First identified in December 2019, the SARS-CoV-2 virus rapidly spread across the globe leading to a worldwide pandemic. Early on, New York City saw one of the highest rates of infection. 1 In severe cases of acute COVID-19, the disease is associated with myocardial injury and arrhythmias not directly due to the acute respiratory distress seen in a majority of hospitalised patients. Reference Kochi, Tagliari, Forleo, Fassini and Tondo2 In comparison to adults, children tend to have a milder disease course. In a large case series of 2,143 children diagnosed with laboratory-verified or clinically diagnosed COVID-19, over 90% had asymptomatic, mild, or moderate disease. Reference Dong, Mo and Hu3
Most of the paediatric research in relation to SARS-CoV-2 and myocardial disease revolved around multisystem inflammatory syndrome in children (MIS-C), a compilation of symptoms that arise shortly after the acute phase of infection with SARS-CoV-2, with strong evidence of cardiac injury in a majority of these patients. Reference Jiang, Tang and Levin4 One recent study of 186 patients with MIS-C found that 80% had cardiovascular involvement, including conditions such as coronary artery aneurysm, pericarditis, cardiac arrhythmia, and need for vasopressor support. Reference Feldstein, Rose and Horwitz5
In adults, many patients have shown evidence of continued cardiac effects past the acute phase of illness. Reference Puntmann, Carerj and Wieters6 These findings have led to recommendations for obtaining follow-up testing for adults planning to return to sports if they have symptomatic COVID-19 disease. Reference Wilson, Hull and Rogers7–Reference Dores and Cardim9 However, in the paediatric population, there is a paucity of data to drive recommendations for follow-up testing, especially for the majority of children with asymptomatic or mild COVID-19.
This study focuses on children with a history of SARS-CoV-2 infection who had asymptomatic or mild COVID-19 not requiring hospitalisation and were subsequently evaluated by cardiology. It aims to add to the information known about the implications of SARS-CoV-2 on the paediatric heart, specifically in regard to the potential for coronary artery dilation, similar to what is seen in patients with MIS-C.
Methods
We identified patients through our COVID-19 institutional data repository which contains electronic patient data for all COVID-19 patients at our institution and through a search of the electronic medical record. We queried the electronic medical record for patients ≤ 18 years of age who were referred to paediatric cardiology due to a history of SARS-CoV-2 infection between 5/2020 and 4/2021. We identified patients if they had a COVID-19 test performed (polymerase chain reaction or antibody), a COVID-19 diagnosis (ICD10 U07.1), or mention of COVID-19 in the chief complaint of their cardiology visit. We excluded patients who did not have confirmatory COVID-19 testing (either polymerase chain reaction, antigen, or antibody), had been hospitalised for any disease related to SARS-CoV-2 including MIS-C, or who had a history of cardiac disease that could affect coronary artery dimension (i.e., Kawasaki disease), history of surgical correction of CHD involving the coronary artery, history of CHD unless fully repaired, and history of arteritis potentially involving the coronary artery. For eligible patients, we conducted a chart review with data extraction using REDCap Reference Harris, Taylor, Thielke, Payne, Gonzalez and Conde10 (Research Electronic Data Capture), a secure web-based application used for database management. We collected information on the documented SARS-CoV-2 infection, including testing and symptoms, electrocardiogram and echocardiogram findings, and any additional laboratory test results available from either the paediatric cardiology visit or a preceding emergency department visit. Coronary artery dilation on echocardiogram was defined as the Boston Z-score greater than 2.0. Reference Colan11
Results
We reviewed 317 charts, yielding 157 patients who met inclusion criteria (Fig. 1). The mean age was 9.4 years (+/– 5.4 years) with 87 (55%) males. Patients were generally healthy, with asthma and allergies being the most common comorbid medical conditions. We identified 84 (54%) patients having COVID-19 diagnosed via a positive antibody test, 50 (32%) via PCR, 2 (1%) via rapid antigen testing, and 21 (13%) with a positive test that was not defined further in the electronic medical record (Table 1). All patients underwent electrocardiogram and echocardiogram as part of their paediatric cardiology evaluation. We found 135 (86%) patients with a normal electrocardiogram and echocardiogram, or only a minor variant on electrocardiogram, while 22 (14%) patients had abnormalities on echocardiogram. Minor electrocardiogram abnormalities included findings of right or left axis deviation and /or first-degree atrioventricular block. We identified four patients with coronary artery dilation on echocardiogram and found additional abnormalities in eight patients consistent with known underlying heart disease or incidental findings such as mitral valve regurgitation or patent foramen ovale (Table 2).

Figure 1. Flow diagram demonstrating the chart review process and final number of electrocardiogram and echocardiogram abnormalities.
Table 1. Clinical characteristics of patient population.

* n does not equal 157 as some patients had more than one of the diagnoses.
Table 2. Details regarding four patients with coronary artery dilation.
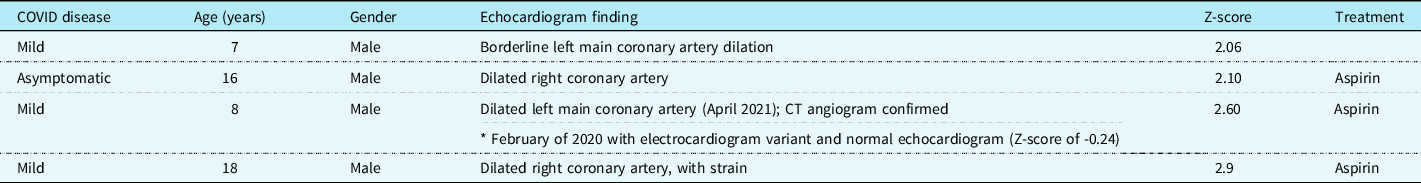
Patients with coronary artery dilation are described in detail here: (1) a 7-year-old male had a history of mild symptomatic COVID-19 with borderline left main coronary artery dilation with a Z-score of 2.06. Although follow-up was recommended, he did not return.
(2) A 16-year-old male had positive surveillance Sars-CoV-2 serology without symptoms of COVID-19, with a dilated right coronary artery with a Z-score of 2.10. On 1-month follow-up from his original visit, he had no change in his coronary artery dilation.
(3) An 18-year-old male had a history of mild symptomatic COVID-19 with a dilated right coronary artery with a Z-score of 2.9, also found to have decreased myocardial strain on echocardiogram. Although follow-up was recommended, he did not return to paediatric cardiology, although he continues to receive primary care at our institution with no further concerns.
(4) An 8-year-old male had previously been seen by paediatric cardiology in February 2020 with a normal echocardiogram, including normal coronary artery dimensions, with a Z-score of -0.24. He was evaluated in April 2021 due to chest pain after mild symptomatic COVID-19 and was found to have new dilation of the left main coronary artery, with a Z-score of 2.60, confirmed on CT angiography (Fig. 2). He had a repeat echocardiogram in November 2021, showing normalisation of his coronary artery dimension with a Z-score of 1.9.

Figure 2. Cardiac imaging of patient with normal echocardiogram prior to COVID-19 infection and coronary artery dilation after a ) normal left main coronary artery dimension (2.8 mm; z = 0) on routine echocardiogram 9 months before COVID-19 infection. b ) Dilated left main coronary artery (4.2 mm; z=+2.6) 5 months after COVID-19 infection. c ) CT angiography 10 days after B, showing dilated left main coronary artery (4.2 x 4.6 mm).
Discussion
Cardiac dysfunction is well defined in adult and children with moderate to severe COVID-19 and MIS-C. Cardiac manifestations of COVID-19 and MIS-C include myocardial inflammation, ventricular dysfunction, conduction abnormalities and arrhythmias, coronary artery dilation, symptomatic heart failure, and shock. Reference Kochi, Tagliari, Forleo, Fassini and Tondo2,Reference Feldstein, Rose and Horwitz5,Reference Maron, Udelson and Bonow12 Myocarditis has been described as the most common cardiac manifestation, stemming from direct myocardial injury from inflammation. Reference Kochi, Tagliari, Forleo, Fassini and Tondo2,Reference Wu and Campbell13 Markers such as troponin and brain natriuretic peptide can document myocardial damage, help predict the severity of disease, and guide treatment. Reference Kochi, Tagliari, Forleo, Fassini and Tondo2,Reference Feldstein, Rose and Horwitz5,Reference Wilson, Hull and Rogers7 However, there is little to no information delineating the risk of cardiac complications from asymptomatic or mildly symptomatic COVID-19 infection in children, which comprise the majority of the paediatric cases. Reference Dong, Mo and Hu3
One of the most pressing questions for parents and paediatricians is the safety for children to return to regular activities, including competitive sports, following COVID-19 infection. As myocarditis has been found to be a complication of COVID-19 and myocardial injury and is more likely in severe cases of COVID or MIS-C, attention has centred on the possibility of myocarditis in patients with severe disease. The current American Academy of Pediatrics guidelines stratify follow-up and work-up based on severity of illness and cardio-pulmonary symptoms. 14 Cardiac clearance criteria for severe cases of COVID-19 and MIS-C mirror those recommended for other forms of myocarditis. Reference Dores and Cardim9,Reference Maron, Udelson and Bonow12,Reference Dean and Paridon15 Return-to-play guidelines for mild COVID-19 infections are more informal, with no stated criteria for asymptomatic infection.
In this study, we found 4 of 157 (2.5%) children with a history of asymptomatic or mild COVID-19 disease without MIS-C to have some degree of coronary artery dilation. It is important to note that given the sample size, statistically it would be expected that 2.3% of this population would have a Z-score greater than 2, meeting the definition for coronary artery dilation. Although it may be too early to understand the future significance of this finding, these patients continue to follow with paediatric cardiology to determine whether there is progression or persistence of coronary artery dilation, development of coronary aneurysm, or development of late complications.
Most notable is patient 4, an 8-year-old male who had an echocardiogram demonstrating normal coronary artery dimensions prior to his COVID-19 infection. Approximately 10 months following his initial evaluation, and 5 months after he experienced mild symptomatic COVID-19, he had a paediatric cardiology evaluation for chest discomfort and was found to have dilation of the left main coronary artery, with a Z-score of 2.6, confirmed on CT angiography. On follow-up, he had improvement in the coronary artery dilation with a Z-score of 1.9. This course is in line with scant prior literature showing coronary artery dilation and resolution following MIS-C. Reference Farooqi, Chan and Weller16
Our study of a cohort of children with a history of asymptomatic or mild COVID-19 found an incidence of coronary artery dilation near expected for the general population. As mild and asymptomatic COVID-19 infection has become common in the paediatric population, routine echocardiographic surveillance does not appear to be feasible nor necessary. However, our report of mild coronary artery dilation following mild or asymptomatic COVID-19 in children may provide guidance for conservative management of similar cases in the future.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Competing interests
None.







