Congenital junctional ectopic tachycardia is a rare arrhythmia that occurs in patients without previous cardiac surgery. This is often refractory to medical therapy and associated with high morbidity and mortality. Reference Tulino, Dattilo, Tulino, Marte and Patanè1
In this report, we wanted to present a 6-hour-old newborn with congenital junctional ectopic tachycardia resistant to conventional anti-arrhythmic medications, who was successfully treated with ivabradine and amiodarone combination.
Case
A six-hour-old newborn girl was hospitalised in neonatal ICU because transient tachypnoea of the newborn. She was monitorised with noninvasive ventilation and cardiac monitoring. In her 6th hour, tachycardia was noticed. Her heart rate was 170/min, she was afebrile, and her blood pressure was 70/40mmHg. The electrocardiogram showed supraventricular tachycardia (Fig. 1). Intravenous adenosine 100 mcg/kg was given twice but no change in heart rate. Then, patient was consulted to paediatric cardiology. Paediatric cardiology reported that there was an evidence of atrioventricular disassociation, and a diagnosis of congenital junctional ectopic tachycardia was made (Fig. 2a). Transthoracic echocardiography revealed a structurally normal heart. In the meantime, heart rate of the patient increased to 200/min. Intravenous esmolol 500mg/kg was loaded; however, the rhythm was resistant. Then, the respiration of the patient got worse and hemodynamically instable despite noninvasive ventilation; therefore, the patient was intubated. Synchronised direct cardioversion was applied firstly with 0,5 j/kg; then 1 j/kg. at first heart rate got slower but then it increased again. Intravenous amiodarone 10mg/kg was loaded followed by a maintenance dose of 5mcg/kg/min. The heart rate was decreased from 200 to 160/min but still junctional ectopic tachycardia rhythm continued. We have added propranolol (2mg/kg/day) to the treatment and followed patient for 2 days. On the fourth day, junctional ectopic tachycardia rhythm still persisted; therefore, ivabradine 0.05mg/kg/dose twice was added to the treatment. On the following day, the heart rhythm was slowed to 110/min, and propranolol was stopped; intravenous amiodarone treatment was changed to the oral form. The rhythm turned into normal sinus rhythm; two days after starting ivabradine treatment (Fig. 2b). She was extubated on the 4th day of hospitalisation, and she was discharged on the 7th day with oral ivabradine and amiodarone treatment.

Figure 1. The electrocardiogram showing supraventricular tachycardia.
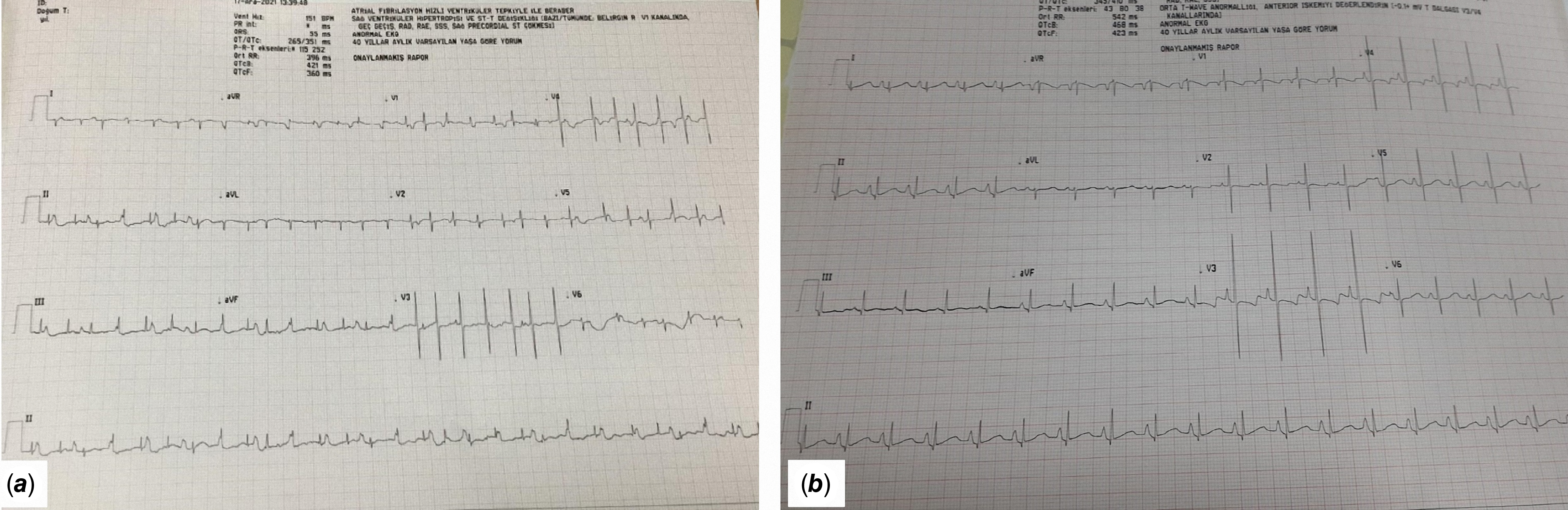
Figure 2. a : The electrocardiogram showing atrioventricular disassociation. b : Normal sinus rhythm after ivabradine treatment.
Discussion
Tachyarrhythmia originating in the atrioventricular node and atrioventricular junction including the bundle of His complex are called junctional tachycardia or junctional ectopic tachycardia. The types of junctional ectopic tachycardia based on their aetiology are congenital, postoperative, and focal paroxysmal and non-paroxysmal forms and those associated with digitalis toxicity. Reference Tulino, Dattilo, Tulino, Marte and Patanè1,Reference Kean, Hazle, LaPage, Bromberg and Macdonald2 Most common form is postoperative junctional tachycardia; its incidence is 5%. Reference Josephson and Josephson3 Congenital junctional ectopic tachycardia is a rare phenomenon, and it is mostly resistant to the conventional medical treatment. Our case was resistant to multiple medications like adenosine, esmolol, amiodarone. Furthermore; junctional ectopic tachycardia persisted despite cardioversion.
Ivabradine is a new anti-arrhythmic agent with direct inhibition of the pacemaker current. It has been used extensively to decrease sinus rate in the treatment of cardiac failure. In 2013, it was firstly used for congenital junctional ectopic tachycardia of a 3-year-old girl. It was used for the tachycardia which was resistant to sotalol and flecainide treatment; sinus rhythm was restored through ivabradine at 2.5 mg/day. Reference Al-Ghamdi, Al-Fayyadh and Hamilton4 In 2016, Dieks et al. Reference Dieks, Klehs, Müller, Paul and Krause5 reported 5 patients with Junctional ectopic tachycardia rhythm. Ivabradine successfully achieved sinus rhythm in 4 of 5 patients. The authors also showed that left ventricular functions normalised in all three patients with impaired left ventricular function. Furthermore, no side effect was reported in any of these patients. Kothari et al. Reference Kothari, Kidambi and Juneja6 reported the two siblings (2 months and 2 years old) whose congenital ectopic tachycardia was managed with ivabradine. Left ventricular function was deteriorated in both siblings, and the rhythm cannot be controlled despite combination therapy. After ivabradine therapy, both the rhythm and left ventricular function were normalised. Ergul et al. Reference Ergul, Ozturk, Ozgur, Ozyurt, Cilsal and Guzeltas7 reported three infants with refractory congenital junctional ectopic tachycardia despite multiple anti-arrhythmic treatments. The authors have emphasised that rhythm was turned to the normal so rapidly after adding Ivabradine to the treatment. Haemodynamics and clinical response were so satisfactory. However, the authors have emphasised that ivabradine as monotherapy may not be as effective as in combination therapy.
Conclusion
This report is to improve the awareness of the paediatricians about congenital junctional ectopic tachycardia in neonates. Ivabradine is an option for the resistant congenital ectopic tachycardia.
Acknowledgements
Our study does not bear any conflict. There is not any honorarium, grant, or payment given to any author of this manuscript.
Financial support
There is no external financial support.
Competing interests
Authors declare that they do not have any competing interest.





