Lithium is found naturally in variable amounts in food and water; and is widely and effectively used in pharmacological doses in psychiatry for the treatment and prevention of manic and depressive episodes. Mood disorders are characterised by a 30–50 times increased risk of suicide that can be reduced with lithium treatment. Reference Cipriani, Pretty, Hawton and Geddes1,Reference Baldessarini, Tondo, Davis, Pompili, Goodwin and Hennen2 Lithium has also been found to have an anti-suicidal property that might be independent from its mood-stabilising effect. Reference Müller-Oerlinghausen, Felber, Berghöfer, Lauterbach and Ahrens3 The recommended serum levels for lithium range between 0.6 and 1.0 mmol/l for maintenance therapy of bipolar disorder. 4 However, the optimal blood level at which lithium exerts a possible preventive effect against suicide has not been confirmed. In an ecological study in 1990, Schrauzer & Shrestha reported that the average suicide rates in 27 counties of Texas, USA, over a 10-year period, were consistently lower in counties with relatively high natural lithium content in the drinking water compared with those with medium or low content. Reference Schrauzer and Shrestha5 Recently, Ohgami et al examined lithium levels in tap water in the 18 municipalities of Oita prefecture in Japan, and correlated these with the standardised mortality ratios (SMRs) for suicide in each municipality. They found that lithium levels in tap water were significantly and negatively correlated with SMRs across that particular region in Japan. Based on this correlation, the authors hypothesised that lithium in drinking water may be associated with the risk of suicide in the general population. Reference Ohgami, Terao, Shiotsuki, Ishii and Iwata6 Since the publication of this report in 2009, there has been considerable debate in the scientific literature and print/electronic media regarding the possibility of adding lithium to drinking water supplies to benefit community mental health. The study, however, has been criticised for not accounting for potential confounding factors, ecological fallacy, methodology and interpretation of the findings. Reference Young7–Reference Huthwaite and Stanley11 To further test this hypothesis, we conducted an ecological study in the East of England to examine whether there was an association between naturally occurring lithium levels in drinking water and mortality from suicide.
Method
The East of England is one of the nine official regions of England, UK, and it is made up of six counties (Essex, Hertfordshire, Bedfordshire, Cambridgeshire, Norfolk and Suffolk), which are further divided into 47 subdivisions. In 2007, the population in each of the subdivisions in the East of England varied from 62 200 to 188 800, with a total population of 5.7 million (www.statistics.gov.uk).
We obtained indirectly SMRs of suicide (ICD-10 12 codes: X60–X84) for the period 2006–2008, for the 47 subdivisions of the East of England as reported in the NHS Clinical and Health Outcome Knowledge Base (www.nchod.nhs.uk).
We obtained drinking (tap) water samples from publicly accessible sources (restaurants, public toilets, pubs, cafeterias and petrol stations) in the 47 subdivisions. The samples were collected in 120 ml sterilised plastic containers provided by Eurofins UK (www.eurofins.co.uk). We obtained one water sample of 100 ml from each subdivision in the East of England. Sample containers were submitted for analysis within 48 h of collection. No specific storage requirements were advised by the laboratory. Lithium levels were measured by Eurofins UK, using inductively coupled plasma mass spectrometry. Collection of all water samples and analysis of lithium levels were performed in the calendar year 2010.
We used Pearson's correlation coefficient (r) and bivariate scatter plots to investigate the association between lithium levels in drinking water and suicide SMRs in the 47 subdivisions of the East of England.
Results
Overall, for the 3-year period 2006–2008 (pooled), the SMR for suicide in the East of England was 98, varying from 36 to 194 across all the subdivisions. The SMR in males was 95 (range 35–213) and in females 108 (range 0–292).
Lithium levels in drinking water ranged from <1 to 21 μg/l across the 47 subdivisions of the East of England. The distribution of these levels in this large geographical area revealed little or no variation if the water was supplied by the same company.
The analyses of these data showed that there was no correlation between lithium levels in drinking water and the suicide SMRs in the 47 subdivisions of the East of England (r = –0.054, P = 0.715 for males; r = 0.042, P = 0.777 for females; r = – 0.03, P = 0.838 for both genders). Similarly, the bivariate scatter plots showed no association between lithium levels in drinking water and the suicide SMRs (Fig. 1).
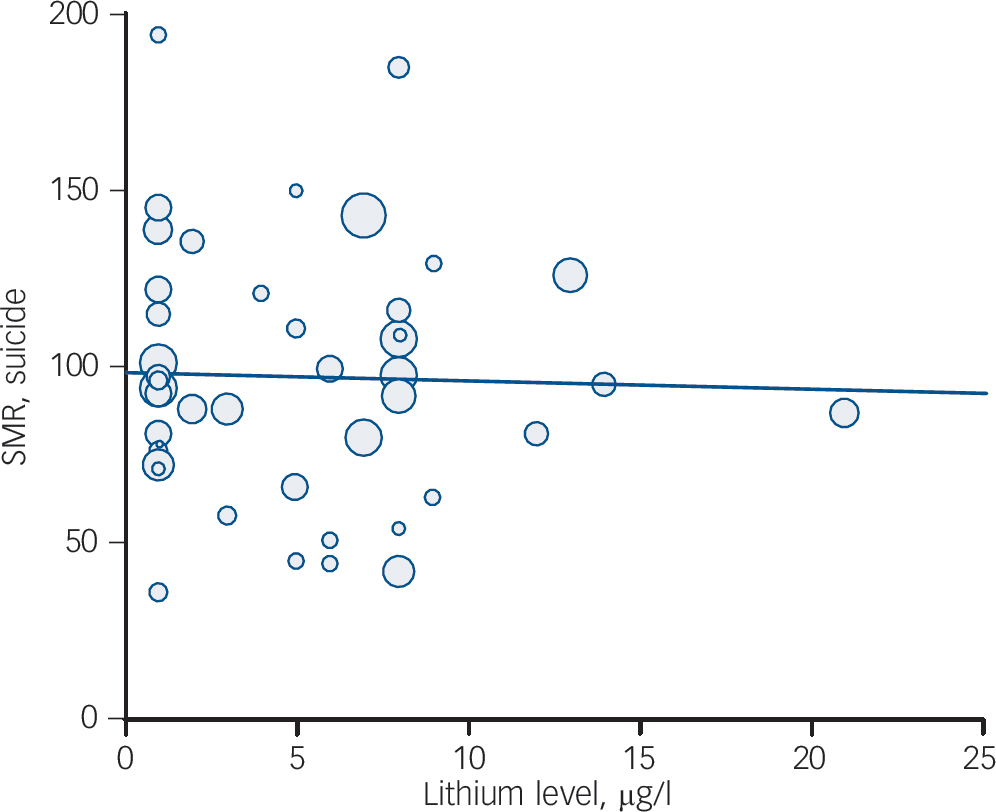
Fig. 1 Lithium levels in drinking (tap) water and standardised mortality ratios (SMRs) for suicide from 2006 to 2008 (pooled) in the 47 subdivisions of the East of England. The size of the dot represents population size in each subdivision.
Discussion
Contrary to the two previous studies (from USA in 1990 and Japan in 2009), we found no association between lithium levels in drinking (tap) water and mortality from suicide in the East of England, a region with a total population of 5.7 million. A variety of factors may have played a part in these differing results. For example, Ohgami et al weighted data by population sizes within the 18 municipalities of the Oita prefecture (population 1.2 million). Reference Ohgami, Terao, Shiotsuki, Ishii and Iwata6 It raises the possibility that the apparent negative correlation was perhaps as a result of a single measurement point, i.e. Oita city had the largest population (n = 463 973, 38%). In the East of England, there was relatively little variation in population size across the 47 subdivisions. Also, the lithium levels in drinking water in Texas and in the Oita prefecture ranged from 0 to 160 μg/l, and 0.7 to 59 μg/l, respectively. Reference Schrauzer and Shrestha5,Reference Ohgami, Terao, Shiotsuki, Ishii and Iwata6 These values represent a much wider range and higher top level than those found in the East of England (<1–21 μg/l). Accordingly, the normal distribution of serum levels of lithium in these populations might also differ, and be hypothetically responsible for the discrepancy between these results and the respective suicide rates.
All these populations could also differ with regard to ethnic, religious and social class distribution, prevalence and management of mental disorders and mobility patterns. In 2008, the East of England had one of the highest total net in-migration rates of all English regions, of which half was due to international in-migration (www.statistics.gov.uk). However, mobility patterns are unlikely to influence the regional suicide rates in the East of England, as an incident of suicide is only assigned to a particular subdivision if the individual has been resident in that subdivision for at least 6 months.
It is still not clear what amount of lithium in human serum can provide an independent protective effect for suicide. The naturally occurring serum levels of lithium in adults range between 7 and 28 μg/l (0.001–0.004 mmol/l); Reference Schrauzer13 nonetheless, the supposedly preventive therapeutic level to prevent suicide has only been tested with serum levels that are considered effective for prevention of relapse in mood disorders (0.6–1.0 mmol/l). Reference Cipriani, Pretty, Hawton and Geddes1,Reference Baldessarini, Tondo, Davis, Pompili, Goodwin and Hennen2,4
Drinking water is not the only dietary source of lithium. According to the US Environment Protection Agency, some grains and vegetables are much richer in lithium than drinking water. Moreover, daily lithium intake oscillates between 650 and 3100 μg in adults. This means that drinking water can only be a minor contributor to lithium consumption in humans. Reference Schrauzer13
Implications
Further studies are required to relate specific dietary lithium consumption to expected serum lithium levels, as well as to ascertain at what range or threshold, if any, lithium could prevent suicidal behaviour at the population level. Future research may also benefit from accounting for other variables associated with possible variations in suicide rates, for example sociodemographic characteristics or standards of care for people with mental disorders, specifically mood disorders, in each particular geographical area.




eLetters
No eLetters have been published for this article.