INTRODUCTION
Older adults (patients ages≥65) are the fastest growing subset of the population in the industrialized world.Reference Hall, DeFrances and Williams 1 Although this cohort contains 13% of the population, it accounts for 37% of hospital discharges and 43% of patient care days.Reference Hall, DeFrances and Williams 1 Although, on average, older adults cost the health care system more than younger cohorts, not every patient over the age of 65 strains these resources similarly.Reference Picco, Achilla and Abdin 2
Adults sustaining blunt chest trauma represent a specific example of this paradox; although from an epidemiologic perspective, older adults have a higher morbidity and mortality than younger cohorts,Reference Bulger, Arneson and Mock 3 - Reference Battle, Hutchings and Evans 5 not every older adult sustaining blunt chest trauma sustains an adverse event. This suggests that risk factors other than age are at play. Indeed, previous systematic reviews on older adults sustaining trauma have suggested that anti-coagulant use, hypotension, increased Injury Severity Score (ISS), and lower Glasgow Coma Score are risk factors for increased mortality.Reference Sammy, Lecky and Sutton 6 , Reference Hashmi, Ibrahim-Zada and Rhee 7
Prior reviews have examined risk factors for adverse outcomes in older patients sustaining blunt chest trauma.Reference Battle, Hutchings and Evans 5 , Reference Vana, Mayberry and Luchette 8 , Reference Aschkenasy and Rothenhaus 9 To our knowledge, there is only one systematic review in this area, which primarily examined mortality differences between older and younger cohortsReference Battle, Hutchings and Evans 5 and did not specifically consider patients ages 65 and older as a population (or subpopulation) of interest. Furthermore, prior reviews focused solely on morbidity and mortality and did not investigate other patient-centred outcomes (i.e., quality of life and loss of independence) or health care resource use (i.e., emergency department [ED] recidivism and hospital length of stay [LOS]).Reference Battle, Hutchings and Evans 5 , Reference Vana, Mayberry and Luchette 8 , Reference Aschkenasy and Rothenhaus 9 Thus, the goal of the present study was to systemically review the literature for risk factors related to these broader adverse outcomes in older adults who sustained blunt chest wall trauma.
METHODS
We adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)Reference Moher, Liberati and Tetzlaff 10 and the Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines in undertaking this review.Reference Stroup, Berlin and Morton 11
Search strategy
In collaboration with an expert librarian, a search strategy was developed to search EMBASE and MEDLINE (from inception to March 17, 2017). Search terms (medical subject, Emtree headings, and free text words) related to older adults and blunt chest trauma were used in addition to previously validated geriatric search filters with the goal of being as inclusionary as possible (see Appendices 1 and 2).Reference van de Glind, van Munster and Spijker 12 Because adverse events related to chest trauma are diverse, our search strategy was not limited to specific outcomes. In addition, bibliographies of all included studies were screened for potential inclusion in the review. No language restrictions were applied to the initial search strategy, but only abstracts written in English and French were considered for potential inclusion.
Study selection
Search results from EMBASE and MEDLINE were combined using Covidence software (available at www.covidence.org), and duplicates were excluded. Titles and abstracts were independently screened for potential relevance by two reviewers (JS, PD). Our population of interest was patients of age≥65 with blunt chest trauma, which we defined as blunt chest injury resulting in chest wall contusion or rib fractures, with or without immediate life-threatening injury to the lungs or other organ systems. Due to a relatively small number of eligible studies, we elected to include studies that attempted to identify a cohort of older adults sustaining blunt chest trauma, but for logistical reasons had to lower the minimum age for study inclusion. To decrease heterogeneity amongst included studies, studies were only included if the mean age of the study cohort was 65 years or older. Any disagreements were resolved by consensus. If consensus could not be reached, a third reviewer (BT) was consulted to adjudicate. Inter-rater reliability was measured using Cohen’s Kappa statistic.
Following the initial screening, a full-text review was performed by two reviewers (JS, PD). Clinical cohort studies were included if there was a longitudinal component investigating the relationship between prognostic factors and an outcome of interest. Studies were excluded if they 1) were a review article, case report, or case-series; 2) were conducted in a study population not meeting inclusion criteria (mean age of group or subgroup≥65, or patient population not sustaining blunt chest trauma as defined previously); 3) did not analyse risk factors for an outcome of interest; or 4) did not examine an outcome of interest (morbidity, mortality, LOS, ED recidivism, quality of life, or loss of independence).
Outcomes of interest
The primary outcomes of interest were morbidity, mortality, ED recidivism, LOS, quality of life, and loss of independence (defined as discharge to institution). Because morbidity in this patient population was expected to be heterogeneous, we examined any complications reported by study authors, including (but not limited to) pneumonia, intubation, and intensive care unit admission. Mortality was defined as in-hospital or 30-day mortality. Loss of independence implied that the patient was discharged to a higher level of community care than they were admitted from (i.e., transitional care, lodging, or nursing home admittance). ED recidivism was defined as repeat presentation to the ED within 30 days.
Prognostic factors
Prognostic factors for outcomes of interest were classified into three groups for synthesis and to improve clarity of presentation: patient factors, disease factors, and institutional factors. Patient factors included any underlying features, conditions, or demographic characteristics, which were present before the acute injury (e.g., patient age, sex, co-morbidities). Disease factors included any risk factors related to the traumatic event (e.g., multiple rib fractures, flail chest, associated trauma, mechanism of injury). Institutional factors included elements related to the ED admission/hospital admission (e.g., treatment by trauma team, treatment by multi-disciplinary team, adverse events).
Critical appraisal of included studies
Risk of bias (ROB) was assessed by two reviewers (JS, PD), using the Quality in Prognostic Studies (QUIPS) tool.Reference Hayden, Côté and Bombardier 13 The QUIPS tool examines ROB in six domains: study participation, study attrition, prognostic factor measurement, outcome measurement, study confounding, and statistical analysis and presentation. Inter-rater reliability was assessed using the Cohen’s Kappa statistic.
Data extraction
Data extraction was performed by two independent reviewers (JS, PD), using a piloted data extraction form. Where disagreement occurred, the paper was reviewed and the discrepant variable/value was clarified. Extracted information included study characteristics (i.e., type of study, number of patients, outcomes of interest), patient characteristics (i.e., age, sex, co-morbidities, ISS), and strength of association (i.e., odds ratios [OR] and relative risks) between prognostic factors and outcomes of interest. If relevant information was unclear or missing, up to three attempts were made to contact the primary author via email to obtain the pertinent information.
Data synthesis
We used descriptive statistics (means and percentages) to assess study characteristics and the reporting of risk factors. Because a meta-analysis was not performed, mean morbidity and mortality were calculated using a non-weighted average of reported means. Where appropriate, and when not reported, univariate OR and 95% confidence intervals were calculated by creating 2×2 contingency tables using MedCalc software. Data synthesis and meta-analysis of three or more studies examining the same predictor of an adverse outcome were planned using RevMan 5.3 software. Unfortunately, due to the paucity of studies satisfying selection criteria, as well as heterogeneity in how risk factors were measured, this was not possible.
RESULTS
Our initial search strategy produced 894 citations in EMBASE and 1,497 citations in MEDLINE (Figure 1). After excluding duplicates, a total of 2,297 studies underwent initial title and abstract screening; 187 studies were subjected to a full-text review. Thirteen studies met all eligibility criteria and were included in the final review. Overall, agreement on study inclusion was very good (k=0.790).
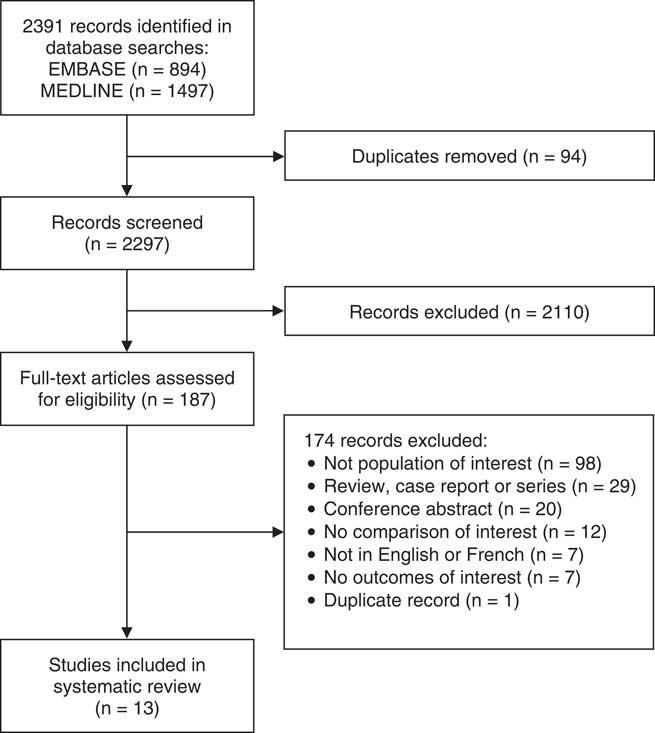
Figure 1 Selection of articles for inclusion.
Study characteristics
Table 1 summarizes the characteristics of the 13 included studies representing a total of 79,313 patients.Reference Alexander, Gutierrez and Mariano 14 - Reference Shulzhenko, Zens and Beems 26 Studies were published between 1985 and 2016; 11 studies were performed in the United States,Reference Alexander, Gutierrez and Mariano 14 - Reference Bansal, Conroy and Chang 17 , Reference Gonzalez, Ghneim and Kang 20 - Reference Shulzhenko, Zens and Beems 26 1 was performed in Egypt,Reference Elmistekawy and Hammad 19 and 1 was performed in Israel.Reference Barnea, Kashtan and Skornick 18 All 13 were retrospective cohort studies, with the majority using data from trauma registries. Study populations ranged in size from 38 to 67,659 patients. Overall mortality across studies was 8.4%, and the overall complication rate was 26.5%. Six studies included mortality as a primary outcome of interest.Reference Bansal, Conroy and Chang 17 - Reference Elmistekawy and Hammad 19 , Reference Harrington 21 , Reference Stawicki, Grossman and Hoey 25 , Reference Shulzhenko, Zens and Beems 26 Eight studies included morbidity as a primary outcome of interest.Reference Alexander, Gutierrez and Mariano 14 - Reference Bakhos, O’Connor and Kyriakides 16 , Reference Barnea, Kashtan and Skornick 18 - Reference Gonzalez, Ghneim and Kang 20 , Reference Kieninger, Bair and Bendick 22 , Reference Lotfipour, Kaku and Vaca 23 Six studies examined prognostic factors related to LOS.Reference Alexander, Gutierrez and Mariano 14 - Reference Bakhos, O’Connor and Kyriakides 16 , Reference Kieninger, Bair and Bendick 22 , Reference Sahr, Webb and Renner 24 - Reference Shulzhenko, Zens and Beems 26 One study examined prognostic factors related to discharge to an extended care facility.Reference Bakhos, O’Connor and Kyriakides 16 None of the studies explored risk factors for ED recidivism or patient quality of life.
Table 1 Study and patient characteristics

ISS=Injury Severity Score; L1TC=Level I trauma centre; L2TC=Level II trauma centre; LOS=length of stay; NR=not reported; TCC=tertiary care centre.
* Calculated value.
Quality assessment of included studies
Table 2 summarizes the ROB assessment for all included studies. Overall inter-rater agreement was excellent (k=0.803). Most studies were of low to moderate quality and at moderate to high ROB. The main issues with study quality were related to prognostic factor measurement, outcome measurement, study confounding, and statistical analysis. Nine studies were found to have moderate to high ROB due to incomplete reporting on how prognostic factors were measured.Reference Alexander, Gutierrez and Mariano 14 - Reference Elmistekawy and Hammad 19 , Reference Kieninger, Bair and Bendick 22 , Reference Sahr, Webb and Renner 24 , Reference Stawicki, Grossman and Hoey 25 Most studies were judged to have high ROB based on partial reporting of confounder measurements. Seven studies were of moderate to high ROB in relation to outcome measurement.Reference Alexander, Gutierrez and Mariano 14 - Reference Bakhos, O’Connor and Kyriakides 16 , Reference Elmistekawy and Hammad 19 , Reference Gonzalez, Ghneim and Kang 20 , Reference Sahr, Webb and Renner 24 , Reference Stawicki, Grossman and Hoey 25
Table 2 Risk of bias assessment using the Quality in Prognostic Studies tool

Prognostic factors associated with post-injury mortality
Prognostic factors associated with post-injury mortality are shown in Table 3. Three studies examined associations between patient factors and mortality. One study found an association between a history of congestive heart failure and mortality after adjusting for age, ISS, the need for intubation, and trauma centre volume.Reference Harrington 21 One study found a univariate association between ages≥80 and mortality,Reference Bansal, Conroy and Chang 17 whereas two others found a multivariate association between advanced age and mortality.Reference Harrington 21 , Reference Shulzhenko, Zens and Beems 26 The association between disease factors and mortality was examined in five studies. Univariate associations were reported for increasing number of ribs fracturedReference Barnea, Kashtan and Skornick 18 , Reference Stawicki, Grossman and Hoey 25 and development of pneumonia,Reference Elmistekawy and Hammad 19 whereas multivariate associations were reported for higher ISS,Reference Harrington 21 need for intubation,Reference Harrington 21 and having eight or more fractured ribs.Reference Shulzhenko, Zens and Beems 26 Only one study reported an association between mortality and an institutional factor. The authors reported a higher mortality in patients admitted to a Level I trauma centre after adjusting for age, ISS, need for intubation, and pre-existing congestive heart failure.Reference Harrington 21 Although three studies examined ageReference Bansal, Conroy and Chang 17 , Reference Harrington 21 , Reference Shulzhenko, Zens and Beems 26 and rib fracturesReference Barnea, Kashtan and Skornick 18 , Reference Stawicki, Grossman and Hoey 25 , Reference Shulzhenko, Zens and Beems 26 as risks for mortality, meta-analysis was felt to be inappropriate due to heterogeneity in how these variables were measured.
Table 3 Prognostic factors associated with post-injury mortality

CHF=congestive heart failure; ISS=Injury Severity Score; L1TC=Level I trauma centre.
* Data are presented as odds ratios with 95% confidence intervals and p values (if available).
† Univariate association using chi-square test was reported.
‡ Calculated odds ratio and 95% confidence interval.
Prognostic factors associated with post-injury morbidity
Patient, disease, and institutional factors associated with post-injury morbidity are summarized in Table 4. Six patient factors were investigated across studies. Univariate associations were reported for the presence of cardiopulmonary diseaseReference Alexander, Gutierrez and Mariano 14 and diabetes mellitus,Reference Barnea, Kashtan and Skornick 18 , Reference Elmistekawy and Hammad 19 whereas multivariate associations were reported for age,Reference Shulzhenko, Zens and Beems 26 chronic obstructive pulmonary disease (COPD),Reference Gonzalez, Ghneim and Kang 20 protein calorie malnutrition,Reference Gonzalez, Ghneim and Kang 20 and ambulatory assist devices.Reference Gonzalez, Ghneim and Kang 20
Table 4 Prognostic factors associated with post-injury morbidity

CD=cardiopulmonary disease; COPD=chronic obstructive pulmonary disease; ISS=Injury Severity Score; IV=intravenous; MV=mechanical ventilation; OR=odds ratio.
* Data are presented as odds ratios with 95% confidence intervals and p values (if available).
† Calculated odds ratio and 95% confidence interval.
‡ Univariate association using student’s t-test was reported.
§ Univariate association using chi-square test was reported.
There were six disease factors associated with post-injury morbidity examined across included studies. Univariate associations were reported for the need for early mechanical ventilation,Reference Allen and Schwab 15 oxygen saturation,Reference Barnea, Kashtan and Skornick 18 and number of rib fractures,Reference Barnea, Kashtan and Skornick 18 , Reference Elmistekawy and Hammad 19 whereas multivariate associations were reported for the need of tube thoracostomy,Reference Gonzalez, Ghneim and Kang 20 increasing ISS,Reference Gonzalez, Ghneim and Kang 20 per one increase in number of ribs fractured,Reference Gonzalez, Ghneim and Kang 20 or having eight or more ribs fractured.Reference Shulzhenko, Zens and Beems 26
Only one institutional factor was investigated in relation to post-injury morbidity. The authors reported higher morbidity in patients receiving epidural rather than intravenous (IV) analgesia after adjusting for ISS and the presence of pre-existing cardiopulmonary disease.Reference Kieninger, Bair and Bendick 22 Although three studies examined rib fractures as a risk factor for pneumonia, meta-analysis was felt to be inappropriate due to heterogeneity in how the risk factor and outcome variable were measured.Reference Elmistekawy and Hammad 19 , Reference Gonzalez, Ghneim and Kang 20 , Reference Shulzhenko, Zens and Beems 26
Prognostic factors associated with length of stay
The patient, disease, and institutional factors associated with LOS are summarized in Table 5. A total of three patient factors were investigated across studies, suggesting univariate associations between in-hospital LOS and the presence of cardiopulmonary disease,Reference Alexander, Gutierrez and Mariano 14 vital capacity,Reference Bakhos, O’Connor and Kyriakides 16 and percentage of predicted vital capacity.Reference Bakhos, O’Connor and Kyriakides 16
Table 5 Prognostic factors associated with hospital length of stay (LOS)

CD=cardiopulmonary disease; IV=intravenous.
* Data are presented as mean LOS and p values (if available).
† p-values from linear regression analysis were reported.
‡ p-values from analysis of variance analysis were reported.
Two disease factors were investigated across studies, and reported associations included the number of ribs fractured (univariate),Reference Bakhos, O’Connor and Kyriakides 16 , Reference Stawicki, Grossman and Hoey 25 having 5 or more ribs fractured (multivariate, adjusting for 23 patient and hospital factors),Reference Shulzhenko, Zens and Beems 26 and the need for mechanical ventilation (univariate).Reference Allen and Schwab 15
There were two institutional factors analysed across studies. Kieninger et al. reported increased LOS in patients receiving epidural rather than IV analgesia after adjusting for ISS and pre-existing cardiopulmonary disease,Reference Kieninger, Bair and Bendick 22 whereas Sahr et al. reported an unadjusted decreased LOS in rib fracture patients receiving protocolized care.Reference Sahr, Webb and Renner 24
Prognostic factors associated with discharge to an institution
Only one study examined the association between prognostic factors and discharge to an institution.Reference Bakhos, O’Connor and Kyriakides 16 This study showed that patients discharged to an extended care facility had lower mean vital capacities (within 48 hours of admission) than those discharged to home (0.9±0.4 L v. 1.3±0.5 L; p=0.025).
DISCUSSION
As the population continues to age, the care of geriatric patients is receiving more attention as older adults have proportionally higher rates of adverse events than younger cohorts.Reference Bulger, Arneson and Mock 3 , Reference Latham and Ackroyd-Stolarz 27 Older adults may differ from other patients in a variety of ways, including the number of (and severity of) co-morbid conditions, post-injury problems that can arise, and the extent of treatment offered to them. Further, the fast-paced, goal-oriented environment of the ED is not always conducive to the treatment of older patients who often have more acute, complex, or atypical presentations of illness,Reference Kahn, Magauran and Olshaker 28 highlighting a need for behavioural or system change.
This is the first systematic review to specifically examine risk factors for adverse outcomes among older adults with blunt chest wall trauma. We identified 13 studies, which reported on 26 risk factors for adverse outcome in older adults sustaining blunt chest trauma. There was significant variation in risk factor and outcome measurement across studies, and, with the exception of age and rib fractures reported, associations were limited to one or two studies. Therefore, a meta-analysis could not be performed. Of note, most studies focused on finding novel associations using small datasets rather than building on previous research. Indeed, only six of the included studies used multivariate analysis techniques, potentially inflating the relative strength of associations because confounders were not controlled for.Reference Barnea, Kashtan and Skornick 18 - Reference Kieninger, Bair and Bendick 22 , Reference Shulzhenko, Zens and Beems 26 Lastly, all included studies used phase one (identifying associations) methodology,Reference Hayden, Côté and Steenstra 29 and only one study considered the potential for prognostication.Reference Lotfipour, Kaku and Vaca 23
A previous systematic review examining risk factors for mortality in blunt chest trauma patients ages≥18 suggested that ages>65, three or more rib fractures, pre-existing cardiopulmonary disease, as well as the development of pneumonia were associated with mortality.Reference Battle, Hutchings and Evans 5 Our study suggests that, in older adults, additional disease factors may be at play, including higher ISS and the need for intubation. While these outcomes are unlikely to be modifiable, they may be potentially useful in prognostic models as well as in guiding goals of care. Of interest, Harrington et al. reported that patients admitted to Level I trauma centres tended to have higher mortality rates than those admitted to Level II trauma centres on a multivariate analysis.Reference Harrington 21 This suggests a need for further research because unmeasured markers of trauma burden are likely to be at play.Reference Harrington 21
Earlier reviews have suggested that an increasing number of rib fractures are associated with pulmonary complications in patients sustaining blunt chest wall trauma.Reference Vana, Mayberry and Luchette 8 , Reference Aschkenasy and Rothenhaus 9 Our review is the first to systematically examine risk factors for morbidity in older adults sustaining chest trauma and identify 10 potential patient and disease factors for morbidity. Again, none of these are likely to be modifiable; but, with additional study, they could be incorporated into prognostic models to help guide care. Of note, Kieninger et al. reported an increase in complication rate associated with the use of epidural over IV analgesiaReference Kieninger, Bair and Bendick 22 and noted that this association persisted when ISS and cardiopulmonary co-morbidities were accounted for. The study was retrospective with the choice of analgesia left up to the care team, and it is possible that unmeasured markers of trauma burden were apparent to the care team but could not be measured. However, it does highlight that institutional factors can affect patient outcome; further study in this area is warranted.
As the population ages, the rising demand on the health care system is becoming increasingly concerning. One of the current rate limiters in emergency care is inpatient LOS because it has a trickle-down effect on ED flow.Reference Schiff 30 Although pre-existing conditions and markers of trauma burden are unlikely to be modified, two studies suggested potential modifiable risk factors that could improve patient care and contribute to decreased LOS.Reference Kieninger, Bair and Bendick 22 , Reference Sahr, Webb and Renner 24 Due to the retrospective design of the Kieninger et al. study, it is difficult to judge the impact of IV over epidural analgesia on LOS; but promisingly, Sahr et al. showed that the use of a protocolized care plan in patients over age 65 can reduce LOS.Reference Sahr, Webb and Renner 24 Further study is needed to assess the external validity of these findings, as well as their potential impact on health care costs.
Only one study assessed prognostic factors associated with loss of independence, and no studies examined quality of life or ED recidivism, identifying an important gap in the literature. Given that many older patients consider quality of life to be more valuable than duration of life,Reference Cohen-Mansfield, Droge and Billig 31 , Reference Lee 32 additional research is needed to investigate patient-centred outcomes related to quality of life such as ED recidivism and discharge to a continuing care institution.
This study had several limitations. Firstly, all systematic reviews are limited by the inclusiveness of their search strategy. To minimize the potential for missing studies of interest, we used an expert librarian to develop our search strategy and attempted to make it as sensitive as possible. Further, we hand-searched the references of included studies to minimize the chance that an important study was missed. Secondly, we were limited by the quality of included studies. Over half of the included studies did not include a multivariate analysis, making it difficult to interpret the relative strength of associations across studies. Thirdly, five studies did not specifically examine patients ages 65 years and older, and the inclusion of younger patients in the study cohorts has the potential to weaken the strength of associations. We opted to include these studies for two reasons: 1) historically, the definition of older adults has changed over time, and there may have been a good reason to study a slightly younger cohort at the time of the initial study; and 2) due to the relatively small number of included studies, we felt it was important to highlight the findings of prior researchers to aid future research in this area.
A fourth limitation of the current study was the significant heterogeneity in the trauma burden of patients among included studies. The mean ISS of included studies ranged significantly (from 6.9 to 19.4). Further, four studies did not report ISS, and several studies did not adjust for injury severity. Lastly, the definition of morbidity varied across studies, making it difficult to assess the severity of complications. For example, complications such as pleural effusion, pneumonia, and intubation were not necessarily reported separately. This highlights the need for clearer definitions of complication severity in future studies.
CONCLUSION
Our findings indicate that there is limited high-quality evidence available in the literature on risk factors for adverse outcomes in elderly patients with blunt chest wall trauma. Currently, there are no established models that can help in predicting adverse outcomes in this specific group. Given the aging population and the likely future increase in ED presentations of older aged patients, additional high quality studies are indicated.
Acknowledgements
We would like to thank Melissa Helwig from Dalhousie University for her assistance in developing our search strategy. This study was supported by the College of Medicine, University of Saskatchewan, Saskatoon, SK.
Competing interests: None declared.
SUPPLEMENTARY MATERIAL
To view supplementary material for this article, please visit https://doi.org/10.1017/cem.2017.377








