CASE
A 47-year-old homeless male presents to the emergency department (ED) with right lower extremity swelling, erythema and pain. He has diabetes mellitus, and had one prior episode of cellulitis three months ago affecting the same leg. He has a history of medication noncompliance. At triage, his temperature is 38.3°C but the remaining vital signs are unremarkable. On examination of the affected leg, there is an approximately 10 × 10 cm area of erythema, induration and increased warmth. There is mild tenderness to palpation and you wonder if there is a small degree of fluctuance. There is no lymphangitis, crepitus, necrosis or pain out of proportion to clinical findings.
- 1.
In this patient, other than the most likely diagnosis of cellulitis, what are important differential diagnoses to consider?
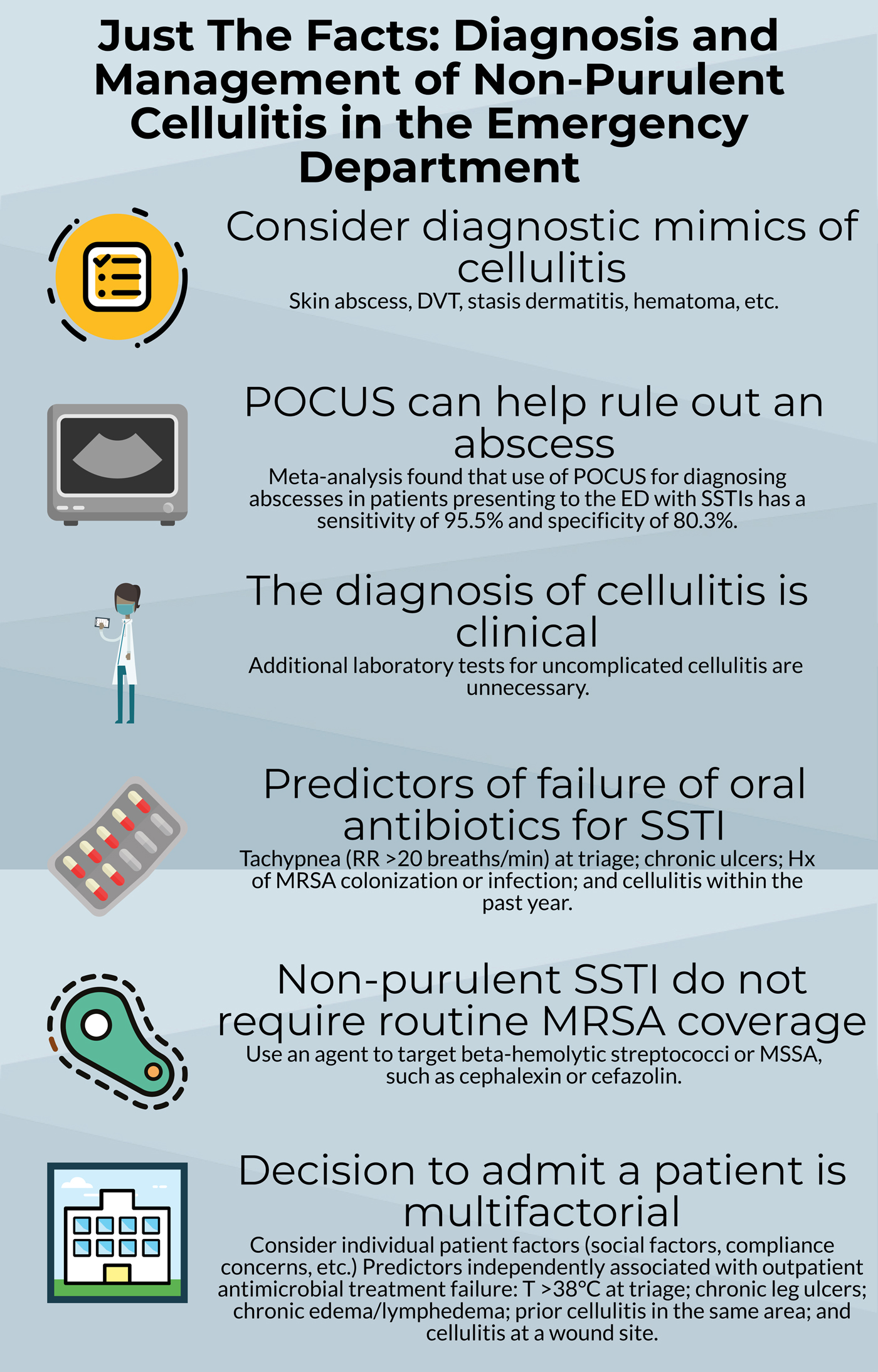
Consider important diagnostic mimics of cellulitis, such as an abscess, deep vein thrombosis or ruptured Baker's cyst.
The diagnosis of non-purulent skin and soft tissue infections (SSTIs; cellulitis or erysipelas) remains challenging due to a large number of diagnostic mimics (Box 1).Reference Raff and Kroshinsky1 Up to one-third of initial patient presentations may be misdiagnosed as cellulitis. Misdiagnosed patients with non-infectious underlying pathology are subjected to unnecessary antimicrobial therapy and its associated risk of adverse effects, in addition to potentially unnecessary hospitalization and investigations.
Box 1: Conditions that mimic cellulitisFootnote *

* Adapted in part from data by Raff and Kroshinsky1
- 2.
This patient had possible mild fluctuance. What is the utility of point-of-care ultrasonography (POCUS) to differentiate between non-purulent cellulitis versus cellulitis with abscess?
If the diagnosis of non-purulent cellulitis versus abscess is unclear, use POCUS to rule out an underlying collection.
Differentiating abscesses from non-purulent cellulitis is important because the management is very different. A bedside procedure (incision and drainage, loop drainage or needle aspiration) is a vital component for managing abscesses. In contrast, antibiotics alone are required to treat non-purulent cellulitis. One tool at the emergency physician's disposal is the use of point-of-care ultrasonography (POCUS). A recent meta-analysis found that use of POCUS for diagnosing abscesses in ED patients with SSTIs has a sensitivity of 95.5% and specificity of 80.3%.Reference Barbic, Chenkin, Cho, Jelic and Scheuermeyer2 When there is clinical suspicion, POCUS should be used to rule out the presence of an underlying abscess.
- 3.
Does this patient require any further investigations?
Laboratory tests for uncomplicated cellulitis are unnecessary. The diagnosis of cellulitis is clinical.
Wound cultures are not easily performed for non-purulent SSTIs without associated ulcers. Blood cultures are low yield and laboratory tests such as white blood cell count or C-reactive protein would be typically elevated but not specific for cellulitis. Thus, laboratory tests are often unhelpful and the diagnosis of cellulitis is clinical. Adjunct tests may be useful in certain situations. For example, ultrasonography may be indicated to rule out a deep vein thrombosis or ruptured Baker's cyst.
- 4.
Does this patient require oral or intravenous antibiotics?
When selecting the route of therapy, the following factors are considerations for IV therapy: failed oral therapy; systemically unwell; clinical signs of deeper infection; immunocompromised; plus additional factors (tachypnea at triage, chronic ulcers, history of MRSA colonization or infection, cellulitis in the past year).
Selecting the optimal route of antimicrobial therapy is a key decision point in the management of SSTIs for emergency physicians. Oral antibiotics hold several advantages over the intravenous (IV) route, including fewer complications, decreased cost, and increased patient convenience and comfort. Current guidelines recommend IV therapy for ‘moderate’ (fever, tachypnea, tachycardia or abnormal white blood cell count) or ‘severe’ (failed oral therapy, clinical signs of deeper infection or immunocompromised) infections.Reference Stevens, Bisno and Chambers3 A recent health records review at two Canadian EDs identified four factors associated with oral antibiotic treatment failure for non-purulent SSTIs: tachypnea (respiratory rate >20 breaths/minute) at triage; chronic ulcers; history of MRSA colonization or infection; and cellulitis within the past year.Reference Yadav, Suh and Eagles4 These factors, along with availability of outpatient IV programs, should be considered when deciding upon oral versus IV therapy.
- 5.
Should this patient receive antibiotics that are effective against methicillin-resistant Staphylococcus aureus (MRSA)?
Antimicrobial therapy should target β-hemolytic streptococci and MSSA for non-purulent cellulitis. We recommend a first-generation cephalosporin (cephalexin or cefazolin).
The growing prevalence of methicillin-resistant Staphylococcus aureus (MRSA) SSTIs has led some clinicians to question whether all SSTIs should be treated with antibiotics effective against MRSA. However, β-hemolytic streptococci and (to a lesser degree) methicillin-susceptible Staphylococcus aureus (MSSA) remain the predominant causes of non-purulent cellulitis. Non-purulent cellulitis should be treated with antimicrobials effective against β-hemolytic streptococci, such as cephalexin or cefazolin.
- 6.
Can this patient be discharged home or does he require hospital admission?
Multiple considerations, including social and individual patient factors, influence the decision to hospitalize patients with uncomplicated cellulitis.
The decision to manage non-severe SSTIs as an inpatient versus outpatient is influenced by many factors. If patients require IV therapy, outpatient parenteral antibiotic therapy (OPAT) is an attractive option to avoid the need for hospitalization. OPAT can be delivered in a number of settings (ED, outpatient clinic, or in the home). Social factors (e.g. homelessness, injection drug use) may warrant hospital admission to ensure compliance and for patient safety. A prospective observational cohort study at two Canadian EDs identified five predictors independently associated with outpatient antimicrobial (oral or IV) treatment failure: fever (temperature >38°C) at triage; chronic leg ulcers; chronic edema or lymphedema; prior cellulitis in the same area; and cellulitis at a wound site.Reference Peterson, McLeod, Woolfrey and McRae5 These identified factors, in addition to individual patient circumstances, should be considered when deciding upon inpatient versus outpatient therapy.
CASE RESOLUTION
The emergency physician rules out the presence of an underlying abscess by using POCUS. This patient has several factors (fever and cellulitis in the preceding year) that warrant IV therapy. The patient receives intravenous cefazolin, which is effective against β-hemolytic streptococci and MSSA. This patient also has factors (fever and prior cellulitis in the same area) that may be associated with outpatient failure. Factors such as homelessness, a history of medication noncompliance, concerns about patient safety and access to outpatient care result in a decision to refer for hospital admission and further care.
Funding source
None.
Competing interests
None to declare.



