What is a carers’ clinic?
Heroin addiction is a chronic condition that, more often than not, adversely has an impact on those caring (family, partners and/or friends) for the addict. However, the information and support needs of carers often go unrecognised and unaddressed. Feelings experienced by carers include guilt, shame, anger and loss of control. This devastating impact is well acknowledged and is in turn reflected in various government and National Treatment Agency policy documents - all recommending the need to provide information and support for carers. However, this does not always translate from rhetoric into practice. Hence, we set up the carers’ clinics in April 2007, at The Bridge substance misuse service. This is primarily an information-sharing and support group for carers of heroin addicts who are receiving treatment from our drug service.
Why was it set up?
There were several reasons for setting up the first carers’ clinics. First, the compelling evidence base: research has shown that carer needs include information, support, contact with other carers and an empathic, non-judgemental approach. 1 It has also been found that provision of support for carers of substance misusers can result in better engagement and retention of users in treatment and even a better treatment outcome. Reference Copello, Velleman and Templeton2 Second, in our clinical work with heroin addicts, we were increasingly coming across carers who asked for more information regarding various aspects of their loved ones’ care and treatment. Finally, one of the authors learnt from his own experience as a carer that ‘quality time’ to answer his queries with the treating consultant was limited - resulting in significant emotional burden and poor satisfaction with treatment.
Our aims in setting up these clinics were twofold: to give carers the chance of quality time with the consultant to get accurate answers to their queries (information giving/sharing), in an informal and non-judgemental setting; and to give carers the opportunity to share their experiences and support each other.
How is it run?
The clinics take place at The Bridge Substance Misuse Service, part of Birmingham and Solihull Mental Health NHS Foundation Trust. The Bridge is commissioned by The Solihull Partnership on behalf of the Solihull Care Trust and offers treatment services to misusers of Class A drugs living in Solihull.
Setting up the clinics
The clinics run on the second Thursday of every month, from 19.00 to 21.00 h. We allow half an hour from 18.30 to 19.00 h for carers to have the time to arrive, have a chat and some refreshments before the session formally starts at 19.00 h. Many carers utilise this time to catch up with each other or have a quick word with the consultant or other staff at The Bridge. The evenings are advertised through word-of-mouth, individual flyers sent to carers, posters and other displays in reception. Between 8 and 18 carers attend each session and some ex- and current drug users (who come in with their carers) also attend some of these sessions. The sessions are jointly facilitated by the consultant (S.G.) and the team manager (S.B.). Although we aim to end the meetings by 21.00 h, some carers spend time with the consultant (one to one) afterwards, or even arrange for one to one meetings at a later date. Some users and carers also arrange for joint meetings with the consultant outside these sessions.
Format of the clinics
The session starts with an offer for all participants to say their name or give more information if they wish. We agreed at the outset that any contribution to the meeting would be voluntary and in some instances it has taken several sessions before carers felt ready to start speaking. When we have new members we restate the purpose of the group and clarify the ground rules (particularly emphasising patient confidentiality aspects), which are agreed with the whole group at the beginning.
We then introduce the topic for the session that has been chosen by participants at the previous meeting. Where carers have requested a formal input from the consultant on a specific topic, the session starts with a short 10 min presentation. Some of the topics discussed so far have included management of heroin overdose, polysubstance misuse, how methadone and subutex (opiate substitutes) work, blood-borne viruses, cannabis and mental health, relapse prevention and treatment effectiveness. The atmosphere is very relaxed and every opportunity is taken to encourage carers to share their own knowledge and experience. We deliberately keep the meetings as informal as possible while making sure that all carers who want to do so get the chance to speak.
Some of the sessions can be very moving: there is a mixture of tears, laughter and the incredible bravery of people who feel safe enough to share their suffering with each other. Some sessions are more intense than others; what is constant is the mutual support for carers and the way participants respect each others’ viewpoints. There is real active listening and the closeness of the group is tangible. The mix of medical expertise on offer and the facilitators’ gentle reassurance coupled with the first-hand experience of carers (and sometimes users) can be immensely powerful.
The facilitators conclude with an attempt to recap on the session and ask participants to agree a topic for the next month. Even after the session is over, invariably the meeting continues informally in the room, in the corridor and outside: carers’ reluctance to part at the end of the night is real proof of the huge need they have to share the difficulties they are experiencing with others in the same situation, with the safety of accurate and empathic medical information and support. A summary of the key features of these clinics is given in Box 1.
Illustration of a session
We think it will be useful to briefly describe one actual session, to clarify better what these sessions are all about. One of the recurring questions from the participants has been about treatment effectiveness: do treatments work? We offered this as the topic of one of the sessions. We (S.G. and S.B.) started with a short explanation of the theories of behaviour change. We then encouraged the group to think of examples of improvements in drug use and to identify treatment goals. We explained the various treatment interventions, pharmacological and psychological, and the evidence for their effectiveness. The aim of the session was twofold: to give accurate answers to the specific questions carers have about treatment, but also to encourage them to share their own experiences, identify what has worked or not for their loved ones and support each other in making plans for the future. Like all our sessions, this was about debunking myths, about acknowledging the difficulty and the pain involved in helping drug users to change, and about sharing practical tips on how to cope. At the end of the session carers said they wanted the opportunity to talk to someone who had successfully completed their treatment. In the following session we arranged for an ex-user to come and share their ‘story’ and this was deeply moving for all participants.
Box 1. Key features of clinics
Structure of sessions
Venue: The Bridge substance misuse service, Solihull
Time:19.00-21.00 h
Frequency: monthly (second Thursday of every month)
Number of attendees: range from 8 to 18
Facilitators: consultant (S.G.) and team manager (S.B.)
Refreshments on offer at start and during the session
Format of sessions
Introductions
Brief recap of scope and purpose
May or may not start with a 10-minute presentation on a specific topic (chosen by the group)
Questions and answers/discussion
Sharing of experiences
Facilitators’ concluding remarks and agree on topic for next session
Is it useful?: the carers’ perspective
Levels of satisfaction
We carried out two questionnaire surveys, in July 2007 and March 2008, to evaluate the carers’ clinics. The same questionnaire was used on both occasions: it consisted of seven questions. Questions one to six assessed carers’ levels of satisfaction (rated on a scale of 1-10) with the venue, time, duration, content, format and frequency of the sessions. Question seven asked for ‘any other comments?’
We had 12 responses in July 2007 and 18 in March 2008. Figure 1 summarises the results. Scores of nine or above were taken to mean that the rater was very satisfied on that item - this is represented as percentages (of satisfaction levels) in Fig. 1.
Carers’ comments
Carers appreciate the chance to address their concerns openly in a supportive and trusting environment. The sessions provide a source of considerable emotional support and a learning environment. Given below is a selection of responses of carers to question seven (‘any other comments’).
-
• ‘This “special place” has been a great help to many people, users, families, friends. Everyone here has all the time in the world for you and it makes you feel like you’re getting somewhere.’
-
• ‘Because of the friendly, kind and non-judgemental approach, everyone has found the courage to attend the carers’ clinics sessions and benefit enormously. We have the opportunity to ask questions, discuss our experiences and fears, and we are given truthful answers and advice. Caring for an addict isn't easy; when someone you love is out of control and chaotic, it is very frightening, for you and them. Learning about addiction and meeting regularly with others who have similar experiences helps to alleviate your distress.’
-
• ‘You don't feel alone.’
-
• ‘Other people look down on people like us; it is so isolating to look after a drug user. Here, we are all in the same boat. I get answers to questions and see how others perceive the topics.’
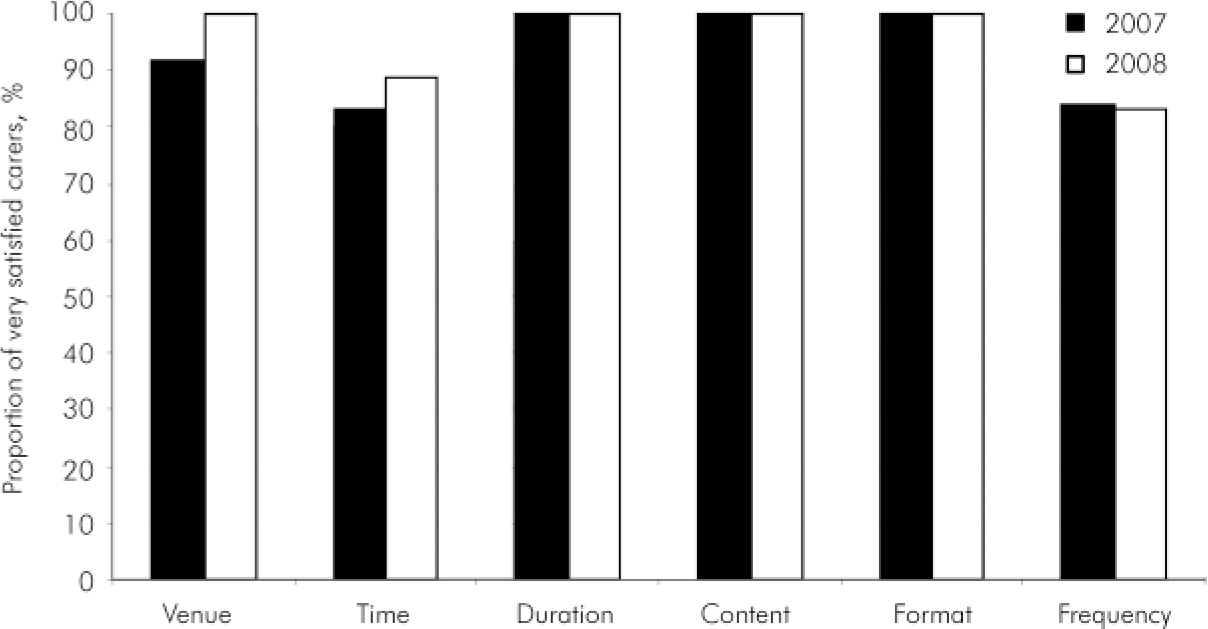
Fig. 1. Carers’ levels of satisfaction with clinics in 2007 (n = 12) and 2008 (n = 18).
The future
Given the very positive feedback and the enthusiastic attendance of many carers, we intend to continue this service provision. The group is currently working on producing an information leaflet for carers of heroin misusers. There are also plans to roll out this initiative across other services in the Trust. Leading on from these clinics, we hope to get carers more involved in various aspects of the service - development, training and research. We also plan to use these clinics to ensure our service is user and carer friendly, and sensitive to their needs. All in all, we believe that this simple yet innovative attempt at effectively addressing carer needs can easily be replicated across other services.
Declaration of interest
S.G., S.B. and H.J. jointly organise, and S.G. and S.B. facilitate these sessions. They offer their time voluntarily.
Acknowledgements
We thank all carers and users who have attended carers’ clinics and consented to this publication.




eLetters
No eLetters have been published for this article.