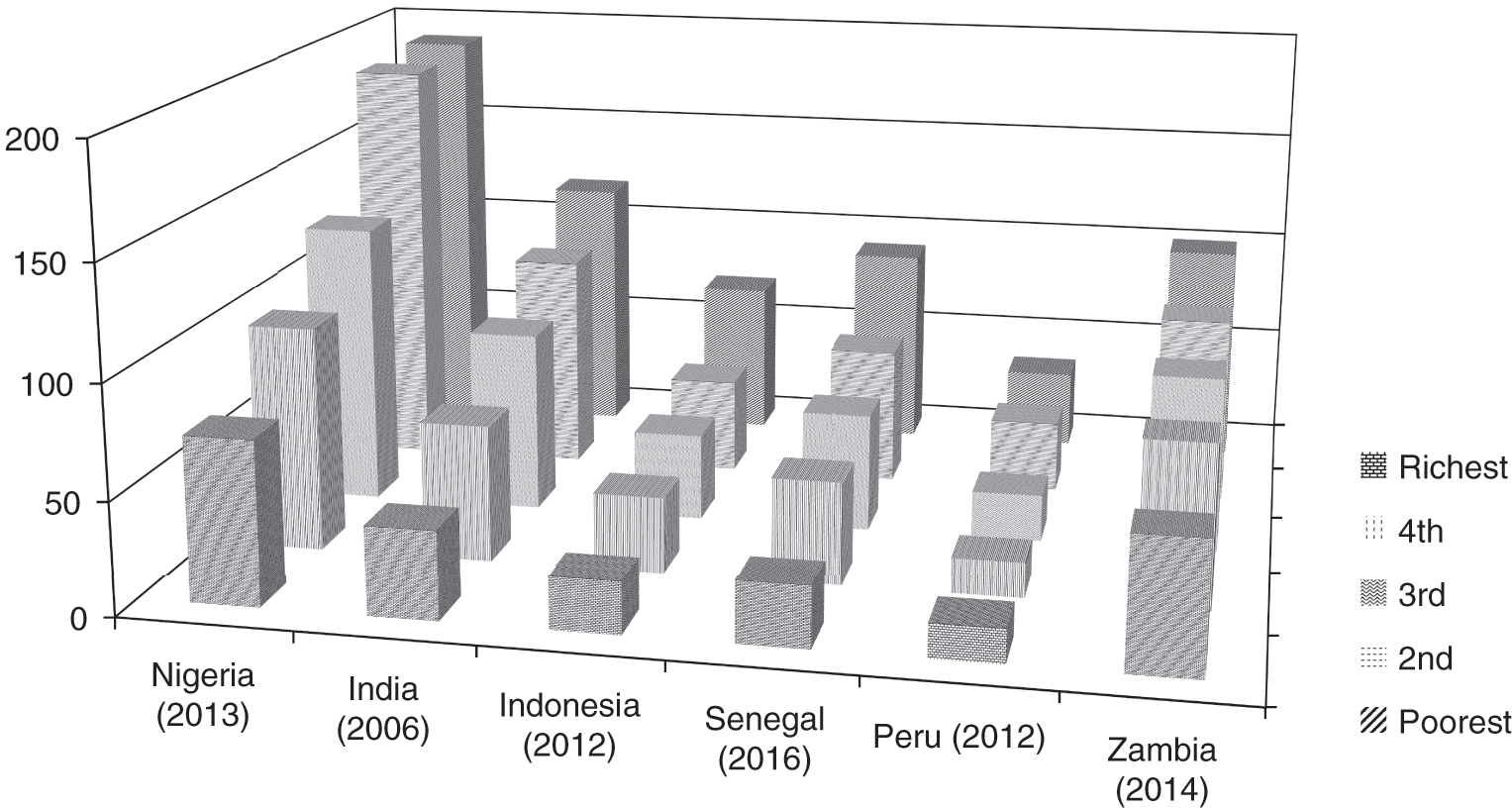
Figure 1.1 Gradient in under-five mortality rate (U5MR), by income quintile, selected LMICs
Socioeconomic gradients reflect not only daily conditions of life and work but also economic influences on access to health services. For example, socioeconomic gradients are pronounced in access to key health system interventions such as antenatal care and attendance by skilled health personnel at birth that improve maternal, newborn, and child health (WHO, 2015b). Importantly, “world scale” socioeconomic gradients in health are widespread in HICs as well. The Eight Americas Study in the USA, where racial and economic inequalities tend to be superimposed on one another, found that the life expectancy of African Americans in “high risk” urban counties was almost nine years shorter than that of the mostly white residents of Middle America (Reference Murray, Kulkarni and MichaudMurray et al., 2006). In the words of the authors, “tens of millions of Americans are experiencing levels of health that are more typical of middle-income or low-income developing countries” (Reference Murray, Kulkarni and MichaudMurray et al., 2006: 9). A decade later, Reference Shaefer, Wu and EdinShaefer, Wu, & Edin (2017) pointed out that African-American men with limited education had a life expectancy at birth in 2008 comparable with the national averages for Pakistan, Bhutan, and Mongolia; the infant mortality rate among African Americans in 2011 was higher than the national averages for Tonga and Grenada; and high-poverty US cities had a homicide rate that made them almost as dangerous as Colombia and Brazil. And circa 2015, the difference in male LEB between the most and least economically deprived wards of the small English postindustrial city of Stockton-on-Tees, where one of us (TS) lived and worked until recently, was larger than the difference in national average male life expectancy between the United Kingdom and Tanzania (Reference SchreckerSchrecker, 2018).
Growth (and Wealth) Are Not Enough
Discussions of global health ethics must avoid the simplistic leap from this set of observations to the conclusion that greater wealth through economic growth is the surest route to better health – and, therefore, that improvements in population health are best achieved by policies that promote economic growth. Superficial support for the growth → wealth → health causal pathway comes from a widely cited graph known as the Preston curve, after the demographer who first drew it. Figure 1.2 shows the Preston curves for the years 2015 and 1960. The graph represents most of the world’s countries with a circle, the area of which is proportional to the size of the country’s population. The vertical axis shows average life expectancy at birth, and the horizontal axis shows the country’s gross domestic product (GDP) per capita, adjusted for purchasing power. The dotted trend lines on the graph show the national average life expectancy that would be anticipated at a given level of GDP per capita based on a population-weighted average of all the national data. The graph shows strong returns to economic growth in terms of LEB at low per capita incomes, up to about US$7.40 per day, which is seen by many as the minimum level at which one could not be considered materially very poor (Reference Labonté and RuckertLabonté & Ruckert, 2019: 149–150). Above that point, a weaker but still positive relation between LEB and per capita income is evident.Footnote 5
Wide variations exist in LEB among countries with comparable GDP per capita figures, which are not fully evident in this version of the graph. For example, in 2016, LEB in the USA, with a GDP per capita of $59,531, was 79 years, but it was 80 years in Chile and Costa Rica, countries with GDP per capita levels of $24,635 and $17,073, respectively (in 2017, again after adjustment for purchasing power). Conversely, some countries do far less well in terms of LEB than one might expect given their income levels. The United States in fact is one of these underperformers, quite probably because of a continuing failure to provide access to healthcare to millions of its people (Reference Barnett and BerchickBarnett & Berchick, 2017) and an emerging epidemic of “deaths of despair” among a subpopulation trapped by stagnating economic prospects (Reference Case and DeatonCase & Deaton, 2017). Indeed, one of Preston’s original conclusions was that “[f]actors exogenous to a country’s level of income probably account for 75%–90% of the growth in life expectancy for the world as a whole between the 1930s and the 1960s. Income growth per se accounts for only 10%–25%” (Reference PrestonPreston, 2007: 486; original publication 1975). In the recent past, the most conspicuous outliers in this respect were countries in Sub-Saharan Africa, where life expectancy was drastically reduced by the AIDS epidemic (see Figure 1.3 and a version of the Preston curve for the year 2000 in Reference DeatonDeaton [2003: 116]).
Two sets of factors are relevant to explaining such variations. The first set comprises advances in medical treatment and preventive health measures such as antibiotics, immunization, and antiretroviral therapy for HIV/AIDS. The upward movement of the dotted trend line in the Preston curve over time can be thought of as the treatment and prevention dividend, examples of which are cited in this chapter’s concluding section. The second set of factors involves the extent to which countries use their available resources in ways that result in widely shared improvements in health status for their populations – including access to advances in treatment and prevention. The underperformance of the United States has already been noted. Conversely, Sri Lanka, Costa Rica, and the Indian state of Kerala are often cited as overperformers in population health status despite low GDP per capita, attributed to their attention to accessible primary healthcare and other social protection measures – what Reference RileyRiley (2008) refers to as “social growth” (see also Reference Balabanova, Mills and ContehBalabanova et al., 2013).
Based on such examples, Angus Reference DeatonDeaton (2006: 3), who was later to win a Nobel Prize in economics, concluded: “Economic growth is much to be desired because it relieves the grinding material poverty of much of the world’s population. But economic growth, by itself, will not be enough to improve population health, at least in any acceptable time…. As far as health is concerned, the market, by itself, is not a substitute for collective action.” This collective action pertains not only to the second set of factors (how countries allocate resource priorities and distribution) but also to the first set of factors (publicly financed or supported innovations in health knowledge, technology, and global diffusion). Deaton points out that most health innovations that contributed to the global convergence in health in the last half of the last century, which has now been replaced by divergence (Reference Moser, Shkolnikov, Leon, Caraël and GlynnMoser, Shkolnikov, & Leon, 2007), originated in wealthier countries. “In this sense, the first world has been responsible for producing the global public goods of medical and health-related research and development from which everyone has benefited, in poor and now-rich countries alike” (Reference DeatonDeaton, 2004: 99). In the last 20 years, however, companies in HICs have led a push for worldwide expansion of intellectual property protection, notably in knowledge-based industries such as information technology and pharmaceuticals. This has led to the emergence of one of the most contentious issues in contemporary global health: that of access to essential medicines and other health technologies (Reference Muzaka, Brown, Yamey and WamalaMuzaka, 2014). There is also the vexing, more basic question of whether such a profit-driven regime of innovation priorities can effectively support research into diseases that afflict mainly people who are too poor to represent a commercially attractive market (Reference Pedrique, Strub-Wourgaft and SomePedrique et al., 2013).
How Health Risks Are Distributed
A further complication of the relation between economic growth and health involves how growth influences the nature and distribution of risks to health. It was once argued that countries experienced a relatively standardized epidemiological transition as they grew richer, in which infectious or communicable diseases (disproportionately affecting children) declined while chronic diseases (disproportionately affecting adults) increased (Reference OmranOmran, 1971). Although still useful, the concept only partially captures a pattern in which LMICs are increasingly affected by a “double burden of disease,” as persistent or resurgent communicable diseases coexist with rapid increases in noncommunicable diseases such as cardiovascular disease, diabetes, and cancer (see Reference Agyei-Mensah and de-Graft AikinsAgyei-Mensah & de-Graft Aikins, [2010] for an important case study). Figure 1.4 shows that the age-adjusted death rates from such noncommunicable diseases as cardiovascular diseases and cancer in LMICs in some regions are actually higher than in the high-income world, although their proportional contribution to mortality in some regions is lower because of the toll taken by other causes of death.
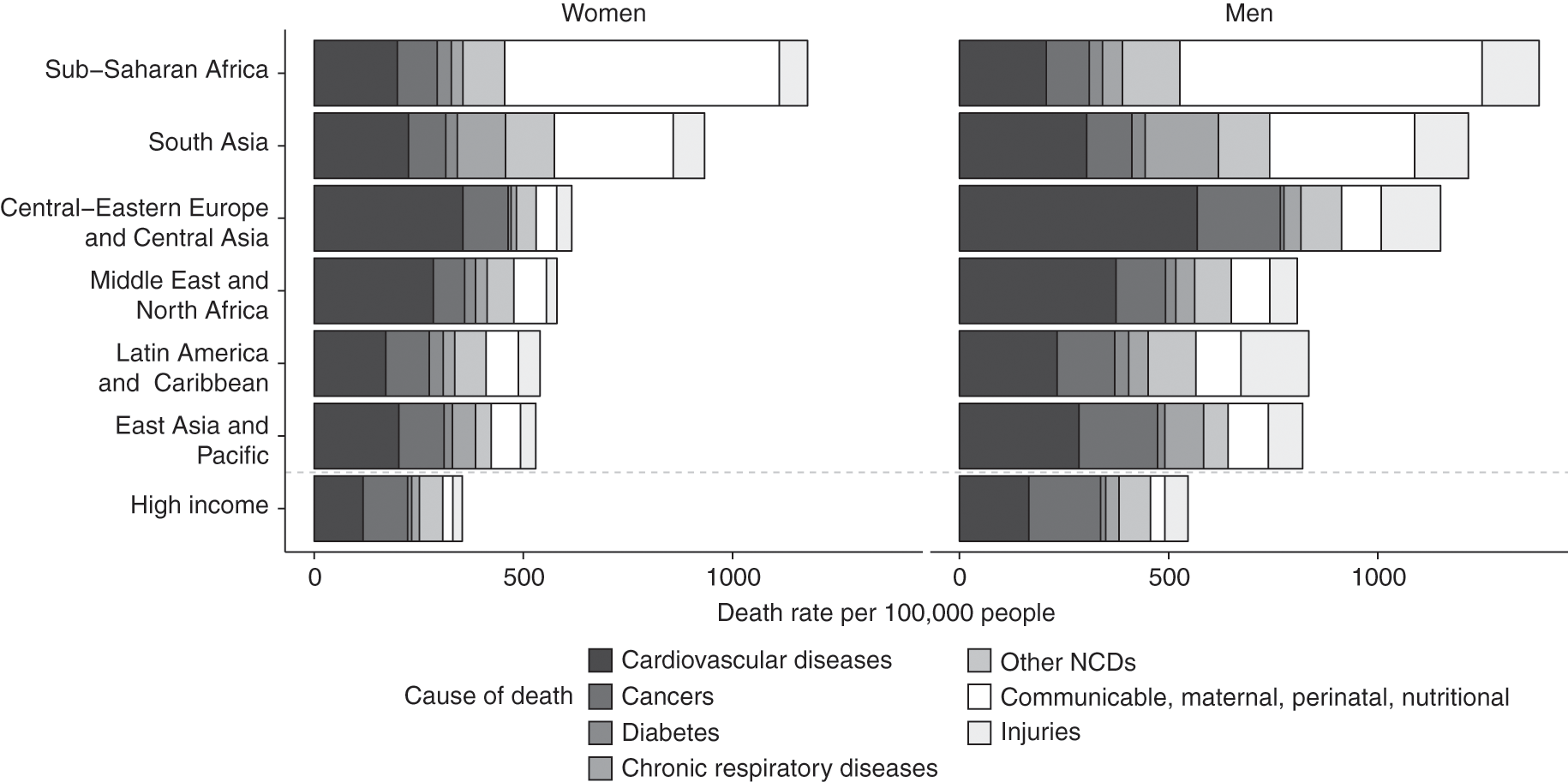
Figure 1.4 Age-adjusted death rates from various causes, 2010
It was estimated at the start of this century that 100 million men in China alone would die from smoking-related diseases between 2000 and 2050 (Reference Zhang and CaiZhang & Cai, 2003). Additionally, road traffic accidents kill an estimated 1.2 million people a year, disproportionately in LMICs (WHO, 2015a). Ironically, those most likely to be injured are the poor, who are least likely to own a vehicle – a distribution of risks that is sometimes exacerbated by planning practices that favour high-speed roads for the emerging middle classes. In many cases, additional hazards are associated with exposures to industrial or motor vehicle pollution and dangers in the industrial or agricultural workplace. In a standard text on global health, Reference Birn, Pillay and HoltzBirn, Pillay, & Holtz (2017: 231–284) have suggested that it may be useful to replace the familiar categories of communicable and noncommunicable diseases with a threefold typology: diseases of marginalization and deprivation, such as diarrhea, neglected tropical diseases, malaria, and respiratory infections; diseases of modernization and work, such as cardiovascular disease, cancer, and road traffic injuries; and diseases of marginalization and modernization, such as diabetes, chronic obstructive pulmonary disease (COPD), tuberculosis, and HIV/ AIDS. Socioeconomic gradients are observable with respect to all three categories of disease, including those widely if mistakenly regarded as “diseases of affluence” (Reference Ezzati, Vander Hoorn and LawesEzzati et al., 2005).
The significance of the double burden of disease concept is illustrated by the coexistence of undernutrition with rapid growth of overweight and obesity in LMICs – indeed, in some instances, of undernutrition and overweight in the same household (Reference Black, Victora and WalkerBlack et al., 2013). Reflecting a nutrition transition involving a rapid shift to diets higher in ultraprocessed foods (Reference Monteiro, Moubarac, Cannon, Ng and PopkinMonteiro et al., 2013) coupled with reductions in physical activity, overweight and obesity in several middle-income countries are approaching the levels seen in countries such as the USA. An especially striking study involves a sample of women in regions that account for more than 70% of Brazil’s population. In 1975, almost twice as many Brazilian women were underweight as were obese; by 1997, the proportions had reversed, with the increases in obesity concentrated among low-income women (Reference Monteiro, Conde and PopkinMonteiro, Conde, & Popkin, 2004; see also Reference Mendez, Monteiro and PopkinMendez, Monteiro, & Popkin, 2005). The emergence of this socioeconomic gradient is a broader trend once a certain income threshold is passed (Reference Malik, Willett and HuMalik, Willett, & Hu, 2013), and the connection with aggressive marketing of ultraprocessed foods appears to be worldwide (Reference Baraldi, Martinez Steele, Canella and MonteiroBaraldi et al., 2018; Reference Louzada, Ricardo, Steele, Levy, Cannon and MonteiroLouzada et al., 2018; Reference Martínez Steele, Popkin, Swinburn and MonteiroMartínez Steele et al., 2017; Reference Monteiro, Moubarac and LevyMonteiro et al., 2018; Reference Moodie, Stuckler and MonteiroMoodie et al., 2013). Further, the prevalence of overweight and obesity in many cases is increasing far more rapidly than it did in the HICs decades earlier (Reference PopkinPopkin, 2006), setting the stage for increases in cardiovascular disease and diabetes that will widen existing health disparities and challenge the ability of health systems to respond.
Globalization, Markets, and Health in an Unequal World
Globalization, defined here as “[a] pattern of transnational economic integration animated by the ideal of creating self-regulating global markets for goods, services, capital, technology, and skills” (Reference Eyoh, Sandbrook, Kohli, Moon and SørensenEyoh & Sandbrook, 2003: 252), presents broader challenges as well. Perhaps most fundamentally, as the editor of Le Monde Diplomatique has put it, globalization is an “inequality machine [that] is reshaping the planet” (Reference HalimiHalimi, 2013), as bidding wars of all kinds become transnational in scope. As just two examples, production is now organized in commodity chains that routinely cross multiple national borders, with the hunt for lower-cost labor – facilitated by a legal infrastructure of trade and investment agreements and dramatic reductions in the cost of transport and communication – being a major driver of that organizational pattern. Conversely, “the prime resources of the city are increasingly appropriated by the affluent. And globalization is inflationary as the new rich are able to pay more for a range of key goods, especially land” (United Nations Human Settlements Programme, 2003: 52) – hence such paradoxes as Luanda, the capital city of oil-rich Angola, where poverty is endemic, appearing in some league tables as the most expensive city in the world (Reference NgugiNgugi, 2017). One can find graphic illustrations of many such metropolitan juxtapositions of wealth and poverty in Johnny Miller’s remarkable aerial photographs (www.unequalscenes.com).
The academic literature suggests that while inequality among countries may be decreasing, notably because of rapid growth in some emerging economies, within-country economic inequality is increasing, sometimes rapidly, as is the worldwide concentration of wealth at the pinnacle of the global distribution (Reference MilanovicMilanovic, 2016; Reference ZucmanZucman, 2019). In a synthesis of evidence drawing mainly on the Forbes billionaires list and on research for Swiss wealth manager Credit Suisse (Reference Shorrocks, Davies and LluberasShorrocks, Davies, & Lluberas, 2018), Oxfam International notes that “in 2017, 43 billionaires held as much wealth as the bottom 50% of the world population; in 2018, this figure decreased to 26 billionaires” (Reference Revollo, Mariotti, Mager and JacobsRevollo et al., 2019: 7). Further, the (predivorce) wealth of one person, Amazon founder Jeff Bezos, circa 2018 amounted to 100 times the total annual health budget of Ethiopia, Africa’s second-largest country and as of 2019 one of the least-developed countries (LDCs) as ranked by the United Nations (Reference Revollo, Mariotti, Mager and JacobsRevollo et al., 2019: 5). Such comparisons actually understate the extent of concentration because “there are many more individuals who own $5 million, $20 million, or $100 million than there are billionaires, and the former command a potentially much larger fraction of world wealth than the latter” (Reference ZucmanZucman, 2019: 22). Such figures must be viewed against a background of minimal progress, outside China, in reducing the number of people living in extreme poverty after 1990 on the World Bank’s definition (The Economist, 2016), during a period in which the inflation-adjusted value of the world’s economic product more than doubled.
Why does this matter for global health justice? An accumulating body of evidence – so far largely from the high-income world, where data are more abundant and reliable – indicates that high levels of inequality increase the prevalence of adverse health outcomes and a variety of other social problems across an entire jurisdiction (county, metropolitan area, or country): the Spirit Level argument (Reference Wilkinson and PickettWilkinson & Pickett, 2010; for an updated review of extensive additional evidence, see Reference Pickett and WilkinsonPickett & Wilkinson, 2015). This evidence is, of course, far from convincing in political terms because rising inequality means that the wealthy are increasingly able to isolate themselves from problems outside their epidemiologic worlds, living in gated communities; paying privately for almost all services, including security; and in the extreme, commuting by helicopter and completely avoiding ground-level transit (Reference PhillipsPhillips, 2008). Concentration of income and wealth is likely to translate into concentration of political influence; an expanding body of recent political science research corroborates the conclusion of earlier analyses ranging across a spectrum from mainstream to Marxist that policymakers disproportionately respond to the preferences of the rich, even under conditions of formal democracy (Reference BartelsBartels, 2004, Reference Bartels2017; Reference GilensGilens, 2012; Reference Page and BartelsPage & Bartels, 2013), conditions that are increasingly under siege (Freedom House, 2018).
Conclusion and Prospects for the Future: Money and Power Matter
It can always be argued that the longer-term benefits of integration into the global marketplace have yet to materialize; growth should eventually generate resources to improve health for all. Whereas growth may of course do so, recall Deaton’s skepticism about what might be called the waiting for Godot approach to population health. This approach was articulated with unusual frankness by a team of World Bank economists writing about the former Soviet Union and its Eastern European satellites: “In the long run, the transition towards a market economy and adoption of democratic forms of government should ultimately lead to improvements in health status…. In the short run, however, one could expect that health status would deteriorate” (Reference Adeyi, Chellaraj, Goldstein, Preker and RingoldAdeyi et al., 1997: 133). Anticipation of long-term gains is better understood as an expression of faith than as an evidence-based assessment. Nobel Prize–winning economist Joseph Stiglitz, formerly of the World Bank, has described the consequences of the post-1980 promotion of a particular market-focused vision of globalization by the governments of major G7 powers, acting on their own and through multilateral institutions such as the World Bank and the IMF, as “a lost quarter-century in Africa, a lost decade in Latin America, and a transition from communism to the market economy in the former Soviet Union and eastern Europe that was, to say the least, a disappointment” (Reference StiglitzStiglitz, 2016). This point is especially important because of philosopher Thomas Pogge’s complex and nuanced argument (1) that a basic “negative obligation” exists to avoid doing harm and that obligation extends across national borders, (2) that the contemporary global economic order systematically neglects that obligation, and (3) that the neglect is avoidable; it is not difficult to envision alternative sets of economic and political institutions and underlying distributions of power that would not demand long periods of pain and widespread persistence of ill-health in anticipation of health gains at some indeterminate point in the future (Reference PoggePogge, 2001, Reference Pogge, Anand, Peter and Sen2004, Reference Pogge and Pogge2007).
More immediately, rising inequality and wealth concentration have important implications for progress toward such objectives as universal health coverage (UHC) – a target of the United Nations’ Sustainable Development Goals (SDGs) and a programmatic priority of the WHO, although uncertainty remains about how UHC will be interpreted with respect to the mix of public/private provision and financing (Reference SenguptaSengupta, 2013). The most fine-grained estimate of the cost of achieving this target available at the time of writing is that an “ambitious” scenario would require additional spending of US$134 billion (at 2014 currency values) initially, rising to US$371 billion in 2026–2030 (Reference Stenberg, Hanssen and EdejerStenberg et al., 2017). Many middle-income countries could mobilize these resources domestically, but substantial and sustained external assistance would be required in the case of many low-income countries (Reference SachsSachs, 2012). Even low-income countries have substantial opportunities to expand health spending that are arithmetically, if not politically, feasible (Reference McIntyre, Meheus and RøttingenMcIntyre, Meheus, & Røttingen, 2017; Reference Meheus and McIntyreMeheus & McIntyre, 2017). Increasing inequality is likely to complicate these questions of political feasibility, as is the ability of the wealthy to avoid taxation by shifting resources to tax havens (Reference HarringtonHarrington, 2016) – a topic that merits a chapter of its own (Reference Brock, Benatar and BrockBrock, 2011). The global arithmetic is that an annual levy of 0.5% on the wealth of the richest 1% would suffice to finance this level of expenditure (Reference Revollo, Mariotti, Mager and JacobsRevollo et al., 2019: 18–19). Indeed, a global financial transaction tax of 0.05% on all currency exchanges (including speculative “shadow banking” and derivative markets) is estimated to be sufficient to fund implementation of all 17 SDGs and their 169 targets (Reference Labonté and RuckertLabonté & Ruckert, 2019: 396).
Despite the uncertainties created by globalization, many efforts to improve the health status of people outside the metaphorical castle walls have succeeded in recent years. The drop in measles mortality is one of the great global health success stories (Reference Perry, Gacic-Dobo and DabbaghPerry et al., 2014), and crucially, the number of people living with HIV/AIDS who are receiving antiretroviral therapy increased from fewer than 1 million at the turn of the millennium to more than 20 million in 2017 (UNAIDS, 2018b) – still far from universal access, and the bitterly contested political economy of this transition again would merit a chapter of its own (but see Reference ‘t Hoen, Berger, Calmy and Moon‘t Hoen et al., 2011; UNAIDS, 2015: 78–95). Such success stories depended on effective and sustained mobilization of financial and other resources, both domestically and internationally. They are also consistent with a biomedical perspective shaped by experience with communicable diseases, a necessary condition for which is exposure to a particular pathogen; the complexities of dealing with a rising burden of noncommunicable diseases, which may have multiple sufficient causes, are conceptually more challenging for many health professionals quite apart from the politics of mobilizing an expanding quantum of resources and, more fundamentally, addressing the “power asymmetries” (Reference Ottersen, Dasgupta and BlouinOttersen et al., 2014: 631) that generate and perpetuate health inequalities on multiple scales. The global reach of transnational corporate promotion of ultraprocessed foods is just one example among many. Moreover, as the 2015 Lancet Commission on Planetary Health noted, aggregate human health has been improving (if inequitably so) at the same time as our ecological boundaries that support life are being broached. The stark conclusion was that “we have been mortgaging the health of future generations to realise economic and development gains in the present” (Reference Whitmee, Haines and BeyrerWhitmee et al., 2015: 1973).
We make two points by way of conclusion. First, money matters, and global health ethics must start from the position that rhetoric is no substitute for commitments of resources to protect health on a much larger scale than at present. This can serve as a point of agreement even among researchers and practitioners who disagree about the relative value of improving social determinants of health and those who emphasize the “upstream” social determinants of health, usually with a focus on poverty and economic inequality, and those who dismiss interventions to address these factors as “romantic but impracticable notions” (Reference Jha, Brown, Nagelkerke, Slutsky and JamisonJha et al., 2005: 1539), arguing instead for a focus on biomedical innovations and scaling up health systems. In fact, all of these are necessary, with the relative importance depending on context. No investment in health systems will undo the damage caused by indoor air pollution from cooking smoke, and health systems are only one among many influences on the incidence of HIV infection; no investment in social determinants of health will substitute for effective immunization programs or antiretroviral therapies; and neither problem can be addressed without real resources.
Second, in today’s global environment, a preoccupation with setting priorities in resource-poor settings is a diversion or worse (Reference SchreckerSchrecker, 2013). The questions of far greater importance, as suggested by the work of Pogge and many others, is why some settings are resource poor and others not, and how to change that. The fact that resource scarcities condemn millions every year to premature and avoidable deaths and millions more to shorter and less healthy lives than most readers of this volume take for granted must be understood as policy-generated, resulting from particular power asymmetries, choices that could have been made differently, and institutions that can function differently. “If living were a thing that money could buy,” indeed.
Acknowledgment
Research for the original version of this chapter was partially supported by the Canadian Institutes of Health (Research Grant No. 79153).