Floors are increasingly recognized as a potential source for the transmission of healthcare-associated pathogens. Reference Donskey1–Reference Redmond, Pearlmutter and Ng-Wong4 In patient rooms, a nonpathogenic virus inoculated on the floor disseminated to the footwear and hands of patients, to surfaces in the room, to adjacent rooms, and to nursing stations. Reference Koganti, Alhmidi, Tomas, Cadnum, Jencson and Donskey3 In rooms of newly admitted patients, healthcare-associated pathogens rapidly contaminated the floor as personnel entered the room, with subsequent detection on patients’ sock bottoms, bedding, and high-touch surfaces. Reference Redmond, Pearlmutter and Ng-Wong4 In 2 recent studies, Clostridioides difficile strains recovered from the shoes of personnel and from the stool of infected patients were genetically linked based on whole-genome sequencing analysis. Reference Janezic, Blazevic, Eyre, Kotnik Kevorkijan, Remec and Rupnik5,Reference Büchler, Wicki and Frei6
Liquid disinfectants or ultraviolet-C (UV-C) light can reduce the burden of pathogens on floors. Reference Carlisle, Rutala, Cadnum, Wilson, Deshpande and Donskey7 However, contamination can rapidly reaccumulate as personnel or wheeled equipment enters the room. Thus, new approaches are needed to reduce the risk for acquisition of pathogens from floors. In a previous simulation study, use of a UV-C light shoe-decontamination device reduced pathogen contamination on floors, surfaces, and a patient dummy. Reference Rashid, Poblete, Amadio, Hasan, Begum, Alam and Garey8 We examined the frequency of transfer of pathogens onto floors in patient rooms via shoes of personnel, and we tested whether a UV-C shoe decontamination device would reduce pathogen transfer.
Methods
UV-C light shoe decontamination device
The HealthySole PLUS UV-C light shoe-decontamination device (HealthySole, Incline Village, NV) provides an 8-s cycle of UV-C light to the soles of shoes. Pictures of the device are shown in Supplementary Fig. 1 (online). Individuals stand on a specified area on a platform with shoe placement identified by outlines of shoes. The UV-C treatment is initiated when 4 infrared sensors indicate that 2 shoes are in place over the UV-C delivery area. The device is calibrated to operate only if shoes are women’s size 6 or greater. A screen display indicates when shoe placement is correct and when the cycle is in process, and a buzzing noise indicates cycle completion.
Efficacy of UV-C treatment in reducing the transfer of pathogens from shoes to floors
We evaluated the effectiveness of the UV-C shoe-decontamination device in empty patient rooms that had been cleaned and disinfected by environmental services personnel. Research personnel completed additional cleaning and disinfection of a 2-m-wide area of the floor extending from the doorway to the patient bed using a commercial bleach wipe containing 5,500 parts per million sodium hypochlorite. After a 5-minute wet contact time, the cleaned floor surface was wiped with paper towels moistened with water to remove residual bleach and was allowed to air dry.
In our experiment, 32 healthcare personnel were asked to walk into and out of the room on the disinfected floor following a specified 1-m-wide path extending from the doorway to the bed. After exiting the room, the personnel stood on the UV-C shoe decontamination device for one 8-second cycle before again walking into and out of the room on a separate specified 1-m-wide path. For the floor sections where personnel walked before and after UV-C shoe treatment, Replicate Organism Detection and Counting (RODAC) plates with enterococcosel agar (Becton Dickinson, Franklin Lakes, NJ) and CHROMAgar (Becton Dickinson) selective for Staphylococcus aureus were applied to 3 separate locations. The plates were incubated for 48 hours. Colonies consistent with enterococci and S. aureus were subjected to identification and susceptibility testing using standard methods. 9 Total colony-forming units (CFU) of vancomycin-susceptible enterococci, vancomycin-resistant enterococci, methicillin-susceptible S. aureus, and methicillin-resistant S. aureus were counted.
After collection of the RODAC cultures, sterile gauze premoistened with Dey-Engley neutralizing broth (Difco, Franklin Lakes, NJ) was used to wipe 1-m × 10-cm sections of the floor that had been contacted by shoes before or after UV-C shoe treatment. The gauze samples were cultured for C. difficile by broth enrichment. Reference Janezic, Blazevic, Eyre, Kotnik Kevorkijan, Remec and Rupnik5
Efficacy of multiple UV-C treatments in reducing MRSA and C. difficile on shoe soles
To assess the impact of repeated UV-C treatments on shoe contamination, shoe soles were contaminated with 6 log10 CFU of a clinical isolate of MRSA and a ribotype 027 toxigenic strain of C. difficile (American Type Culture Collection no. 43598). The soles were treated with 6 consecutive 8-s cycles of with the UV-C device. After 1, 3, and 6 cycles, CultureSwabs (Becton Dickinson) were used to sample inoculation sites. Log10 reductions in MRSA and C. difficile spores were calculated.
Data analysis
The primary outcome was the frequency and burden of contamination of the floor with 1 or more vegetative pathogens. The McNemar χ2 test was used to compare the frequency of contamination with 1 or more vegetative pathogens and with C. difficile spores before versus after shoe treatment with UV-C. The Wilcoxon signed-rank test was used to compare the mean CFU of a composite of the vegetative pathogens recovered from floors before versus after UV-C shoe treatment. Data were analyzed using R version 3.5.0 software (R Foundation for Statistical Computing, Vienna, Austria).
Results
Figure 1A shows the percentage transfer of pathogens from shoes to floors before versus after UV-C treatment of shoes. UV-C treatment significantly reduced transfer of a composite of the vegetative pathogens to floors [27 (84%) of 32 vs 9 (28%) of 32; P < .001]. However, UV-C treatment did not significantly reduce transfer of C. difficile [12 (38%) of 32 versus 7 (22%) of 32; P = .58]. As shown in Figure 1B, UV-C treatment resulted in a significant reduction in the mean number of vegetative pathogens transferred (P < .001).
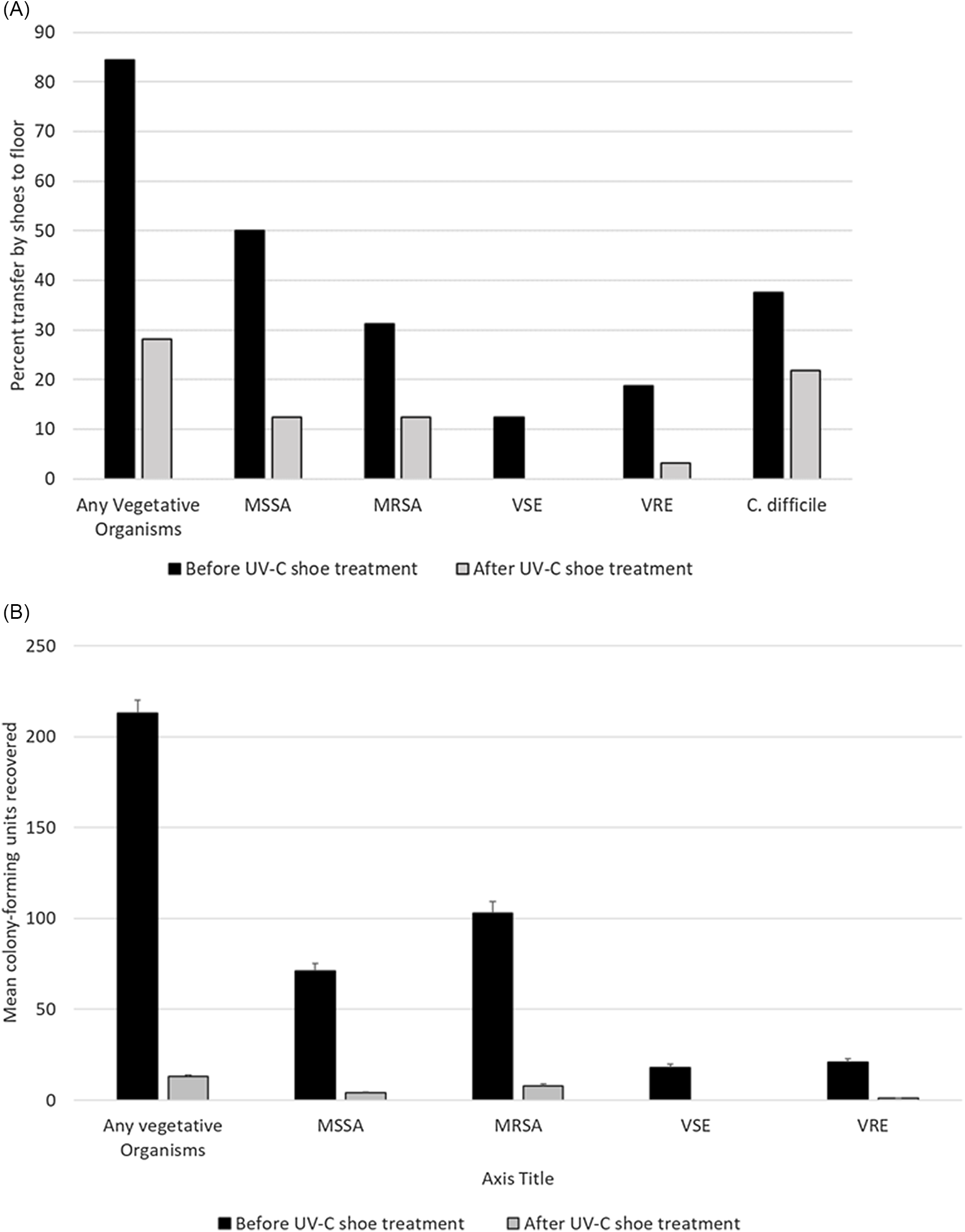
Fig. 1. Percentage of pathogen transfer from shoes of personnel to floors in patient rooms (A) and number of vegetative pathogens transferred (B) before versus after ultraviolet-C (UV-C) treatment of shoes. Note. MSSA, methicillin-susceptible Staphylococcus aureus; MRSA, methicillin-resistant S. aureus; VSE, vancomycin-susceptible enterococci; VRE, vancomycin-resistant enterococci. Error bars show standard deviation.
Figure 2 shows the log10 CFU reductions in MRSA and C. difficile on inoculated shoe soles after 1, 3, and 6 cycles of UV-C treatment. After a single cycle, MRSA was reduced by >3 log10, whereas the mean reduction in C. difficile spores was only 0.57 log10. After 6 cycles of UV-C, the mean CFU reduction in C. difficile spores was 2.0 log10.
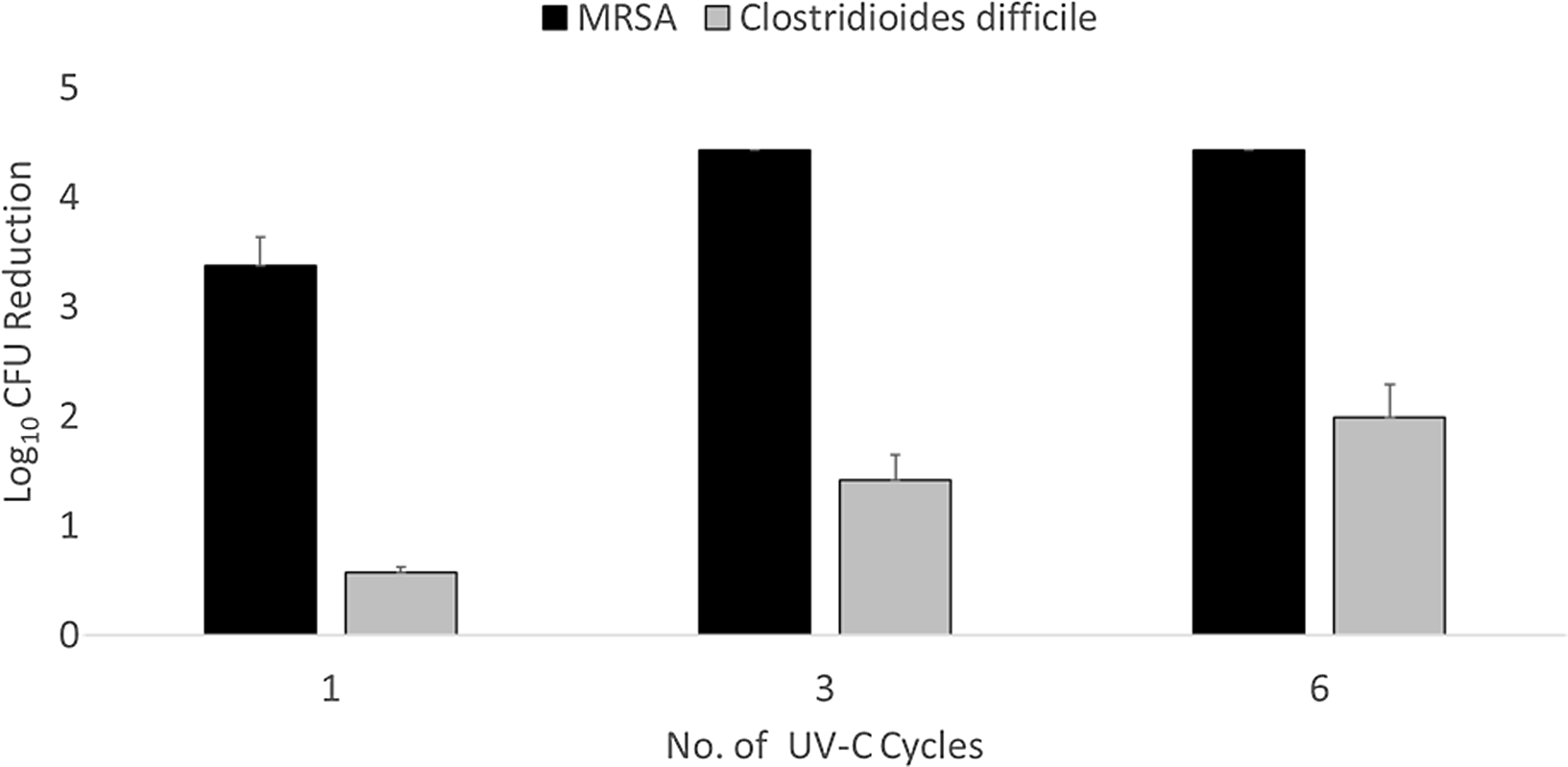
Fig. 2. Log10 colony-forming unit (CFU) reduction in methicillin-resistant Staphylococcus aureus (MRSA) and Clostridioides difficile spores on inoculated shoe soles after one, three, or six 8-s treatments with an ultraviolet-C light.
Discussion
Several studies have demonstrated that the shoes of healthcare personnel are often contaminated with healthcare-associated pathogens. Reference Janezic, Blazevic, Eyre, Kotnik Kevorkijan, Remec and Rupnik5–Reference Carlisle, Rutala, Cadnum, Wilson, Deshpande and Donskey7,Reference Kanwar, Thakur and Wazzan10 Our results build upon those findings by demonstrating that personnel walking into patient rooms frequently transfer healthcare-associated pathogens from their shoes to the floor. In addition, we demonstrated that an 8-s treatment of shoes with a UV-C decontamination device significantly reduced the frequency of transfer of vegetative pathogens but not C. difficile. These findings suggest that the UV-C device could potentially be used to reduce transfer of pathogens into rooms of patients.
The finding that a single 8-s UV-C cycle did not significantly reduce transfer of C. difficile from shoes is not surprising given the relative resistance of C. difficile spores to UV-C. Reference Donskey1,Reference Janezic, Blazevic, Eyre, Kotnik Kevorkijan, Remec and Rupnik5,Reference Rashid, Poblete, Amadio, Hasan, Begum, Alam and Garey8 Using the same device, Rashid et al Reference Rashid, Poblete, Amadio, Hasan, Begum, Alam and Garey8 found that a single UV-C cycle resulted in only a 0.42±0.54 log10 reduction in C. difficile spores. However, we demonstrated that a 2 log10 reduction in C. difficile spores was achieved on inoculated shoe soles after six 8-s cycles. In practice, the shoes of personnel may receive repeated UV-C treatments that might be effective in reducing transfer of spores.
Our study had several limitations. The study was conducted in a single facility with a small number of personnel who entered the test room only once with and once without UV-C shoe decontamination. Only 3 gram-positive bacterial pathogens were studied. Studies are needed to evaluate efficacy against additional pathogens and during repeated room entries and to determine whether the use of this device will reduce acquisition of healthcare-associated pathogens. Finally, we did not compare the UV-C device with other potential methods to reduce transfer of pathogens into patient rooms on shoes (eg, shoe covers).
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2022.242.
Acknowledgments
We thank HealthySole for providing the HealthySole PLUS device used for testing.
Financial support
This work was supported by the Department of Veterans’ Affairs (Merit Review grant no. CX001848 to C.J.D.).
Conflicts of interest
C.J.D. has received research grants from Clorox, Pfizer, PDI, and Ecolab. All other authors report no conflicts of interest relevant to this article.





