Despite a steady decline in the use of lithium over the past decade, lithium treatment remains a major cause of negligence claims in the care of patients with psychiatric disorders. Lack of regular lithium monitoring, the use of interacting medications and failures in communication are the major problems. Damages of some £600 000 were awarded in a case in 1999 in which a patient on lithium had an interaction with other prescribed drugs, resulting in toxicity and damage (Medical Protection Society, Personal Communication, 2002). In that case the patient received lithium from secondary psychiatric care and received interacting non-steroidal anti-inflammatory drugs from a general practitioner (GP). This kind of scenario is not uncommon and presents a significant risk to this patient group.
Monitoring patients on lithium is usually not a complex technical task and the broad parameters of how it should be conducted have been established for many years (Reference KehoeKehoe, 1992). What, however, has sometimes been lacking is a systematic means of ensuring that patients are safely, consistently and efficiently monitored in the setting most appropriate to their needs (Reference RymanRyman, 1997). Many clinicians and geographical areas have local systems that promote good practice, but unfortunately few have effectively bridged the communication gap that can occur between a patient's psychiatrist and the general practice that provides most patient prescriptions and medical care. Differences in individual psychiatrists' approaches may also generate confusion for GPs. Such factors perpetuate the liability for ongoing problems and litigation.
Background
Although there has been a general explosion in the number of guidelines available, there have been no major guidelines produced to facilitate good practice with lithium. In Lothian we were unable to find a regional- or hospital-based guideline. A recent initiative across Lothian involved GPs being asked to create registers of patients on lithium and to audit the monitoring of their lithium. Unsurprisingly, when GPs were asked to submit guidelines on how practices intended to monitor these patients, over 50 guidelines of varying shape, size and form were submitted. Clinical governance highlights the need to assess the clinical effectiveness of our practice and to engage in risk management. The development of a Lothian-wide guideline for the monitoring of lithium treatment was thought to be a useful step towards facilitating improved standards of care for this patient group. A multi-disciplinary working party was established.
The aims of the working party were to:
-
(a) develop a systematic approach that would enable both psychiatrists and GPs to provide safe, effective and consistent management of patients who have lithium prescribed;
-
(b) ensure the transfer of key information and continuity of care as patients moved across the interface between secondary psychiatric care and primary care.
Method
A working group was established in November 1999 consisting of representatives from psychiatric service user groups, general practice, psychiatry, hospital- and community-based pharmacists, community psychiatric nursing, clinical chemistry and information technology departments. Input was available from hospital drug and therapeutics, GP prescribing and GP sub-committees, and our local clinical guidelines group (a subgroup of Lothian Primary Care Trust's Clinical Governance Support Team).
The literature was searched for relevant guidelines and completed audits of lithium prescribing using Medline, Embase and PsychINFO through the Ovid interface. Subject headings used included lithium and either guidelines or audit. In addition, communication with lithium clinics and specialist centres nationally provided an informed context from which the group could start to develop a guideline. This was undertaken by one of the authors (J.N.), who also coordinated the meetings with all parties. The large group met on five occasions. There were a number of smaller meetings among the authors and the clinical guidelines coordinator to maintain a momentum between larger meetings and to compose the draft wording and layout of the document. The priority was to produce a document, written in plain English, that provided clarity and consistency while avoiding confusing detail.
The key areas of debate for the group were the frequency of serum lithium checks, the extent and frequency of assessment of renal function and the desirable therapeutic range of serum lithium levels. Although the group appreciated that often there was no extensive evidence base available to support their decisions, the group was keen to provide clear guidance that supported good practice. It was also necessary to liaise with specialists outside of the group (e.g. renal physicians). Ultimately, the agreement to the final document was forged with all interested parties.
Outcome
The Lothian lithium guidelines include a lithium treatment plan (see Fig. 1); advice for clinicians on managing patients' lithium levels; and pointers for counselling patients on lithium (to be used in conjunction with a patient information leaflet).
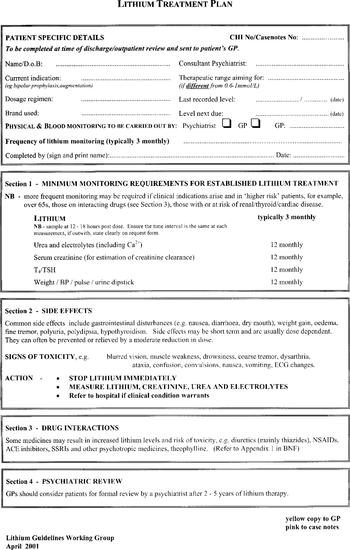
Fig. 1. Lithium treatment plan (the plan is a duplicate — two copies: one yellow and one pink). This fig. may be copied freely.
The lithium treatment plan is a key document in the guidelines. The section requesting the patient-specific details highlights the key information that needs to be clearly communicated at all times. It will alert GPs to any difference from typical monitoring in an individual patient. The information required is fairly basic (e.g. treatment indication, dosage, desired therapeutic range, brand of lithium preparation and the frequency of serum lithium levels to be carried out and by whom) but currently this information is not always available to GPs. A particular concern is to make clear who is responsible for the future physical monitoring of the patient. As a result, patients should neither receive an excessive number of tests from a variety of sources, nor have fewer tests than are recommended.
The lithium treatment plan is completed by the psychiatric team and a copy is sent to the GP following a patient's discharge from hospital, and also at appropriate out-patient reviews (e.g. at initiation or re-introduction of treatment, dosage alteration and side-effect investigation). The lithium treatment plan also includes sections on minimum monitoring requirements for established lithium treatment; side-effects; drug interactions; and psychiatric review. Part of the physical monitoring requirements is an annual serum creatinine to estimate creatinine clearance using the Cockcroft and Gault equation (Reference Cockcroft and GaultCockcroft & Gault, 1976) (see Box 1).
Box 1. Cockcroft and Gault (Reference Cockcroft and Gault1976) equation
 \batchmode \documentclass[fleqn,10pt,legalpaper]{article} \usepackage{amssymb} \usepackage{amsfonts} \usepackage{amsmath} \pagestyle{empty} \begin{document} \(\mathrm{creatinine\ clearance}\left(\frac{\mathrm{ml}}{\mathrm{min}}\right)=\frac{\mathrm{F}{\times}(140-\mathrm{age}){\times}\mathrm{weight\ (kg)}}{\mathrm{serum\ creatinine}\left(\frac{{\mu}\mathrm{mols}}{\mathrm{l}}\right)}\) \end{document}
\batchmode \documentclass[fleqn,10pt,legalpaper]{article} \usepackage{amssymb} \usepackage{amsfonts} \usepackage{amsmath} \pagestyle{empty} \begin{document} \(\mathrm{creatinine\ clearance}\left(\frac{\mathrm{ml}}{\mathrm{min}}\right)=\frac{\mathrm{F}{\times}(140-\mathrm{age}){\times}\mathrm{weight\ (kg)}}{\mathrm{serum\ creatinine}\left(\frac{{\mu}\mathrm{mols}}{\mathrm{l}}\right)}\) \end{document}
|
| Where F=1.23 (male) and F=1.04 (female) |
| This calculation has limitations in some patient groups, for example those who are obese, elderly, emaciated or oedematous. |
The Guidelines for the Management of Patients on Lithium (Guideline Working Party, 2001) were launched in May 2001 with input from the Clinical Guidelines Support Team. They are available to GPs and mental health services as part of the Lothian Health Clinical Guidelines folders. They are also available on the Lothian Primary Care NHS Trust website (http://www.nhslothian.scot.nhs.uk/primarycarelibrary/2_ClinicalPractice/2_Guidelines&SCPs/Guidelines/Lithium.pdf).
Discussion
We are hopeful that the guidelines will be widely used locally and believe there is enough flexibility within them to encompass most clinicians' current style of practice. Achieving agreement among psychiatrists is rarely a foregone conclusion. It is perhaps useful to highlight the issues on which we think considerable progress and agreement was made.
Concerns have been raised about the difficulties in reliably monitoring renal function in patients on long-term lithium. Conventional wisdom has generally been to annually collect a 24-hour urine sample for estimation of creatinine clearance. Most patients and their GPs have found this to be a cumbersome process and concerns are often raised about the reliability of such estimates in patients with psychiatric disorders. Tests often require repetition and abnormal results are difficult to interpret.
After lengthy discussion we recommended estimating creatinine clearance using the Cockcroft and Gault equation (Box 1). Such estimates would be more readily available on all patients. As this is a new departure locally we will be alert to any impact this has on the incidence and nature of renal problems associated with lithium. Concerns about significant changes in clearance still require more specialist investigation of renal function.
Few disagree that lithium levels should be monitored every 3-6 months, except in higher-risk patients. The group, however, felt that such a recommendation is vague and could be unhelpful. The group felt that serum lithium levels should be typically checked every 3 months. It was accepted that this is a statement of best practice rather than an evidence-based recommendation.
Similarly the ideal therapeutic range for serum lithium levels has often been debated. Locally and nationally we found there were variations in what psychiatrists typically recommended for patients. Some advocate a range of 0.4-0.8 mmol/l as preferable to a range of 0.6-1.0 mmol/l. No clear evidence base suggests superiority of one over the other. Our local laboratories' reference ranges have been the latter for many years so it was decided to leave this unchanged at present, while emphasising the choice of range remains with individual psychiatrists.
Conclusion
This development has provided the opportunity for primary and secondary care services to work together in producing a guideline that will facilitate good practice. It is likely to improve patient care, minimise risk and underlines the move towards ‘partnership-working’ across this interface. Liaison with our information technology departments will ensure our document templates can be integrated into local systems. Audit and review of the use of these guidelines are both essential to ensure this endeavour has any clinical impact. In response to this development the Lothian lithium audit was initiated in July 2001 by the Primary Care Clinical Governance Support Team. The aim of the audit is to identify current management of patients on lithium and support practices to implement any changes in line with the Lothian lithium guidelines. Results from the first phase baseline audit have been collated and an interim report disseminated. The full report (which will include the re-audit data) will be available for dissemination in September 2002 and will inform the review of these guidelines.
Such ‘joined-up thinking’ is indeed fashionable at present but there will be some who are sceptical about the value of such exercises. At the very heart of this is often an ambivalence to guidelines in general. There can be worries that overly simplified or prescriptive approaches are inappropriate and unhelpful. Furthermore, there are concerns that failure to adhere to guidelines may increase clinicians' and trusts' liability to allegations of negligence. However, current thinking suggests that failure to produce and consult guidelines would be a far greater omission of care. We are certainly hopeful that this guideline in conjunction with local audits and registers of patients on lithium in general practice will make a valuable contribution to improving the health care provision for these patients. Ultimately it may also reduce costs within NHS psychiatry too.
Declaration of interest
None.
Acknowledgements
We would like to thank the members of the Lithium Guidelines Working Group, in particular Professor Klaus Ebmeier, University of Edinburgh, and Jayne Burnett, the Lothian Primary Care Trust's Clinical Guidelines Coordinator. We would also like to thank the Medical Protection Society for providing us with information on the medico-legal cases involving lithium.





eLetters
No eLetters have been published for this article.