Schizophrenia is a heterogeneous disorder with good symptomatic and functional outcomes in some patients although others have a more severe, deteriorating course (Reference Wiersma, Nienhuis and SlooffWiersma et al, 1998). This heterogeneity can result from environmental factors as well as differences in the underlying disease biology. Antipsychotic medication treatment might be such an environmental factor, with earlier intervention increasing the likelihood of good response (Reference Loebel, Lieberman and AlvirLoebel et al, 1992). Early age of onset and poor premorbid function are associated with prognosis and could be the behavioural manifestation of brain function impairments indicative of a poor prognosis (Reference Lieberman, Perkins and BelgerLieberman et al, 2001b ). Such factors could also conceivably lead to treatment delay and therefore confound the relationship of duration of untreated psychosis (DUP) with outcome (Reference McGlashanMcGlashan, 1999). In this study we evaluated the independent contributions of DUP, age at onset and premorbid function to rate of symptom remission, change in psychopathology severity and social and vocational function.
METHOD
Data for this study were collected as part of a 2-year randomised, double-blind clinical trial that compared the efficacy and safety of olanzapine with that of haloperidol in patients experiencing a first-episode of DSM–IV (American Psychiatric Association, 1994) schizophrenia, schizophreniform or schizoaffective disorder. The trial was conducted from March 1997 to July 2001 at 14 academic centres in North America and Western Europe. All study personnel and participants remained masked for the total duration of the study and until the study data-set was completely finalised. A detailed description of the study methods is available in an earlier publication (Reference Lieberman, Tollefson and TohenLieberman et al, 2003).
Participants
Participants were aged 16–40 years and met DSM–IV diagnostic criteria before age 35 years. They could not have been ill for more than 5 years because individuals with longer duration of illness might be clinically more similar to patients with chronic disease rather than a first-episode. If a prior psychotic episode had remitted 6 months or longer before enrolment, patients were not considered first-episode and were therefore excluded. Individuals were excluded from the study if they had prior antipsychotic drug treatment for more than 16 cumulative weeks. Subjects experienced active psychotic symptoms (scored ≥4 on at least two or scored ≥5 on one of the Positive and Negative Syndrome Scale (PANSS; Reference Kay, Opler and LindenmayerKay et al, 1988) psychosis items P1, P2, P3, P5 or P6, and scored ≥4 on the Clinical Global Impression Severity Scale (CGI-S; Reference GuyGuy, 1976)) and had a premorbid IQ ≥70. In order not to compromise patient safety in a randomised trial, participants could not be at serious suicidal risk. Each participant (or an authorised legal representative) had to understand the nature of the study and sign an informed consent document.
Study design and procedures
Upon study enrolment, a 2- to 14-day screening and washout period was required for all participants who were currently taking psychotropic medication. Following this period, participants were randomised to treatment with olanzapine (5–20 mg/day) or haloperidol (2–20 mg/day), using a central, interactive voice-response system. Baseline study evaluations were carried out before randomisation, and follow-up clinical ratings were performed weekly for the first 6 weeks, every 2 weeks for the next 6 weeks, and monthly afterwards for up to 2 years.
Predictor measures
Measurement of DUP requires the determination of the onset of psychosis and the onset of treatment. Data on the onset of psychosis were determined with the Symptom Onset in Schizophrenia (SOS) scale, a clinician-administered scale that has previously demonstrated excellent interrater reliability (Reference Perkins, Leserman and JarskogPerkins et al, 2000). The SOS scale rates the occurrence and dates the onset of 16 prodromal symptoms and of psychosis (hallucinations, delusions and disorganisation). Defining the onset of treatment is complicated by the fact that most patients had brief exposure to an antipsychotic before randomisation with the study drug. A total of 62% (119/191) of the participants were receiving acute antipsychotic treatment for their psychosis immediately preceding study entry. The mean length of this acute antipsychotic treatment was 26.1 days (s.d.=27.1, median=16.0). Another 23% (44/191) had one or more past brief trials insufficient to lead to treatment remission, where the patient had taken an antipsychotic for at least 1 day but had stopped taking the antipsychotic at least 2 weeks before the current treatment episode. Among the participants who had a prior antipsychotic trial, the mean duration of previous treatment was 34.3 days (s.d.=39.0, median=17). Given these ambiguities, we chose a priori to define onset of treatment for antipsychotic-naïve participants as the date of randomisation. For those who were receiving a commercially available antipsychotic immediately before study enrolment, onset of treatment was defined as the initiation date of that acute antipsychotic treatment. Previous brief episodes of antipsychotic treatment that did not result in symptom remission and that had ended at least 2 weeks before the onset of the current trial were not considered clinically meaningful trials, and were not considered in the dating of treatment onset. The DUP was thus calculated as the number of months between the date that the subject first experienced a psychotic symptom and onset of treatment, as defined above. As indicated above, all patients taking psychotropic medications at study enrolment had a 2- to 14-day washout period before randomisation.
Age at onset of psychosis was calculated from the SOS scale as the age when the subject first experienced psychotic symptoms. Premorbid social and occupational function was rated with the Premorbid Adjustment Scale (PAS; Reference Cannon-Spoor, Potkin and WyattCannon-Spoor et al, 1982) total score with lower scores indicating better function. The SOS and PAS interviews were conducted at 12-week follow-up or study withdrawal.
Outcome measures
Severity of symptoms was evaluated with the PANSS (30 items, 1–7 scale), the Montgomery–Åsberg Depression Rating Scale (MADRS; Reference Montgomery and AsbergMontgomery & Åsberg, 1979; 10 items, 0–6 scale) and the CGI-S (1–7 scale). Patients who met the following criteria for 4 consecutive weeks were classified as remitters: no rating of >3 (mild) on items P1, P2, P3, P5, and P6 of the PANSS; and a CGI Severity score ≤3 (mildly ill). Social and vocational function ratings were available for a sub-sample of 52 participants only, as determined from the relevant first 12 items of the Heinrich Carpenter Quality of Life (QOL) scale (Reference Heinrichs, Hanlan and CarpenterHeinrichs et al, 1984).
Control measures and rater training
In all analyses we controlled for site, antipsychotic drug randomisation, and baseline symptom severity. Formal training for all clinical rating scales was provided at an investigator meeting, supplemented by written training materials. Training for the PANSS, SOS and QOL scales included rating of a videotaped interview, followed by discussion and review of ratings. No formal assessment of rater reliability was carried out for any clinical measure.
Statistical methods
All analyses were performed on an intent-to-treat basis including all randomised participants who provided information about premorbid function and symptom onset. When last-observation-carried-forward change from baseline to end-point was assessed, patients were included in the analysis only if both a baseline and post-baseline measure were available.
Related statistical assumptions and interactions were examined before proceeding with the model selection. To avoid the undue influence from the right skewness in distributions of DUP and days of pre-study antipsychotic treatment, log2 transformation (the base of 2 was chosen for the convenience of interpretation) was applied to these data. As a sensitivity measure, the results were double-validated by categorising DUP into long and short groups split at median. Both results are reported.
Changes in PANSS total, positive, negative and MADRS scores were modelled with hierarchical linear regression models to evaluate independent contributions of DUP, premorbid course and premorbid functioning after the effects of other important predictors had been accounted for. The model first controlled for possible confounding effects from site, baseline and therapy, followed by a stepwise procedure to select important predictor variables from age, gender, ethnicity, smoking status, diagnosis, age at onset and duration of pre-study treatment. A variable had to reach statistical significance at the 0.05 level to enter the model and 0.10 to stay. Premorbid function and log2DUP entered the model last. Finally, we checked the possible interactions between significant predictors and therapy.
The survival curves for time to remission were estimated for short and long DUP groups using the Kaplan–Meier method and tested by the log-rank test. Finally, a survival model was built using Cox regression following the similar strategy outlined above.
Because the data were collected in a study designed originally to compare the efficacy of two antipsychotics, this paper reports secondary analyses. The primary outcomes of interest are rate of remission and change in overall psychopathology (total PANSS score) with either olanzapine or haloperidol treatment for up to 2 years. Additional end-points are reported to provide a complete profile of outcome measures. Interpretation of these results should keep in mind the nature of secondary analysis of this study and multiplicity in hypothesis-testing for additional end-points.
RESULTS
Participants
A total of 263 participants entered the study and were randomised to treatment. From this group, 191 individuals had complete SOS and PAS information and were included in these analyses. SOS and PAS data were collected at the completion of 12 weeks of treatment for most participants (n=152), and were collected at study withdrawal before 12 weeks of treatment for the remainder.
From these 191 participants, 115 (60%) discontinued before completing 1 year of treatment. A total of 66 of these 115 did not meet remission criteria: all 24 of the early discontinuation participants with short DUP and 42 of those with long DUP. By 2 years no additional participants with short DUP, but an additional four with long DUP, had withdrawn without meeting remission criteria (Fig. 1). Reasons for study withdrawal for participants with short and long DUP, respectively, included: lack of efficacy (23% and 29%); adverse events (17% and 12%); patient decision (27% and 23%); physician decision (13% and 18%); and protocol violation/unknown (20% and 18%).

Fig. 1 CONSORT diagram with remission status.
Demographic and other descriptive data are presented in Table 1. The participants’ mean age was 24 years (s.d.=4.9). The distribution of DUP is illustrated in Fig. 2; DUP was right-skewed (skewness=3.2) with an interquartile range from 2 to 24 months and longest DUP at 167 months. (Note that although the study excluded individuals with illness duration greater than 5 years, some patients reported intermittent brief psychotic symptoms as part of the prodrome, and psychosis onset was dated at the time that the first hallucinations or delusions were experienced.) Longer DUP was associated with an earlier age at onset of illness (Spearman correlation, r=–0.15, P=0.03), but DUP was not associated with premorbid function (r=0.09, P=0.21), or with duration of antipsychotic exposure before the current treatment episode (r=–0.09, P=0.21). Consistent with their DSM–IV definitions, patients with schizophreniform disorder had significantly shorter DUP than patients with schizophrenia or schizoaffective disorder (χ2(2)=53.0, P<0.0001 by Kruskal–Wallis test).
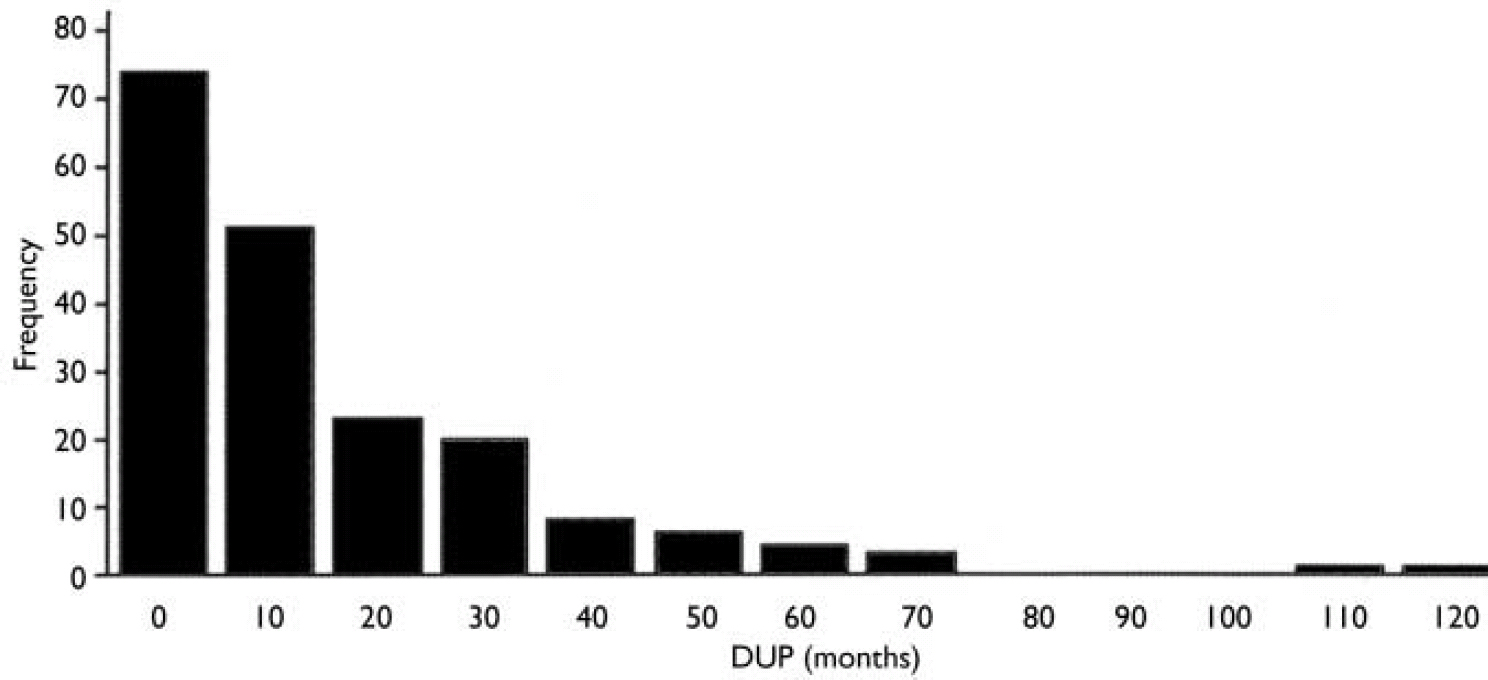
Fig. 2 Duration of untreated psychosis (DUP) distribution.
Table 1 Associations between historical variables and other patient characteristics

| DUP (months) | Age at onset (years) | PAS score (0–1) | Prior antipsychotic treatment (days) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | s.d. | Median | Mean | s.d. | Median | Mean | s.d. | Median | Mean | s.d. | Median | |
| Total group (n=191) | 15.08 | 20.44 | 8.00 | 22.38 | 5.03 | 22.00 | 0.33 | 0.15 | 0.33 | 16.28 | 24.86 | 7.00 |
| Gender | ||||||||||||
| Male (n=153) | 15.56 | 21.43 | 8.00 | 21.95 | 4.62 | 21.00 | 0.34 | 0.16 | 0.33 | 15.49 | 24.10 | 7.00 |
| Female (n=38) | 13.16 | 15.89 | 7.00 | 24.11 | 6.19 | 23.00 | 0.29 | 0.14 | 0.29 | 19.45 | 27.81 | 2.00 |
| Ethnicity | ||||||||||||
| White (n=108) | 15.96 | 18.94 | 9.00 | 23.04 | 5.62 | 22.00 | 0.32 | 0.15 | 0.32 | 14.93 | 25.28 | 4.00 |
| Other (n=83) | 13.93 | 22.30 | 6.00 | 21.52 | 4.00 | 21.00 | 0.34 | 0.16 | 0.35 | 18.04 | 24.33 | 8.00 |
| Diagnosis | ||||||||||||
| Schizophrenia (n=120) | 20.19 | 23.041 | 13.00 | 21.93 | 4.80 | 21.00 | 0.32 | 0.13 | 0.31 | 15.57 | 25.69 | 3.50 |
| Schizophreniform (n=54) | 3.39 | 5.321 | 1.00 | 23.19 | 4.72 | 23.00 | 0.33 | 0.18 | 0.31 | 13.43 | 16.05 | 9.00 |
| Schizoaffective (n=17) | 16.12 | 16.111 | 7.00 | 23.00 | 7.12 | 20.00 | 0.41 | 0.20 | 0.41 | 30.35 | 36.50 | 16.00 |
| Therapy | ||||||||||||
| Olanzapine (n=95) | 12.46 | 17.662 | 5.00 | 22.39 | 5.23 | 21.00 | 0.33 | 0.16 | 0.33 | 18.81 | 27.48 | 8.00 |
| Haloperidol (n=96) | 17.67 | 22.652 | 10.50 | 22.36 | 4.84 | 22.00 | 0.33 | 0.15 | 0.31 | 13.77 | 21.81 | 4.50 |
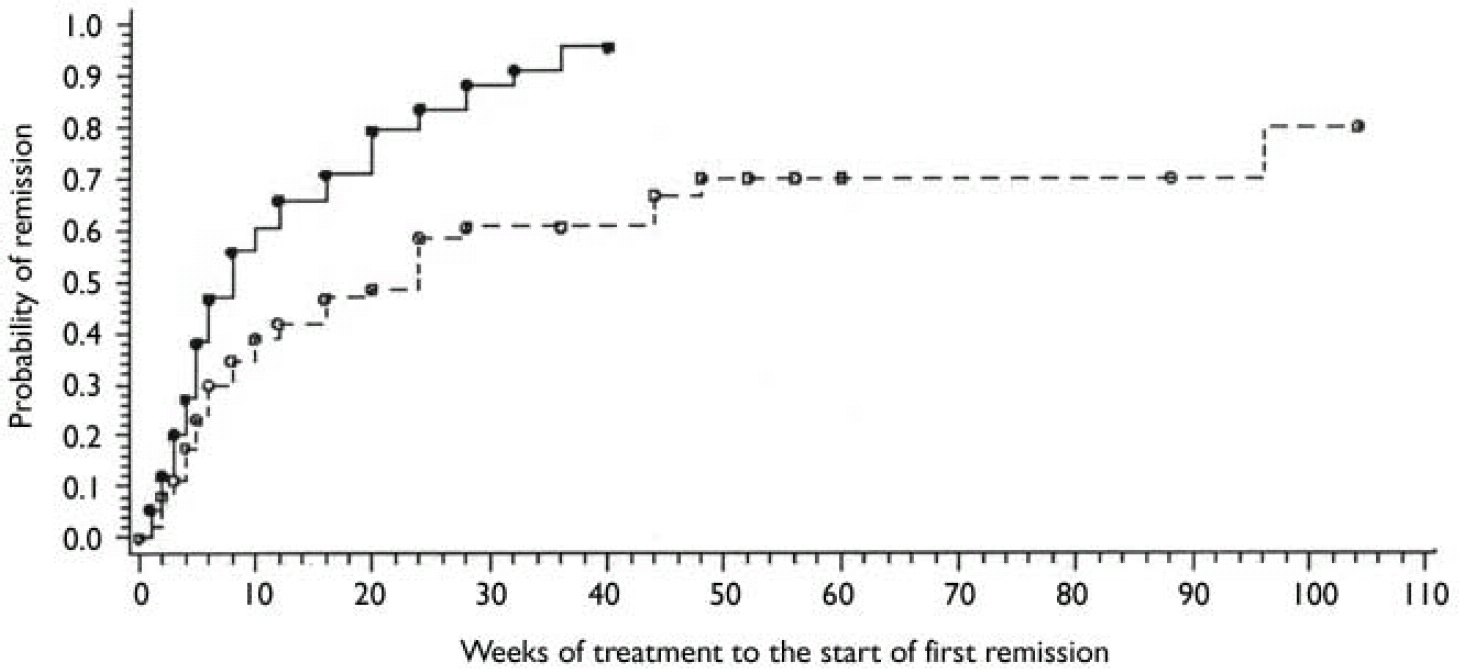
Fig. 3 Proportion of subjects with short and long duration of untreated psychosis (DUP) meeting remission criteria for at least 4 weeks. ○, censored long DUP; - - -, long DUP; •, censored short DUP;—, short DUP. Censored data: results included those of participants who did not complete the entire follow-up period.
Overall change in psychopathology
The results for treatment outcome predictors were remarkably consistent between the 12-week complete data and 2-year last-observation-carried-forward data. To avoid redundancy, only the primary results of 2 years’ data with log2DUP as a continuous covariate are reported here. For comparison, both 12-week and 2-year DUP results are listed in Table 2 analysed as a binary variable.
Table 2 Summary results for short and long duration of untreated psychosis (DUP) groups at 12 weeks and 2 years. Data presented are model estimated means, controlling for study site, therapy, baseline of the outcome measurement and premorbid function

| Outcomes | 12 weeks | 2 years | ||||||
|---|---|---|---|---|---|---|---|---|
| Short DUP LS (n=92) | Long DUP LS (n=99) | Difference | Short DUP LS (n=92) | Long DUP LS (n=99) | Difference | |||
| 95% CI | P | 95% CI | P | |||||
| PANSS | ||||||||
| Total | 54.2 | 60.8 | 1.8 to 11.4 | 0.01 | 55.4 | 62.3 | 1.7 to 12.2 | 0.01 |
| Positive | 11.3 | 13.0 | 0.3 to 2.9 | 0.02 | 12.7 | 14.7 | -0.0 to 3.2 | 0.05 |
| Negative | 16.0 | 17.6 | -0.1 to 3.3 | 0.06 | 14.7 | 16.9 | 0.7 to 3.9 | 0.01 |
| MADRS | 9.4 | 9.5 | -2.4 to 2.6 | 0.94 | 10.1 | 10.3 | -2.2 to 2.5 | 0.90 |
| QOL | ||||||||
| Social | 25.6 | 25.7 | -4.9 to 5.0 | 0.97 | 26.5 | 26.6 | -4.5 to 4.7 | 0.97 |
| Vocational | 12.6 | 12.5 | -3.3 to 3.1 | 0.96 | 14.3 | 13.3 | -4.2 to 2.2 | 0.54 |
After controlling for site, therapy and baseline values, the final model (F(13,176)=5.60, P<0.0001, r 2=0.30) showed that lower PANSS total scores at end-point were associated with better premorbid function (F(1,176)=11.9, P=0.0007, r 2=0.05) and shorter log2DUP (F(1,176)=4.3, P=0.04, r 2=0.02), but not with age at illness onset or other background variables. Independently, premorbid function and log2DUP contributed 5% and 2% to the total variance, respectively. With every 0.1 point decrease in PAS score, there was a 3.2 point (95% CI 1.4–5.1) improvement (decrease) in PANSS total score at end-point and when DUP was shortened by half of the original value (i.e. every 1 point decrease in log2DUP), there was a 1.5 point (95% CI 0.1–2.8) greater improvement in PANSS total score. The effects of log2DUP and PAS score were the same in the haloperidol- and olanzapine-treated subjects, indicated by negligible interaction terms for treatment randomisation (P>0.20 in both cases).
Positive symptoms
With the control variables of site, therapy and baseline values included, premorbid function was the only significant variable significantly associated with positive symptom improvement at end-point (F(1,176)=9.81, P<0.002, r 2=0.04). Every 0.1 decrease in PAS score was associated with a 0.9 point (95% CI 0.3–1.4) improvement in positive symptom severity. Again, the PAS effect was independent of antipsychotic treatment group (P>0.60). The association of log2DUP with positive symptom improvement was considerably weaker (P=0.14).
Negative symptoms
Both premorbid function and log2DUP were significantly associated with end-point negative symptom improvement (premorbid function F(1,176)=5.5, P=0.02, r 2=0.02; log2DUP F(1,176)=4.7, P=0.03, r 2=0.02). There was a 0.7 point (95% CI 0.1–1.3) improvement in negative symptoms when the PAS score was reduced by 0.1 point, and a 0.5 point (95% CI 0.1–0.9) improvement when DUP was shortened by half. Again, these findings were independent of antipsychotic treatment (P>0.40 for both). None of the other variables was related to negative symptom outcome.
Depressive symptoms
Premorbid function and DUP were not associated with change in severity of depressive symptoms as evaluated by the MADRS.
Functional outcome
Premorbid function was the only variable significantly associated with social and vocational function outcome at end-point (social function F(1,52)=3.73, P=0.06, r 2=0.03; vocational function F(1,51)=6.60, P=0.01, r 2=0.08). A 0.1 point better PAS score was associated with a 1.4 point (95% CI –0.1 to 2.9) improvement in social function and a 1.8 point (95% CI 0.6–3.0) improvement in vocational function. Again, these effects were independent of antipsychotic treatment group (P>0.40). The association of log2DUP and premorbid function with social and vocational improvement was considerably weaker (P>0.20 for both).
Remission
By the end of 1 year, 68 (74%) of the 92 participants with short DUP and 50 (51%) of the 99 participants with long DUP met remission criteria. The remaining 24 participants with short DUP and 42 of those with long DUP withdrew from the study before 1 year, and their ultimate remission status is not known. By year 2, another participant with long DUP had remitted (51 out of 99, 52%). Four more participants with long DUP withdrew without meeting remission criteria, and two with long DUP completed the study without meeting remission criteria (Fig. 1).
As shown in Fig. 2, the Kaplan–Meier estimates for the remission rates were consistently higher for individuals with short compared with long DUP (χ2(1)=9.89, P=0.0017). Median time to remission was 8 weeks for short and 24 weeks for long DUP groups. After controlling for therapy and baseline PANSS total, the Cox regression model found significant associations of shorter DUP and better premorbid function with shorter time to remission (log2DUP χ2(1)=14.6, P=0.0001; premorbid function: χ2(1)=4.27, P=0.04). The remission hazard ratio would increase by 18% and 15%, respectively, when DUP was reduced by half or when premorbid function was improved by 0.1 points.
DISCUSSION
Duration of untreated psychosis and clinical outcome
The major findings of these analyses are that shorter DUP and good premorbid function are independently associated with a shorter time to illness remission. Although a greater proportion of participants with short DUP compared with long DUP met remission criteria at 1 year, by 2 years an additional participant with long DUP had improved so that the difference in proportion was not statistically significant. Thus, it could be that DUP influences the rate of symptom improvement rather than the ultimate likelihood of remission.
Shorter DUP and good premorbid function are also associated with clinical response of the first psychotic episode to antipsychotic medication, as measured by improvement in overall psychopathology and severity of negative symptoms. Good premorbid function is associated with positive symptom improvement and improvement in social and vocational function. The sizes of the effects are small to moderate.
The results of this study are in agreement with the findings of the majority of other studies that have examined the relationship between DUP and outcome in patients with first-episode psychosis. Most studies have found associations with the likelihood of symptom remission (Reference Loebel, Lieberman and AlvirLoebel et al, 1992; Reference Wiersma, Nienhuis and SlooffWiersma et al, 1998; Reference Harrigan, McGorry and KrstevHarrigan et al, 2000; Reference Larsen, Moe and Vibe-HansenLarsen et al, 2000; Reference Malla, Norman and ManchandaMalla et al, 2002) and with improvement in the severity of negative symptoms (Reference Haas, Garratt and SweeneyHaas et al, 1998; Reference Harrigan, McGorry and KrstevHarrigan et al, 2000; Reference Larsen, Moe and Vibe-HansenLarsen et al, 2000). Unlike other investigators we did not find a significant association between DUP and positive symptom improvement in our regression model, but did find a weak relationship when DUP was analysed as a binary variable (Reference Loebel, Lieberman and AlvirLoebel et al, 1992; Reference Haas, Garratt and SweeneyHaas et al, 1998; Reference Harrigan, McGorry and KrstevHarrigan et al, 2000; Reference Larsen, Moe and Vibe-HansenLarsen et al, 2000; Reference Malla, Norman and ManchandaMalla et al, 2002).
This study helps to clarify our understanding of the relationship of DUP with outcome by simultaneously assessing and statistically controlling for other potential confounding prognostic indicators. These include diagnosis, premorbid function, age at onset, gender and symptom severity at baseline.
Implications for timing of treatment
The definitive clinical study to address the hypothesis that shorter DUP improves treatment responsiveness would involve the randomisation of first-episode patients to different lengths of treatment delay. Because such a study would not be ethical or feasible, evidence to support this hypothesis must be gleaned from naturalistic studies using correlational analyses, with the accompanying possibility that the observed relationships between DUP and outcome are confounded by yet other unmeasured factors. Within the methodological limits of this study, the finding that longer DUP is independently associated with treatment outcome supports the hypothesis that duration of initial psychosis is a potentially modifiable prognostic factor. The small to moderate effect sizes suggest that there are other, as yet unknown, clinically important factors affecting treatment responsiveness.
Determining the neurobiological explanation for the putative relationship between DUP and outcome could potentially guide the development of preventive strategies. Recent studies suggest that clinical progression in schizophrenia is associated with progressive loss of brain grey matter and ventricular enlargement (Reference Lieberman, Chakos and WuLieberman et al, 2001a ; Reference Cahn, Pol and LemsCahn et al, 2002; Reference Ho, Andreasen and NopoulosHo et al, 2003). It is as yet unknown whether earlier institution of antipsychotic treatment or long-term maintenance medication treatment will offer any protection against clinical or neurobiological illness progression and thus have an impact on long-term symptomatic and functional outcome (Reference Lieberman, Perkins and BelgerLieberman et al, 2001b ).
Premorbid function and outcome
The findings of this study are also consistent with the hypothesis that individuals with poor premorbid function might have an illness that is less responsive to antipsychotic treatment regardless of when it is instituted. Our findings are in agreement with most (Reference McGlashanMcGlashan, 1986; Reference Johnstone, Macmillan and FrithJohnstone et al, 1990; Reference Larsen, Moe and Vibe-HansenLarsen et al, 2000) but not all (Reference Robinson, Woerner and AlvirRobinson et al, 1999) previous studies that have examined the relationship between premorbid function and outcome. Theoretically, poor premorbid function could result from an early insult or disturbance that (subtly) disrupts normal brain development resulting in lower IQ, cognitive impairments, or decreased social capacity (Reference WeinbergerWeinberger, 1987). These initial deficits might lead to decreased social and educational opportunities that could magnify further the functional impairments over time (Reference Ott, Spinelli and RockOtt et al, 1998). Research is needed to develop primary prevention strategies that allow for early identification and effective targeted intervention for individuals in this potentially vulnerable group. For example, it is conceivable that (as yet unknown) treatment strategies could minimise or prevent pathological brain development in childhood and adolescence resulting from neurodevelopmental alterations in brain connectivity.
Duration of untreated psychosis and the treatment effect of typical and atypical antipsychotics
This study involves treatment with either haloperidol or olanzapine, and thus could be generalised directly to treatment with either of these two drugs. We did not find an interaction between drug randomisation and DUP effects, suggesting that DUP and premorbid function might influence response to typical as well as atypical antipsychotics.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Shorter duration of untreated psychosis and good premorbid function are independently associated with better response to antipsychotic treatment.
-
▪ Duration of untreated psychosis might be a potentially modifiable prognostic factor, supporting efforts to develop early intervention programmes.
-
▪ Poor premorbid function could indicate an illness that is less responsive to antipsychotic treatment regardless of when it is instituted.
LIMITATIONS
-
▪ Study participants consented to participate in a randomised double-blind clinical trial and so are not a naturalistic sample; thus, the results of this study might not apply to the general population of people with schizophrenia.
-
▪ Possible heterogeneity in study assessments in the multi-centre study may have increased measurement error and thus reduced the estimated effect magnitude of duration of untreated psychosis and premorbid function; controlling for study site minimised the risk of systematic bias.
-
▪ The correlational design of this study leaves open the potential for other unmeasured factors to confound the observed relationships.








eLetters
No eLetters have been published for this article.